Pain is defined by the International Association for the Study of Pain as “an unpleasant sensory and emotional experience, associated with actual or potential tissue damage, or described in terms of such damage”. Pain may also occur in the absence of tissue damage or any identifiable pathophysiological cause. Pain can be considered more than just a symptom of disease and is sometimes classed as a disease state in itself. Pain is universal, however pain perception varies and is affected by the likes of cultural backgrounds and genetic differences.
The 2006 National Disability Survey Ireland (CSO, 2008) stated that pain was one of the most common disability types reported. Almost 50 per cent of individuals reported pain as the main cause of their disability and, of those, 34 per cent indicated arthritis as being the most common cause of injury or illness. Almost 20 per cent stated the pain disability was caused by an accident or injury.
For this article, I will discuss the types of acute pain often seen in pharmacy and GP settings. The management of acute pain from severe trauma (eg, RTAs) that requires management with the likes of opioids and sedation in hospital settings is outside the scope of this article.
With chronic pain it can be more difficult to determine the cause; whereas with acute pain it has a more clearly identifiable cause, for example, muscle injury
Causes of pain
The cause of pain is sometimes difficult to determine and there are often many aspects to consider. With chronic pain it can be more difficult to determine the cause; whereas with acute pain it has a more clearly identifiable cause, for example, muscle injury. It is the indeterminate nature that can present the biggest obstacle to health professionals as they attempt to establish proper diagnosis of the condition.
The infographic below on ‘Reported Cause of Pain’ from the PRIME study, NUIG 2011, illustrates the problem further:
- General classification of pain (both acute and chronic):
Acute pain
Acute pain starts quickly and lasts a short period of time. The definition of acute pain is pain that improves within one to three months of onset. Pain that lasts longer than six months is considered chronic pain and will require more specialist treatment from a pain expert. The period between three and six months is classified as the time of transition from acute pain to chronic pain. Patients require more specialist evaluation and treatment at this stage rather than just taking painkillers to avoid transitioning into chronic pain.
Common examples of acute pain:
- Headaches;
- Sprains and strains;
- Dental work;
- Surgery;
- Broken bones;
- Burns or cuts;
- Childbirth.
Acute pain can be difficult to diagnose and treat, especially when caused by injuries that are not visually evident like a fractured rib, a herniated disc, a pinched nerve. Pain can develop to be more than a physical sensation. For example, it can develop to become an emotional problem such as fear, or anxiety related to a traumatic event that triggered the pain. For example, a person may avoid driving after suffering severe injuries in a car accident.
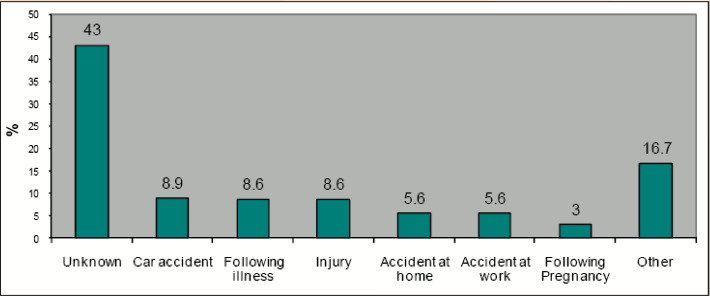
Figure 1: ‘Reported Cause of Pain’ from the PRIME study
Reasons for acute pain
Most acute pain episodes arise from causes that can be categorised as a musculoskeletal condition.
Pain is a sensation experienced through the nervous system (nerves, spinal cord, and brain). Reflexes are the nervous system’s immediate response to acute pain. This is demonstrated by when a hot plate is touched, it takes milliseconds for the nervous system and muscles to coordinate and make the hand move away immediately, ie a reflex reaction.
In addition to reflexes, the nervous system has more sophisticated mechanisms for processing pain. The brain releases neurotransmitters that influence pain levels and have an influence on mood which is one of the reasons why depression can occur in response to pain. Pain and depression can create a vicious cycle in which pain worsens the symptoms of depression and then the resulting depression worsens feelings of pain.
