The pharmacist has a major role to play in providing much-needed advice to parents on their baby’s nutritional needs amid a confusing array of conflicting information
Caring for an infant’s nutritional needs can be a challenging time for parents and carers, particularly if it is their first child, and accessing conflicting information online can further confuse those taking care of an infant, particularly if there is a lack of family or peer support available to them. In this regard, in common with a range of other healthcare areas, the role of the pharmacist in providing advice and support has become increasingly important in offering guidance on early-life nutrition to parents who are often bombarded with sometimes-contradictory information.
While there are some circumstances in which breast milk may not be suitable for an infant, it is widely accepted that breastfeeding an infant provides them with the best start in life. A number of studies have shown that breast milk provides a baby with the optimal start in life and confers benefits such as reducing the risk of diarrhoea, respiratory and urinary tract infections, otitis media, and necrotising enterocolitis, among others.1
There have, however, been some controversies around breastfeeding versus formula feeding, with one Finnish study, for example, suggesting that there was a significant improvement in the symptoms of atopic eczema after cessation of breastfeeding and initiation of an amino acid formula.2
However, overall, there are a limited number of scenarios in developed countries in which breastfeeding may be contraindicated and these include if the mother has untreated tuberculosis, if the infant has galactosaemia, or if the mother is infected with the human immunodeficiency virus. Other barriers to breastfeeding include tender and painful nipples; tiredness and lack of available time; insufficient milk; and embarrassment or inconvenience.
Blocked ducts or engorgement, along with mastitis or thrush, may also discourage the mother from breastfeeding and in some circumstances, baby may simply be unhappy with the breast milk. In these circumstances, support for mother becomes even more important to help them overcome these obstacles.1
While it is down to the mother to decide when to stop breastfeeding, it is advised that breastfeeding is not discontinued abruptly…
Discontinuation
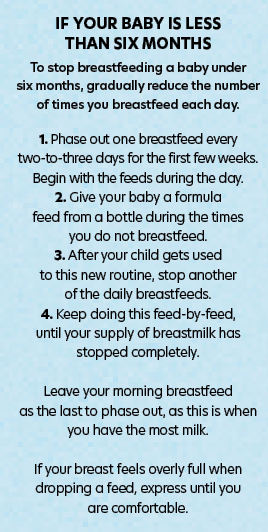
While it is down to the mother to decide when to stop breastfeeding, it is advised that breastfeeding is not discontinued abruptly, as this may lead to complications such as mastitis or blocked ducts, as well as an uncomfortable feeling of fullness for the mother. The HSE advises that when gradually phasing-out breastfeeding, a mother can choose to use a combination of breast milk and formula milk to help the process to happen more smoothly for mother and baby.3
The Executive issued guidance contained in Figure 1 to help guide mothers through the process when they decide to discontinue breastfeeding. As well as advice on the best formula for their baby, parents and carers also need to be counselled on the proper preparation and storage of formula feeds for infants. The Food Safety Authority of Ireland (FSAI) recommends that if an infant is not being breastfed, a standard first infant formula should be used throughout the first year of life and parents/carers should be made aware of the equipment that is required, such as sterilisers, caps, tongs, teats, etc.
Pharmacists can also help parents/carers to select the most appropriate formula milk for their baby, as there is a potentially confusing array of types available, including:4
- Standard infant formula milks: Labelled ‘from birth to newborn’, these milks are suitable for infants from birth to 12 months old and are whey-based. These are the most commonly-recommended milks for babies who are not being breastfed.
- ‘For hungrier babies’ milks: These feeds contain more casein protein than standard formula milks. Parents/carers can be advised that while these may make baby feel more full, they do not actually contain any more nutrients or calories than standard feeds.
- Specialised milks: These include lactose-free formulae, pre-thickened formulae (if regurgitation is a problem), hydrolysed or hypo-allergenic formulae, post-hospital discharge formulae, and follow-on formulae, which contain more iron and protein than other formulae and cow’s milk.
It is important that parents and carers are advised that any suspected allergies are diagnosed by the appropriate healthcare professional and while pre-thickened formulae may help with regurgitation issues, this may simply be down to over-feeding and in these cases, they should be advised to try feeding with smaller volumes more frequently and be sure to burp the baby after each feed.4
The FSAI added that soya-based formulae should not be given to infants under six months old and is not hypoallergenic, and should only be used under medical supervision. Similarly, goat’s milk is not recommended for any infant under 12 months of age, is not considered hypoallergenic, and is not a suitable source of nutrition for infant formulae or follow-on formulae.4
The FSAI and HSE provide detailed information for parents and carers on the correct preparation procedures for a feed, including sterilisation, bottle assembly, using the correct water and preparing feeds, etc. However, if the pharmacist suspects that the parent or carer may have literacy issues, it may be advisable to explain these procedures verbally.
