Eamonn Brady MPSI and Siobhan Clarke MPSI look at the physiological and psychological issues that are likely to arise when children return to school in the aftermath of Covid-19
As you are aware, 2020 has been filled with uncertainty, with concerns schools will not return as normal in September 2020, and with young people and children having been home for six months. Returning to school can always be stressful after time off, but this significant amount of time might affect them differently, so it must be dealt with carefully.
There will be physical changes in schools regarding class layout to facilitate physical distancing and other hygiene standards. These changes can lead to anxiety and stress for parents and children, so effective communication between everyone will be an absolute necessity.
Other than Covid-19 changes in these unprecedented times, young people and children’s mental and physical health are a top priority all-year-round, especially upon their return to school. In this article, we will discuss this, as well as common childhood conditions.
Tips
Tackling back-to-school anxiety
Feeling anxious is completely normal for children, teens and parents when returning to school and/or starting a new school. Feeling anxious is the mind and body’s natural reaction to stress and fear, ie, ‘fight or flight’ — it is essentially the fear of the unknown. Symptoms may include restlessness, nervousness, feelings of danger, panic and stomach upset. These feelings of anxiety only become a problem if these fears become overwhelming or unmanageable. This can be an anxiety disorder.
Within days of returning to school, an anxious child may be clingy, angry, complain of stomach pains and headaches, or be quiet and emotional.
As well as Covid-19 worries, children and young people have different worries relating to school, such as teachers, being away from their parents, friends, and fitting-in. If a child does not go to school because of these feelings, they cannot find out if their fears are irrational or not. If a child is excessively complaining of prolonged headaches, tummy complaints and other symptoms of anxiety, they may need a medical assessment. Don’t rule out other underlying conditions if these complaints are a constant.
Getting children into a school sleep routine before school starts can also reduce the amount of anxiety and stress they may be feeling.
Tip 1: Listen
Simply listening to a child’s fears about returning can make a child feel more at ease and secure. It will give him/her confidence in dealing with these thoughts about difficult times. Dismissing fears, ie, ‘you’ll be fine, there’s nothing to worry about’ generally will not help. Children often want to talk about worries without a parent ‘fixing’ them. They usually seek validation and confidence from a parent or guardian.
Tip 2: The basics
Children can cope better with everything if they are getting enough sleep, eating regular, healthy meals and snacks and getting daily exercise. A healthy body can mean a healthy mind.
Tip 3: Action plan
Worried teens and children may have scattered thoughts, so making coping methods for them can be helpful, for example, asking them ways in which they can react in a situation that is bothering them. A plan will help them to distinguish between rational or irrational situations (real and imaginary scenes in their heads).
Tip 4: Positivity
Everyone needs positivity. Once these fears are addressed and coping methods are in order, there is no need to dwell on them. Focusing on the positives of school can help to alleviate your child’s anxiety, ie, ‘What are you excited about on your first day?’ Fun aspects of school can become obscured by worries.
Tip 5: Parent behaviour
It is daunting for parents leaving their children at a new school for their first day. Children can see the stress and anxiety their parent displays. The calmer and more confident you are, the easier it will be for the child. It is important to be supportive, but also firm. Sharing your own anxieties with a child might not be a great decision if the child is anxious.
NUTRITION
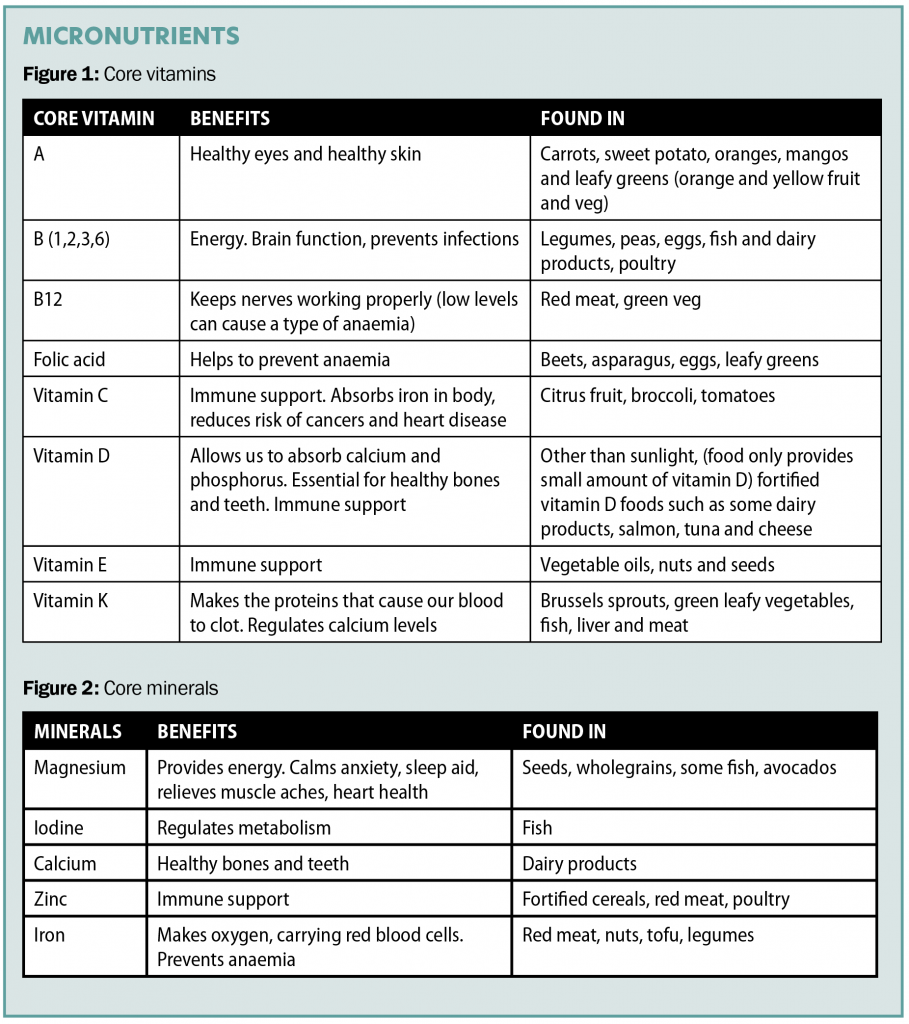
Different nutrients are needed for a balanced diet. Nutrients are made up of macronutrients (big), which are essentially carbohydrates, fats and proteins; and micronutrients (small), which are vitamins and minerals. Different foods have different micronutrients and macronutrients.
