Cardiac conditions can be complex and multifactorial, depending on age, lifestyle, genetics and other factors. On completion of this module, the reader will have an enhanced understanding of the heart’s physiology, risk factors, diseases of the heart, and the importance of choosing the right therapy for the patient’s circumstances
Introduction: Heart Structure and Anatomy:
The heart is a conical, hollow, muscular organ located between the lungs. It maintains unidirectional blood flow throughout the body through its repetitive, rhythmical torsion and untwisting. The receiving chambers are the left and right atriums, and its pumping chambers are the ventricles. The right atrium receives the venous return via the vena cava and the coronary sinus artery. The sinus node, or sinoatrial (SA) node, a cluster of specialised myocardial cells that can spontaneously generate electrical impulses, is located where the superior vena cava meets the wall of the right atrium (the cavoatrial junction).
The right ventricle receives blood via the tricuspid valve, and ejects blood into the pulmonary artery via the pulmonic valve. The left atrium receives oxygen-rich blood from the pulmonary veins, which enters the left ventricle through the mitral valve. The left ventricle, the largest and thickest heart chamber, receives the oxygenated blood via the mitral valve during diastole and transfers it across the aortic valve during systole (Figure 1). All three coronary artery branches contribute to blood supply of the left ventricle, so ischaemic events here usually manifest as regional wall motion abnormalities.1

FIGURE 1: The human heart2
The right and left coronary arteries branch off the aorta. There is some variability in their exact origin and distribution, but the right coronary artery usually supplies the right ventricle, and the left supplies the anterior and lateral left ventricle. The blood supply to the rest of the ventricle depends on the coronary dominance, ie, which artery supplies the posterior descending artery. Cardiac veins (great, middle, and small, among others) carry deoxygenated blood from the myocardium into the right atrium.
The pacemaker of normal cardiac muscle is the SA node. Electrical signals arising in the SA node stimulate the atria to contract. Then the signals travel to the atrioventricular node (AV node), which is located in the interatrial septum. After a short delay that allows the ventricles to fill, the electrical signal is conducted through the bundle branches of His to the respective Purkinje fibres for each side of the heart, as well as to the apex of the heart, then finally to the ventricles, causing the ventricles to contract. These rhythmic signals result in the co-ordinated rhythmic contraction and relaxation.
PHARMACOLOGICAL MANAGEMENT Antiarrhythmic drugs
The clinical effect of all antiarrhythmic drugs is determined by their effects on the action potential and refractory period of the cardiac action potential.1 L and T type calcium channels, present in the myocardium, are the targets of calcium channel blockers (CCBs).
- Class I drugs are subdivided into subclasses A, B, and C.3 Class I drugs are all sodium channel blockers (membrane- stabilising drugs) that block fast sodium channels, slowing conduction in fast-channel tissues (working on atrial and ventricular myocytes and the His-Purkinje system).
- Class 1A causes moderate-degree blockage of fast sodium channels. Their use is limited due to proarrhythmic effects because of their effect of prolonging the QT interval,4 ie, disopyramide, quinidine. The QT interval is inversely proportional to heart rate: It shortens at faster heart rates and lengthens at slower heart rates. An abnormally prolonged QT is associated with an increased risk of ventricular arrhythmias.1
- Class 1B causes a mild-degree blockage of sodium channels,4 shortening the QT interval, and is used for ventricular arrhythmias, ie, lidocaine, mexiletine.
- Class 1C causes a marked degree of sodium blockage, and has no effect on QT interval, ie, flecainide, propafenone.
- Class II drugs are beta blockers (BB), which predominantly affect slow-channel tissues (the SA and AV nodes), where they decrease conduction velocity and prolong the refractory period. Beta 1 receptors are located on the SA node, AV node and myocardium, where activation results in faster heart rate and more forceful contractions.3 BBs are used for rate control in patients with atrial fibrillation (AF) and atrial flutter. These
are often first-line choices because of their excellent safety profile and effectiveness in treating ventricular arrhythmias.4 BBs are discussed in more detail in their own section.
- Class III drugs are primarily potassium channel blockers,3 which prolong action potential duration and refractory period in slow- and fast-channel tissues, and prolong the QT interval.4 Amiodarone is recommended in AF to maintain sinus rhythm and also for ventricular arrhythmia (VA). Dronedarone is used for AF in patients who do not have permanent AF. Sotalol is a BB used to treat both VA and supraventricular arrhythmias, sharing effects of multiple classes of antiarrhythmic agents.