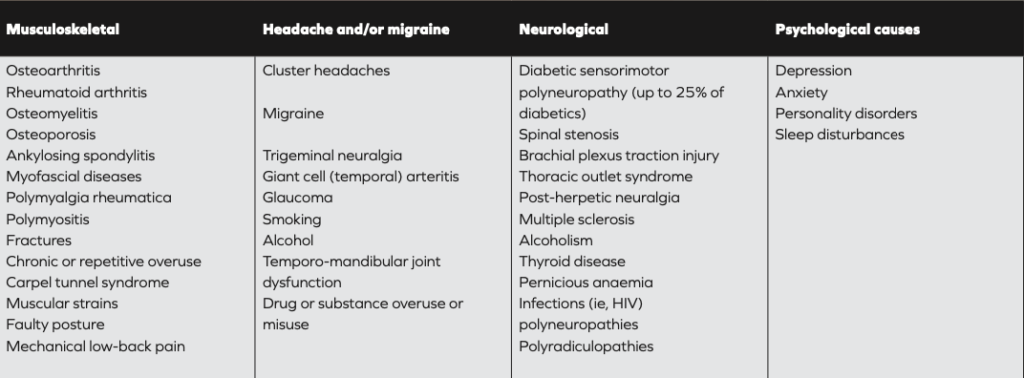
General classification of pain (both acute and chronic):
Symptoms
Acute pain can be felt in a specific body area such as the neck or back or the patient may have widespread pain with conditions such as a viral illness.
Acute pain may be described as:
- Sharp;
- Dull;
- Stabbing;
- Throbbing (sign of inflammation);
- Shooting or shock-like (sign of nerve involvement).
Diagnosis
The reason for the pain may not be visually obvious. Diagnostic tests are helpful and include:
- Blood tests;
- Imaging studies (X-ray, CT, MRI, nuclear scans);
- Local anaesthetic injections;
- Dye-injection studies such as a diskogram to identify painful disks in the spine or myelogram to identify areas of spinal nerve compression;
- Electromyography and nerve conduction studies to identify nerve abnormalities.
Chronic versus acute
Chronic pain can be defined as pain which lasts longer than what is considered a ‘normal’ healing time, perhaps as part of recovery from illness or injury – generally more than three months.
Chronic pain may be attributable to an event, such as an accident, developing from acute pain. Opinion differs as to whether previous acute pain is always the root cause of chronic pain or simply appears, sometimes without an initial cause. In some cases, especially in relation to sports injury in contact sports, the underlying chronic pain may appear sometime after an event. Pain may also be related to another condition. Surveys show that in Ireland, 35 per cent of reported chronic pain was arthritis related. It may site-specific, ie, back, knee, and wrist; however 80 per cent of sufferers in Ireland report that their pain relates to more than one site.
Types of chronic pain
Pain can be classified either by type of pain, or by body region. Classes of pain types include:
- Nociceptive pain: Aching, boring, worse on movement, anatomically defined, fluctuates in severity;
- Neuropathic pain: Burning sensation, sharp stabbing type, tingling, transient limb pain (shooting), associated with allodynia (experience of pain from a non-painful stimulation of the skin, such as light touch), hypersensitivity, or other sensory changes;
- Mixed nociceptive and neuropathic pain: Combination of symptoms;
- Visceral pain: Dull, non-specific, difficult to pinpoint;
- Autonomic symptoms: Physiological changes (colour, temperature), sweating.
Given the wide and varied nature of acute and chronic pain, there is a myriad of medication options. The effectiveness of medication depends on the nature and severity of the pain
Treatment
Aims of treatment are to:
- Reduce intensity of the pain;
- Enhance physical functioning;
- Improve mood;
- Promote the return to work or school and/or role within family and society;
- Improve quality of life;
- Support pain-management planning decisions;
- Reduce need for healthcare services.
- First-line treatment options include:
- Resting the affected area;
- Applying ice or heat;
- Paracetamol or non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, or naproxen;
- Exercise;
- Physiotherapy;
- Stress reduction;
- Bioelectric therapy (ie, local electrical stimulation like a TENs machine for moderate pain);
- Opioid medication such as codeine or morphine;
- Muscle relaxant medications.
Second-line treatment options include
Antidepressants: some tricyclics such as amitriptyline have a role in nerve pain and some antidepressants may be needed for mood and insomnia issues exacerbated by pain;
- Anticonvulsants: more often used for nerve pain;
- Nerve blocks: local anaesthetics to block nerve activity);
- Trigger point injections: to treat muscle spasms;
- Steroid injections: to reduce tissue inflammation;
- Acupuncture.