Water
Staying hydrated is important to ensure all our nutrients are absorbed properly. Dehydration causes fatigue and lack of concentration. We should aim to drink about six-to-eight glasses of water per day to stop us getting dehydrated. Water can also be obtained through diet, ie, soups.

Lunch
School lunches should be nutritionally balanced; they should include at least three food groups (fruit, vegetables, grains, protein and dairy/calcium-rich foods). Unhealthy lunch habits decrease brain power and can cause memory loss. Foods high in saturated fat, sugar and salt should be kept to a minimum. Many children experience fatigue after lunch. High-protein lunches appear to produce greater alertness and more focused attention.
Fruit and vegetables
Fruit and vegetables are packed with different vitamins and minerals (micro), which are all essential in different ways (see Figures 1 & 2). Fruit and vegetables are also a good source of dietary fibre, which is important for digestive health and regulates bowl movements. Including more fruit and vegetables as part of a balanced diet will help children grow and develop, improve vitality and help prevent a range of chronic diseases such as type 2 diabetes, heart disease, high blood pressure and cancer in later life. It can be difficult to get some kids to eat the recommended ‘five a day’ of fruit and veg. Research has shown that the more fruit and vegetables that are available and easily accessible for children, the more likely they are to eat them. Therefore, if fruit is chopped-up and ready to eat, children will eat more of them. Providing a variety of different fruits and vegetables is one way to encourage children towards healthy eating habits, however parents must be patient. There is some evidence that children need to try new fruits and vegetables up to eight or nine times before they are liked or accepted. Being creative in the way you serve fruit and vegetables can help. For example, prepare vegetables in different ways to vary the texture, such as raw, microwaved, mashed, baked, and grated into a casserole, blended up as a pasta sauce or as a soup.
Carbohydrates
Carbohydrates are made up of sugars and are for energy. Refined sugars include sweets, cakes, etc. They have no nutritional benefits and should only be consumed sparingly, as they can cause serious health problems for adults and children, including tooth decay, diabetes and heart disease. Wholegrain carbohydrates are the more nutritious option as opposed to wheat, ie, white bread. Wholegrains contain soluble fibre, vitamin, iron, copper, zinc, magnesium and antioxidants.
Protein
Proteins are made up of essential and non-essential amino acids. Non-essential amino acids are already made in the body, so we do not need them from our diet; on the other hand, essential amino acids are the proteins we need to ingest. All these proteins (amino acids) help each other for the growth and repair of the body’s cells. Children need about 20-to-35 grams of protein in a day, depending on weight, age and gender, ie, a tablespoon of peanut butter is about 5gs protein and a palmed-sized portion of meat is about 20 grams. Other examples of foods high in protein are eggs, cheese, nuts, seeds and poultry, etc.
Fish: Fish oil is recommended for a healthy diet because it contains the omega-3 fatty acids eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA). EPA aids emotional health and reduces stress levels, while DHA aids memory and concentration, therefore they are essential for children. Children should eat at least two portions a week of fish; one of the weekly portions (140g) should be oily fish, ie, salmon, mackerel.
Fats
Fats can either be saturated or unsaturated. Unsaturated are ‘good’ fats (nuts and seeds), while saturated are considered ‘bad’, ie, butter and fatty meat like sausages. Small amounts of fat are essential for body insulation but too much can lead to obesity and other serious health conditions later in life.
High-fat diets for children tend to lead to greater fatigue, sleepiness and distraction. Chicken, tuna, lean beef and eggs are examples of healthy options that are high in protein and low in fat.