- Class IV drugs are the nondihydropyridine CCBs, which decrease conduction velocity and slow conduction through the AV node, ie, diltiazem, verapamil. They are useful for ventricular rate control in acute and chronic AF and atrial flutter, as well as in hypertension.
Alpha blockers
Prazosin, doxazosin and tamsulosin are selective alpha 1 receptor antagonists. These decrease vascular resistance with minimal increase in heart rate. Tamsulosin is a selective alpha 1A blocker used for symptomatic benign prostatic hyperplasia and to help with the passage of kidney stones. Orthostatic hypotension may occur with these drugs, especially after the initial dose.1 Clonidine is a centrally acting alpha agonist almost fully selective for alpha 2 receptors, which causes a reduction in vascular resistance. It is also an effective analgesic when administered epidurally. It should not be discontinued abruptly due to resulting rebound hypertension.
Angiotensin-converting enzyme inhibitors
When peripheral blood volume is low and renal perfusion is reduced, renin is released by the kidneys. This results in production of angiotensin I ( from the cleavage of angiotensinogen), which is cleaved into the potent vasoconstrictor angiotensin II (ATII) by angiotensin converting enzyme (ACE). This also stimulates aldosterone secretion from the adrenal cortex, which leads to sodium and water retention. ATII normally binds to the AT1 receptor to produce its vasoconstrictive effects, and it also mediates alveolar permeability.
ACE inhibitors (ACEi, ie, ramipril, lisinopril, perindopril, quinapril) block the ATI to ATII conversion. They also block breakdown of bradykinin, an endogenous vasodilator. The build-up of this substance is responsible for
the potential side-effects of a chronic, non- productive cough, and angioedema.1
Angiotensin receptor blockers
ATII levels may still remain elevated even with ACEi treatment, because there are additional biochemical pathways that still produce ATII. ARBs (ie, losartan, valsartan) are an alternative drug class that produce antihypertensive effects through the direct blockade of ATII receptors, with no effect on ACE. As a result, they do not cause the side-effects of ACEis that are related to this, ie, cough, angioedema. They act as diuretics, and counteract cardiac remodelling that can occur in hypertension, heart failure, and myocardial infarction.1
Angiotensin receptor- neprilysin inhibitors
Clinical trials have shown a mortality benefit from sacubitril/valsartan ARNI combinations when used in patients with chronic heart failure. Natriuretic peptides, which are made by the heart, are potent vasodilators with natriuretic (sodium excretion in the urine) properties.1 Neprilysin is an endogenous peptidase that degrades natriuretic peptides. Sacubitril, a neprilysin inhibitor, increases the concentration of natriuretic peptides, leading to increased vasodilation. Natriuretic peptides also inhibit the renin-angiotensin-aldosterone (RAAS) axis. RAAS activation leads to vasoconstriction, hypertension, and increased aldosterone levels, and worsening heart failure.5
Because neprilysin also breaks down ATII, inhibition of neprilysin with sacubitril will cause ATII to build up. For this reason, a neprilysin inhibitor must always be combined with an ARB to block the effect of the excess angiotensin II.
Antiplatelet drugs
Antiplatelet medications are an important part of pharmacological management of the secondary prevention of atherosclerotic cardiovascular and cerebrovascular diseases. Besides there being little evidence of any benefit for their use in primary prevention (ie, in cases where there are no previously documented cardio/cerebrovascular events), they also carry the risk of excess bleeding.6 In cases of documented disease (ie, secondary prevention), stable patients benefit from long- term antiplatelet monotherapy.
Aspirin is the first choice for those with CHD, and clopidogrel in those with cerebrovascular disease. Recent evidence shows that low-dose rivaroxaban in combination with aspirin provides additional benefits in certain patient cohorts. In patients with acute cerebrovascular disease, aspirin combined with clopidogrel reduces risk of recurrence, while in acute coronary syndrome (sudden, reduced blood flow to the heart), dual antiplatelet therapy (DAPT) consisting of aspirin and a P2Y12 inhibitor (clopidogrel, prasugrel or ticagrelor) gives greater protection than aspirin monotherapy. Prasugrel and ticagrelor offer more pronounced and faster antiplatelet effects than clopidogrel. While this greater antiplatelet efficacy is favourable for the prevention of thrombotic events, the increased risk of bleeding may be a particular issue in certain patient groups.