Choices and volumes
Some of the more popular formulae in Ireland for babies aged from birth to 12 months include: Aptamil Organic Follow on Milk 800g; SMA Advanced Follow-On Milk 800g; Cow & Gate 1 First Infant Milk Formula 800g and Cow & Gate 2 Follow-On Baby Milk Formula 200ml; SMA Pro Follow-On Milk 6 Mth+ 800g; HiPP Organic 1 First Infant Baby Milk Powder from birth 800g; Aptamil 1 First Baby Milk Formula From Birth 1L and Aptamil 2 Follow On Baby Milk Formula 1L; and Cow & Gate Comfort Baby Milk Formula From Birth 800g.
This is a small sample of some of the formulae available for pharmacists to recommend and a full list is beyond the scope of this article, however the pharmacist should familiarise themselves with the characteristics of each and how they would be best suited to a particular infant’s needs.
The HSE provides general guidance on the volumes to use when feeding formula to infants (see Figure 2). However, the Executive stresses that it is a general guide only and if parents or carers are in any doubt about feed volumes, they should consult a healthcare professional for more detailed recommendations tailored to their individual circumstances.
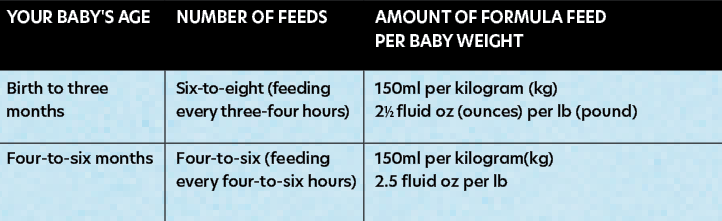
The HSE also cautions parents and carers to never re-use leftover milk once the baby finishes feeding.
It is therefore understandable that parents and carers can be overwhelmed by the range of choices available and sources of information, which emphasises the need for pharmacist intervention to provide clarity and reassurance. In a US study designed to address this issue, the authors concluded:
“With an extensive array of infant formulas available, pharmacists and caregivers can be overwhelmed when selecting an appropriate product. However, with careful questioning and a basic knowledge of the available formulas, an initial selection can be provided to caregivers. In addition to assisting in infant formula selection, pharmacists should provide information on proper preparation, handling, and storage of the product.”5
A separate Australian study was one of several to examine the issue of how infant nutrition influences the potential for overweight and obesity in later life for the infant. The authors suggest that certain modifiable practises may put children at a higher risk for overweight and obesity in later life and they emphasised the importance of a greater focus on how parents use infant formulae and their feeding practises. In this regard, the authors also noted that parents expressed a lack of support and resources to help guide them through this important phase of the infant’s life.
They concluded: “Additional support for parents’ feeding their infants with formula is necessary. Health professionals and policy around infant formula use should include how formula information may be provided to parents who use formula in ways that do not undermine breastfeeding promotion. Further observational research should seek to understand the interaction between advice, interpretation of cues and the amount formula fed to infants.”6
Pharmacists’ role
In both the community and hospital settings, pharmacists have an increasingly important role to play in providing evidence-based advice to parents and carers with regard to infant nutrition. The role in which pharmacists can have the greatest influence includes to:
- Promote and support breastfeeding with enthusiasm. Use appropriate opportunities to provide breastfeeding education to children and adults. Encourage family and societal support for breastfeeding.
- Collaborate with health professional colleagues (in both primary and secondary care) to make sure that women obtain adequate information throughout pregnancy to make an informed choice about feeding.
- Encourage hospital policies that facilitate breastfeeding.
- Familiarise yourself with local breastfeeding resources and support networks.
- Collaborate with health professional colleagues to ensure consistency in education for parents and carers and support for both mothers and infants.
- Be prepared to refer mothers with breastfeeding problems. Do not assume that provision of an infant formula is the best solution.
- In bottle-fed infants, advise on appropriate choice and correct use of formulae.
- Advise on appropriate choice of foods and drinks in weaned infants.
- Advise on vitamin supplementation. Vitamin drops containing vitamins A, C and D are advisable for most children between the ages of six months and five years.1
- Infant milk – an update. The Pharmaceutical Journal, Vol 264 No 7089p471-475.
- Isolauri E, Tahvanainen A, Peltola T, Arvola T. Breast feeding of allergic infants. Pediatrics 1999;134:27-32.
- Stopping Breastfeeding. HSE, https://www2.hse.ie/wellbeing/child-health/stopping-breastfeeding.html. Accessed Jan 2021.
- FSAI, Best Practice for Infant Feeding in Ireland 2012, accessed online Jan 2021.
- Pharmacists’ guide to infant formulas for term infants. J Am Pharm Assoc (2003), May-Jun 2011;51(3):e28-35; quiz e36-7, doi: 10.1331/JAPhA.2011.09125.
- Infant formula feeding practices and the role of advice and support: an exploratory qualitative study. BMC Pediatrics volume 18, Article number: 12 (2018).