Exercise
It is important for children and young people to get enough exercise for their mental and physical health. Kids and teens should get one hour or more of moderate-to-vigorous activity daily. Exercise can improve their social skills, self-esteem, academic scores and concentration and builds a stronger heart and bones.
Common conditions
Head lice
Head lice is common as children return to school. The lice are small insects that feed on blood obtained by biting the scalp. These bites tend to be itchy and this itchiness is caused by an allergy to the lice. Head lice are transferred by close hair-to-hair contact. They cannot jump, fly or swim, but walk from one hair to another. It is a misconception that head lice infestation is as a result of dirty hair and poor hygiene. Head lice can be found in all hair types, long or short, and in hair of any condition.

Prevention
There is no way of guaranteeing your child won’t get head lice but checking yours and your family’s hair and scalp regularly is important. If your child has long hair, tie it back, as this helps to reduce the likelihood of contact between their hair and that of an infected child.
Treatment
There are many products to treat head lice, some of which include:
1. Hedrin Once Spray Gel and Shampoo.
2. Full Marks Solution.
3. Lyclear products.
If you do not wish to use chemicals, wet-combing is another method of removing head lice. Nit combs are used for wet-combing. The steps to follow for wet-combing are to wash the hair as normal using an ordinary shampoo, apply conditioner liberally to wet hair (this causes lice to lose their grip on hair), and comb the hair through with a normal comb first. Then with a fine-tooth nit comb, comb from the roots along the complete length of the hair and after each stroke, check the comb for lice and wipe it clean. Work methodically over the whole head for at least 30 minutes. Rinse the hair as normal. Repeat every three days for at least two weeks.
Threadworm
Threadworms are tiny parasites that infect the large intestine. They are mostly common in children under the age of 10. A common symptom includes intense itching around the anus, especially at night. If you suspect a child has threadworms, the entire family should be treated, as sometimes they can be asymptomatic.
Prevention
Threadworms are usually passed on through poor hygiene. The female worms lay eggs around the anus. When a child scratches, the threadworms can be transferred from their fingers to their mouth and different surfaces. If another person touches these contaminated surfaces and then their mouth, they become infected with threadworms. Therefore, the prevention of threadworms includes keeping a high standard of hygiene, ie, frequent hand-washing and avoid scratching the area.
Treatment
Hygiene method: This can be used to stop the threadworm infection. These methods should be followed for six weeks. Everyone in the house must strictly follow the methods. Some of these methods include: Wash all bed linen and clothes; thoroughly vacuum and dust the house; disinfect bathrooms and kitchen; keep fingernails short; no nail-biting; wash hands frequently; clean toothbrushes thoroughly before use; shower regularly; and avoid towel-sharing.
Medication: There is a 75 per cent chance that everyone in the family will be infected with threadworms if one person has them.
The most common medications are mebendazole and piperazine. Mebendazole (Vermox) is the preferred treatment for those over two years of age. It prevents the threadworms from absorbing glucose. It kills the worms in the gut, but not the eggs that have been laid around the anus. These can stay on underwear and bed linen, so it is important to have good hygiene standards in the house.
Re-infection can be common, so another dose can be common after two weeks of the initial treatment.
Conjunctivitis
Conjunctivitis is when the eyes become inflamed, more commonly from a virus than bacteria. Symptoms usually clear-up within two weeks. The main symptom to look out for is red or pink eyes, green discharge, or swollen and itchy eyes. If there is pain and both eyes are red for more than two days, it may be a bacterial infection and the child needs to see his/her GP. If the child has sticky eyes for two weeks, they also need to see their GP.
Prevention
Both viral (most common) and bacterial conjunctivitis are highly contagious, so good hygiene standards can prevent the contamination and spread of conjunctivitis. Make sure they wash their hands often, don’t let them rub their eyes (if they do, wash their hands after touching their eyes), don’t share pillows and towels.
Treatment
Viral conjunctivitis: There is no medication to treat a viral infection. There are ways to ease their discomfort, which include: 1) Wash your hands; 2) wet a cotton ball or pad with cooled boiled water; and 3) wipe the child’s eye from the inner to outer corner. Make sure to use a different cotton ball or pad each time; 4) dry the eyes using a different cotton ball or pad; and 5) wash hands.
Bacterial conjunctivitis: The doctor may prescribe antibiotic eye drops and a pharmacist can advise on OTC options and when referral to a GP is required.
The HSE has stated that there is no reason for a child to be out of school because of viral conjunctivitis, unless they feel sick, and the childcare provider should be advised if a child has conjunctivitis.
Disclaimer: Brands mentioned in this article are meant as examples only and not meant as preference to other brands.
References on request.
Written by Siobhan Clarke (Pharmacy Technician) and Eamonn Brady (Pharmacist). Whelehans Pharmacies, 38 Pearse St and Clonmore, Mullingar. Tel 04493 34591 (Pearse St) or 04493 10266 (Clonmore). www.whelehans.ie