Beta blockers
BBs inhibit myocardial and peripheral vascular beta 1 receptors, causing a reduction in heart rate, contractility, and myocardial oxygen consumption. While often first-line treatment for arrhythmias, they are generally not preferred as first-line treatment for initial management of hypertension, but may be considered as add-on therapy in patients who do not respond adequately to treatment with other drug classes. They can precipitate congestive heart failure, especially when used with other myocardial depressants, ie, CCBs.1
Propranolol, a non-selective BB and highly soluble, is associated with a higher frequency of CNS side-effects. It reduces heart rate and contractility, which are marked in sympathetically-driven disease states. Metoprolol was the first selective beta 1 blocker, which mostly avoids the increased airway resistance in asthma patients that
is observed with the use of non-selective BBs. Atenolol and bisoprolol are also cardioselective. Labetalol is a non-selective BB with selective alpha 1 blocking properties (three times more potent at beta blockade than alpha).
Calcium channel blockers
CCB drugs bind to voltage-gated transient (T), long (L) type channels in the myocardium and smooth muscle (or to neural (N) type channels). This selectively inhibits calcium influx into the myocardial and smooth muscle cells. Non-dihydropyridines are discussed previously under antiarrhythmics.
Dihydropyridines, ie, nifedipine, amlodipine, mostly exert their effects peripherally, with little direct effect on the heart. They prevent calcium entry into the vascular smooth muscle cell by extracellular modulation of the L-type channels. Each CCB has its own properties. They are commonly used for treatment of stable angina.1
Coronary vasodilators
Glyceryl trinitrate (GTN) is a smooth muscle relaxant that maximises blood flow. When it enters the smooth muscle cells, it generates nitric oxide, which results in peripheral vasodilation. GTN reduces myocardial oxygen demand, and increases oxygen supply.
Digoxin
Digitalis is a cardiac glycoside that selectively and reversibly inhibits the integral membrane protein Na+/K+ ATPase ion transport system: This determines myocardial excitability and action potential. Digoxin, the commercially available version of Digitalis, binds externally to this transport system and makes more calcium available to generate contraction.1 Overall, it increases the force of the heartbeat and decreases the heart rate.7
Direct oral anticoagulants
NICE now recommends the use of these drugs in preference to vitamin K antagonists like warfarin. Trials have shown that DOACs are even more effective than warfarin in stroke prevention and have lower haemorrhage risk, and NICE even suggests that those on warfarin for AF may be invited to switch to a DOAC where appropriate.8 Apixaban, dabigatran, edoxaban, and rivaroxaban are all recommended as options.
The mechanism of action of all DOACs is factor Xa inhibition. When prothrombinase complex-bound and clot-associated factor Xa is inhibited, this results in a reduction of the thrombin released during the coagulation cascade. These drugs do not directly affect platelet aggregation induced by collagen, adenosine diphosphate or thrombin, but by inhibiting factor Xa, they indirectly decrease clot formation induced by thrombin.9
Ivabradine
Ivabradine is a hyperpolarisation-activated cyclic nucleotide-gated (HCN) channel blocker. It is a sinoatrial modulator used to treat specific cases of chronic stable angina and heart failure. It reduces the heart rate by inhibiting a specific type of cardiac pacemaker current (‘funny’ current) in the sinoatrial node, which, unlike BBs or CCBs, produces selective heart rate control without affecting ventricular repolarisation or myocardial contractility.1
Statins
Statins are the most effective oral agents for the prevention and treatment of cardiovascular diseases associated with dyslipidaemia.10 Statins reach the liver via the portal blood and enter the hepatocyte, where they inhibit the 3-hydroxy-methylglutaryl- coenzyme A reductase (HMG-CoAR) and are then metabolised. Statins are reversible competitive inhibitors of HMG-CoAR, which results in a reduction of intracellular cholesterol synthesis. This inhibition also leads to reduced synthesis of other compounds including bile acids, ubiquinone, steroids, and vitamin D.