Medication
Overview of pain medications
A successful outcome from GP visits should be a pain management plan. It is highly likely that as part of this, some form of pain-relieving medication will be prescribed. Ideally, advice will be given on promotion of self-help, self-management, and other treatments to help improve patients’ condition and add value to the benefit offered by medication.
Given the wide and varied nature of acute and chronic pain, there is a myriad of medication options. The effectiveness of medication depends on the nature and severity of the pain.
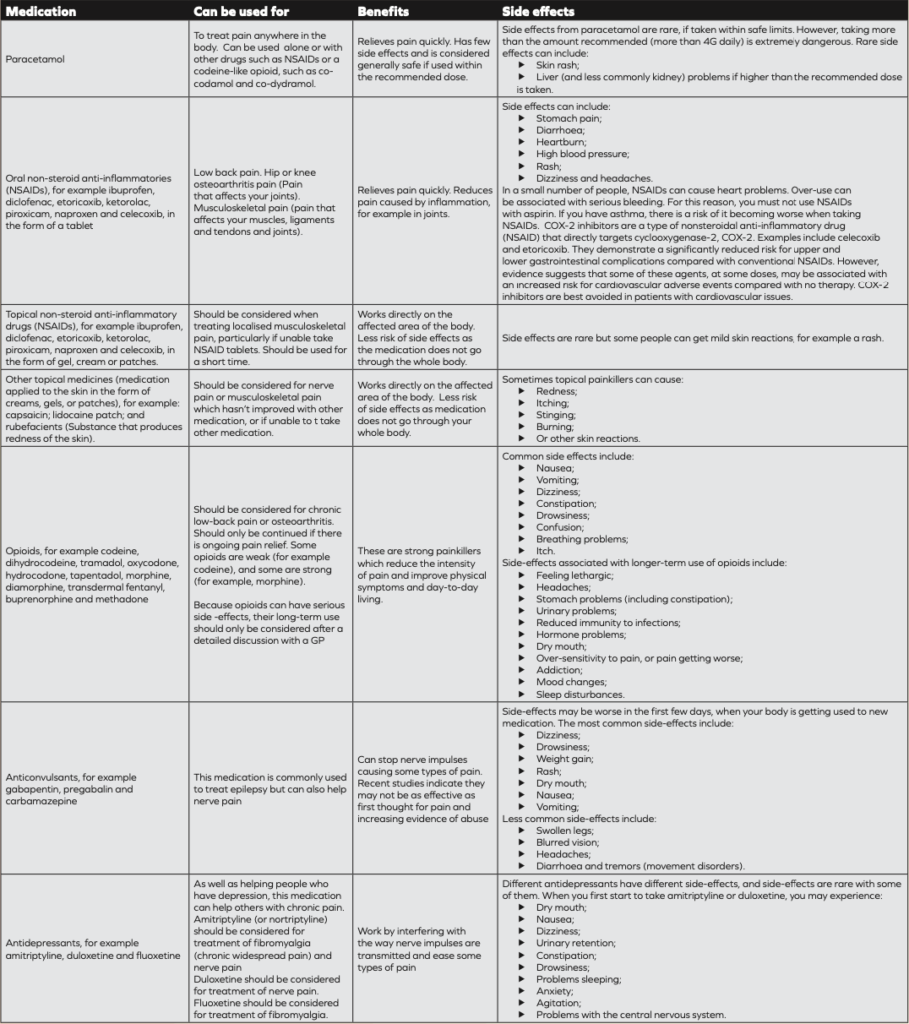
Types of medications, their benefits and potential side-effects are shown in the table, right.
Regarding treatment of acute pain caused by headache (ie, migraine), in addition to standard paracetamol and NSAIDs, triptans are considered the most effective to combat acute attacks if ordinary analgesics do not work.
These include:
- Almotriptan;
- Frovatriptan;
- Sumatriptan;
- Zolmitriptan;
- Eletriptan;
- Naratriptan.
All are POM, apart from sumatriptan, which has an OTC version available in Ireland.