The myotoxicity of statins results from the inhibition of this same enzyme in the myocytes and has been estimated
to affect between 7 and 29 per cent of patients. Pharmacokinetic and myocyte conditions both contribute to this effect, as well as risk factors such as age, gender, ethnicity, genetics, and polypharmacy. Drug interactions may account for up to 50 per cent of statin-induced myotoxicity. It has been suggested that pravastatin
and rosuvastatin may be less prone to produce this than simvastatin, atorvastatin, fluvastatin, and lovastatin.
CARDIAC HEALTH
Factors that can increase the risk of poor cardiovascular health, ie, hypertension, atherosclerosis, strokes, and angina, include:11,12,13
- Age.
- Family history.
- High-salt diet.
- Lack of exercise.
- Being overweight.
- Alcohol.
- Smoking (increases the risk of developing heart disease by 24 per cent).
- Long-term sleep deprivation or obstructive sleep apnoea.
- Diabetes may cause the lining of blood vessels to become thicker, which can restrict blood flow.
HYPERTENSION
Lifestyle changes to reduce blood pressure include reducing salt intake to less than 6g (0.2oz) a day, eating a balanced diet, exercising, reducing alcohol, smoking cessation, and adequate sleep. The HSE recommends that people aged 40 years or older should have their blood pressure checked at least annually. As a general guide:11
- High blood pressure is 140/90mmHg or higher (or an average of 135/85mmHg at pharmacist home), or if over the age of 80, high blood pressure is 150/90mmHg or higher (or an average of 145/85mmHg at home).
- Ideal blood pressure is usually considered to be between 90/60mmHg and 120/80mmHg. The target for over-80s is below 150/90mmHg (or 145/85mmHg at home).
In about 5 per cent of cases, hypertension is caused by an underlying health condition or medication side-effects. Health conditions such as kidney disease, diabetes, long-term kidney infections, obstructive sleep apnoea, and hormonal problems can contribute to hypertension. The oral contraceptive pill, steroids, NSAIDs, and some SNRI antidepressants can also increase blood pressure.
Medication is indicated for hypertension when lifestyle modifications fail to control blood pressure adequately. The main determinants of blood pressure are cardiac output and peripheral vascular resistance. Heart rate is altered by BB, CCBs, and ivabradine. Peripheral resistance is reduced by alpha blockers, ACEi, ARBs, CCBs, diuretics, or direct vasodilators like GTN. NICE guidelines14 recommend an ACEi or ARB if under 55 years of age, or a CCB, thiazide diuretic, ACEi or a combination if aged 55 or older. Additional medication from alternative drug classes can be added until blood pressure is adequately controlled. Figure 2 presents a visual summary of the NICE guidelines for hypertension treatment.
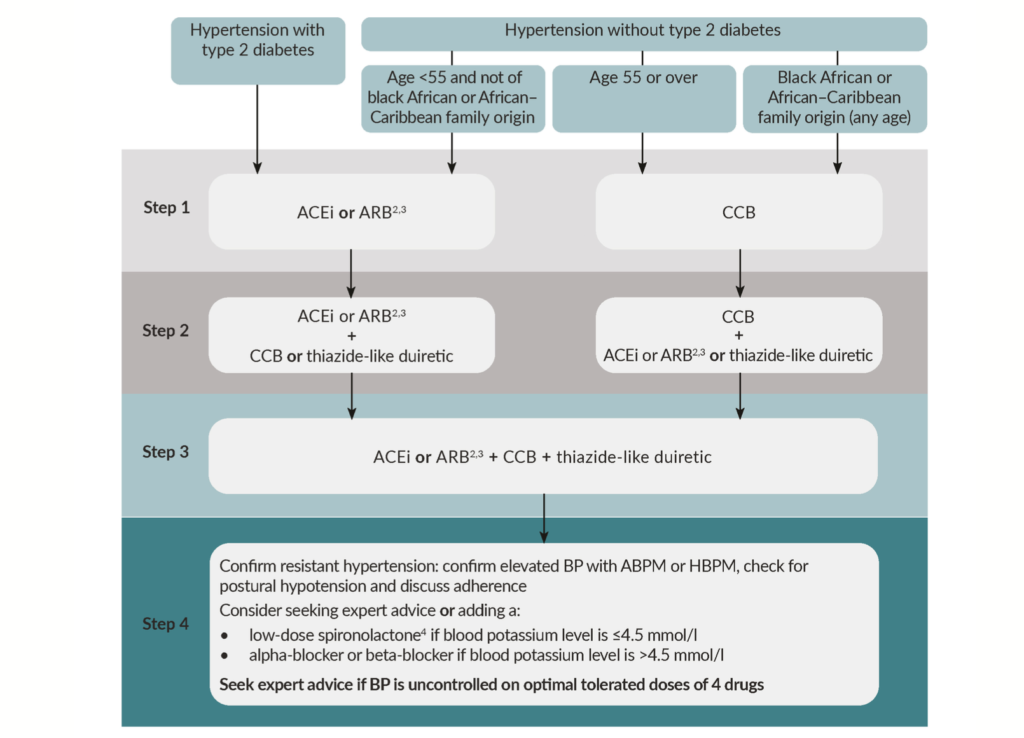
FIGURE 2: NICE guidelines for hypertension treatment: Visual summary15
ANGINA AND CORONARY HEART DISEASE
Chest pain caused by angina usually feels tight, dull or heavy and may spread to the left arm, neck, jaw or back along with symptoms of nausea, shortness of breath, and palpitations. It is often triggered by physical exertion or stress, and stops after resting. Stable angina has a trigger (ie, stress or exercise) and stops within a few minutes of resting. Unstable angina is more unpredictable and can continue despite resting. Angina and coronary heart disease (CHD) are usually caused by atherosclerosis, which reduces the blood supply to the heart. Heart failure can also occur in people with CHD when the heart becomes too weak to pump blood efficiently, causing fluid to build up in the lungs and making it difficult to breathe.
GTN mouth spray is used to treat angina. Additional medicines such as antiplatelet/anti- clotting drugs, especially for stroke prevention in unstable angina, are often indicated.12,16 Optimal pharmacological treatment for stable angina consists of one or two anti-anginal drugs as needed, along with medicines for secondary prevention.12,17 A BB and/or CCB are recommended as first-line treatment for stable angina by NICE. For secondary prevention
of cardiovascular disease, NICE guidelines recommend considering 75mg aspirin daily for people with stable angina, along with ACEIs, statins, and any additional appropriate treatment for hypertension if needed. Statins are prescribed as necessary for high cholesterol. Surgery may be recommended if medicines are not controlling the angina, ie, coronary artery bypass graft (CABG) and percutaneous coronary intervention (PCI).
LIPID MODIFICATION THERAPY
Estimating cardiovascular risk is a big part of the prevention of cardiovascular disease. This can be done using a global risk score, which can be calculated using one of a number of different validated risk tools. The National Institute for Health and Care Excellence (NICE) recommends estimating an individual’s risk of cardiovascular disease (CVD) on an ongoing basis using the QRISK3 tool. People at high risk of or with CVD are advised to reduce their saturated fat intake and increase their mono-unsaturated fat intake with olive oil, rapeseed oil or spreads based on these oils and to use them in food preparation.
Statins should be considered for primary prevention of CVD in some patient groups, ie, those with type 1 diabetes over the age of 40. First-line pharmacological treatment for primary and secondary prevention of CVD as recommended by NICE is atorvastatin 20mg and 80mg, respectively. Once started, a follow-up cholesterol test should be performed after three months of treatment. If non-HDL cholesterol is not reduced by 40 per cent or more, a dose increase should be considered (along with a discussion about adherence to recommended diet/lifestyle changes and medication). Annual reviews should be provided.17
If not tolerated, the statin can be stopped, and started again when symptoms have resolved to check if symptoms were related to the statin. Alternatively, a reduced dose can be prescribed, or a different statin, ie, rosuvastatin, can be used. Ezetimibe is an option for those who cannot take or tolerate a statin.18 Recent clinical studies have shown clear evidence that higher doses of omega 3 polyunsaturated fatty acids (2–4g/ day of EPA + DHA) appear to be safe and associated with a significant reduction in CVD events, although are not recommended so far by NICE for CVD prevention.19
Author: Dr Donna Cosgrove, PhD. Donna’s overall aim is to improve patient outcomes through education. After graduating with a BSc in Pharmacy, she returned to university to complete a MSc in neuropharmacology. This led to a PhD investigating the genetics of schizophrenia, followed by a postdoctoral research position in the same area. She has worked in hospital, research, and community pharmacy settings and is currently a community pharmacist in Galway and a clinical writer.