Types of medications, their benefits and potential side-effects:
Efficacy of OTC painkillers
Cochrane reviews (39 in total) of randomised controlled trials on effectiveness of OTC analgesics in acute pain found reliable evidence to indicate that simple, inexpensive, and common analgesics give good pain relief to many patients with acute pain, such as headache, toothache, sprains, and strains. Data demonstrated the most efficacious OTC drugs used were ibuprofen/paracetamol combinations in respective 400mg/1000mg and 200mg/500mg doses.
These formulations gave effective relief in seven out of ten patients. Fast-acting ibuprofen 200mg and 400mg was effective in at least five out of ten patients. Paracetamol alone was effective four out of 10 patients.
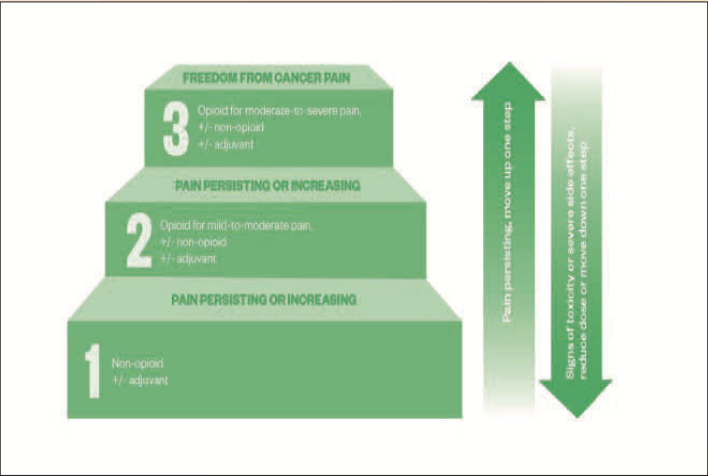
World Health Organization (WHO) analgesic ladder
The World Health Organization (WHO) analgesic ladder (introduced in 1986) was developed to help clinicians decide cancer pain treatment. It was developed for chronic pain, but the principles apply to the management of acute pain. Over-the-counter painkillers can be used for mild pain according to this tool, starting with a non-opioid (eg, paracetamol or aspirin) for mild pain then trialling an opioid plus a non-opioid (eg, co-codamol) for mild-to-moderate pain. Despite its origin to manage cancer-related pain, the WHO analgesic ladder now acts as a useful guide for pain control in both acute and chronic pain from malignant and non-malignant causes. As pain is a subjective experience, the stepwise approach of the WHO analgesic ladder is not always appropriate for managing intense pain.
Guidance on musculoskeletal injures
The American Academy of Family Physicians (AAFP) and American College of Physicians (ACP) guidelines published in 2020 (after a review of 13 million patients) recommending topical NSAIDs as first-line therapy for patients experiencing pain from musculoskeletal injuries (excluding lower back pain). The guidelines recommend that clinicians not prescribe opioids except in cases of severe injury or if patients cannot tolerate first-line therapeutic options.
The recommendations state that topical NSAIDs were the only intervention that improved all outcomes in patients with acute pain from non-lower back musculoskeletal pain. They found that topical NSAIDs also were among the most effective options for treatment satisfaction, pain reduction, physical function, and symptom relief, and were not associated with a statistically significant increased risk of adverse effects.
Oral NSAIDs were shown to be effective in reducing pain within two hours and one to seven days after treatment and were associated with greater likelihood of symptom relief. However, oral NSAIDs also were associated with an increased risk of gastrointestinal adverse events.