REFERENCES
- Bauer M (2018). Cardiovascular anatomy and pharmacology. Basic Sciences in Anaes- thesia, 195-228. Available at: www.ncbi.nlm. nih.gov/pmc/articles/PMC7121118/.
- Wapcaplet, via Wikimedia Commons (2006). Diagram of the human heart – CC BY- SA 3.0. Available at: http://creativecommons. org/licenses/by-sa/3.0/.
- 3. Mitchell BL (2023). Merck Manuals Profes- sional Edition: Medications for arrhythmias. Available at: www.msdmanuals.com/profes- sional/cardiovascular-disorders/overview- of-arrhythmias-and-conduction-disorders/ medications-for-arrhythmias.
- King GS, Goyal A, Grigorova Y, Hashmi
MF (2022). Antiarrhythmic medications. In StatPearls [Internet]. StatPearls Publishing. Available at: www.ncbi.nlm.nih.gov/books/ NBK482322/. - Nicolas D, Kerndt C, Reed M (2022). Sacubitril-Valsartan. NCBI National Centre for Biotechnology Information. Available at: www. ncbi.nlm.nih.gov/books/NBK507904/.
- Passacquale G, Sharma, P, Perera D, Ferro A (2022). Antiplatelet therapy in cardiovas- cular disease: Current status and future direc- tions. British Journal of Clinical Pharmacology, 88(6), 2686-2699.
- DrugBank Online (2023). Digoxin: Uses, in- teractions, mechanisms. Available at: https:// go.drugbank.com/drugs/DB00390.
- Jones NR, Round T, Rajappan K (2022). Atrial fibrillation: NICE 2021 update and the focus on anticoagulation. British Journal of General Practice, 72(717), 193-195.
- Schwarb H, Tsakiris DA (2016). New direct oral anticoagulants (DOAC) and their use today. Dentistry Journal, 4(1), 5
- du Souich P, Roederer G, Dufour R (2017). Myotoxicity of statins: Mechanism
of action. Pharmacology and Therapeutics, 175, 1-16. - Health Service Executive (2022). Overview high blood pressure (hypertension). Available at: www2.hse.ie/conditions/high- blood-pressure-hypertension/.
- Health Service Executive (2021). Overview angina. Available at: www2.hse.ie/ conditions/angina/.
- Health Service Executive (2021). Over- view coronary heart disease (CHD). Available at: www2.hse.ie/conditions/coronary-heart- disease-chd/.
- National Institute for Health and Care Excellence (2022). Hypertension in adults: Diagnosis and management. [NICE Guideline no. 136]. Available at: www.nice.org.uk/ guidance/ng136/resources/hypertension- in-adults-diagnosis-and-management- pdf-66141722710213.
- National Institute for Health and Care Excellence (2022). Hypertension in adults: Diagnosis and management. [NICE Guideline No 136 Visual Summary]. Available at: www. nice.org.uk/guidance/ng136/resources/ visual-summary-pdf-6899919517.
- National Institute for Health and Care Excellence (2016). Stable angina: Manage- ment. [NICE Guideline no. 126]. Available at: www.nice.org.uk/guidance/cg126/chapter/ Guidance#drugs-for-secondary-prevention- of-cardiovascular-disease.
- National Institute for Health and Care Excellence (2022). Cardiovascular disease: Risk assessment and reduction, including lipid modification [NICE Guideline No 181]. Available at: www.nice.org.uk/guidance/ cg181/chapter/Recommendations#lipid- modification-therapy-for-the-primary-and- secondary-prevention-of-cardiovascular- disease.
- National Institute for Health and Care Excellence (2016). Ezetimibe for treating pri- mary heterozygous-familial and non-familial hypercholesterolaemia. [NICE Technology ap- praisal guidance TA385] Available at: www. nice.org.uk/guidance/TA385/chapter/1- Recommendations.
- Elagizi A, Lavie CJ, O’Keefe E, Marshall K, O’keefe JH, & Milani RV (2021). An update on omega-3 polyunsaturated fatty acids and cardiovascular health. Nutrients, 13(1), 204.