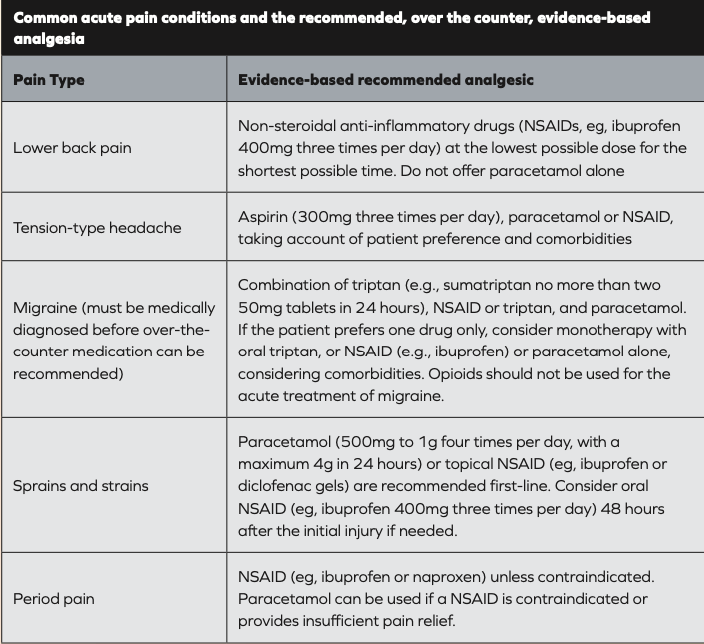
Reference: National Institute of Health and Care Excellence (UK)
World Health Organization (WHO) analgesic ladder
Self-help
Pain management programme
The Pain Management Program (PMP) is a psychologically based rehabilitative treatment for people with persistent pain. It is delivered in a group setting by a multidisciplinary team of experienced healthcare professionals working closely with patients. The main aim is to teach patients with similar problems about pain, how best to cope with it, and how to live a more active life. Referral to a Pain Management Programme is usually through the general practitioner to your local pain clinic.
There are public pain management programmes in*:
- St Vincent’s University Hospital, Dublin;
- The Adelaide and Meath Hospital (Tallaght), Dublin;
- The Mater Misericordiae University Hospital, Dublin;
- Mercy University Hospital, Cork. *This list not exhaustive
- Private hospitals also have pain clinics. For example, the Beacon Hospital operates an acute pain service and a chronic pain service.
- Physical therapy
Physical therapy covers several different treatment types, which can be beneficial for chronic pain, especially pain due to musculoskeletal disorders.
- Hot or cold (ice) pack treatment;
- Ultrasound;
- Peripheral nerve stimulation/transdermal electronic nerve stimulation (TENS).
A chartered physiotherapist can help with manual therapy, which helps to increase tissue extensibility and range of movement, thereby decreasing pain. Manual therapy can also help with alignment and joint mechanics issues, which can also help alleviate pain.
- Therapeutic exercise – Eg, hydrotherapy, can restore joint movement and flexibility and strengthen and condition muscles to help movement, thus reducing pain.
- Patient education – Can support physical therapy in a self-help or home-based manner. Reading and learning about their condition can assist in management of their own pain.
- Exercise – Staying active can be the key to improving chronic pain symptoms. Any activity that increases mobility can have not only a positive physical benefit, but also an affirming mental health benefit also.
Oral NSAIDs were shown to be effective in reducing pain within two hours and one to seven days after treatment and were associated with greater likelihood of symptom relief; but there was also a bigger risk of suffering gastrointestinal adverse events
Cognitive behavioural therapy (CBT)
CBT is a proven ‘talk therapy’, the primary aim of which is to reveal how to recognise and manage negative thinking or unhelpful beliefs that lead to increased distress.
CBT is generally delivered on a one-to-one basis, with the participant being taught techniques and strategies to enable them to challenge their thoughts and change their attitude, leading to a modification in future behaviour. Through regular attendance, confidence builds, leading to positive goal setting. These goals should relate to achieving resumption of activities previously restricted by pain. Learning problem-solving strategies and stress reduction techniques will help achieve a successful outcome.
Pharmacists’ role
The patient’s needs will affect treatment choice so pharmacists and pharmacy teams should have available (and understand) a range of guidance and literature to best advise patients about the most effective treatment for them.
Regularly reviewing the continued suitability of all medications used by those suffering with acute and chronic pain is vital. For many, the pharmacy is becoming the first port of call when a health problem – especially a pain-related one – arises. Using some of the ideas regarding questions, pain diary etc will really help in enabling people to make better informed decisions about their own next step. Becoming familiar with local resources like physios, support groups, condition specific charities – and signposting these – will only add value to a positive perception. l
Eamonn Brady MPSI (Pharmacist). Whelehans Pharmacies, 38 Pearse St and Clonmore, Mullingar. Tel 04493 34591 (Pearse St) or 04493 10266 (Clonmore). www.whelehans.ie. Eamonn specialises in the supply of medicines and training needs of nursing homes throughout Ireland. Email info@whelehans.ie
References upon request







