A clinical overview of the importance of controlling cholesterol levels to prevent atherosclerosis, heart attacks and strokes
Cholesterol is a lipid (fat). It is manufactured by the liver from the fatty foods that we eat, and plays a vital part in allowing the body to function normally. Cholesterol is present in the membrane (outer layer) of every cell in the body. It insulates nerve fibres and is an essential building block for hormones, such as the sex hormones, and the hormones of the adrenal cortex. It also enables the body to produce bile salts.
Cholesterol is carried in the blood by molecules called lipoproteins. There are several different lipoproteins, but the three main types are:
- Low-density lipoprotein (LDL). This is often known as ‘bad’ cholesterol and is thought to promote arterial disease. It carries cholesterol from the liver to the cells and can cause a harmful build-up if there is too much for the cells to use. Normally, the blood contains about 70 per cent of LDL, but the level will vary from person-to-person. Recommended LDL level is below 3.37mmol/l.
- High-density lipoprotein (HDL). This is often referred to as ‘good’ cholesterol, and is thought to prevent arterial disease. It takes cholesterol away from the cells and back to the liver, where it is either broken down, or is passed from the body as a waste product. Recommended LDL range is 1.45-4mmol/l.
- Triglycerides are another type of fatty substance present in the blood. They are found in dairy products, meat, and cooking oils. Triglycerides are also produced by the liver. Those who are overweight, have a diet that is high in fatty or sugary foods, or drink a large amount of alcohol, have an increased risk of having a high triglyceride level.
Recommended triglyceride level is below 1.71mmol/l. The amount of cholesterol present in the blood can range from 3.6 to 7.8mmol/litre. A level above 6mmol/litre is considered high, and a risk factor for arterial disease. A total cholesterol level of below 5.2mmol/litre is recommended to prevent heart disease.
Evidence strongly indicates that high cholesterol levels can cause narrowing of the arteries (atherosclerosis), heart attacks, and strokes. The risk of coronary heart disease also rises as blood cholesterol levels increase. If other risk factors, such as high blood pressure and smoking, are present, the risk increases even more.
Symptoms
High cholesterol is not a disease in itself, but it is linked to serious conditions, such as cardiovascular conditions (disease of the heart and blood vessels), angina, stroke, and mini-stroke, known as transient ischemic attack (TIA). A high level of cholesterol in the blood, together with a high level of triglycerides, can increase the risk of developing coronary heart disease.
Coronary heart disease is caused by narrowing of the arteries that supply the heart with blood. This narrowing of the arteries is called atherosclerosis. Fatty deposits, such as cholesterol, cellular waste products, calcium and other substances build-up in the inner lining of an artery. This build-up, known as plaque, usually affects small and medium-sized arteries. The flow of blood through the arteries is restricted, as the inside diameter is reduced. Blood clots, which often happen in the coronary arteries during a heart attack, are more likely to develop when arterial walls are roughened by the build-up of fatty deposits.
A high cholesterol level may only be revealed with symptoms of atherosclerosis. These can include:
- Angina, caused by narrowed coronary arteries in the heart.
- Leg pain on exercising, due to narrowing of the arteries that supply the lower limbs.
- Blood clots and ruptured blood vessels, which can result in a stroke or TIA.
- Ruptured plaques, which can lead to a blood clot forming in one of the arteries delivering blood to the heart (coronary thrombosis), and may lead to heart failure if a significant amount of heart muscle are damaged.
- Thick yellow patches (xanthomas) around the eyes or elsewhere on the skin. These are cholesterol deposits and can often be seen in people with inherited or familial cholesterol (where close family members have a history of high cholesterol).
Causes
A number of different factors can contribute to high blood cholesterol:
- Lifestyle risk factors
There are a number of preventable lifestyle-related risk factors that can increase the risk of developing high blood cholesterol. They include:
- Unhealthy diet — some foods contain cholesterol (known as dietary cholesterol) for example, liver, kidneys and eggs. However, dietary cholesterol has little effect on blood cholesterol. More important is the amount of saturated fat in the diet. Foods that are high in saturated fat include red meat, meat pies, sausages, hard cheese, butter and lard, pastry, cakes and biscuits, and cream, such as soured cream and crème fraîche.
- Lack of exercise or physical activity — can increase the level of LDL and decrease level of HDL.
- Obesity — being overweight means increased risk of high LDL and a decreased level of HDL, increasing overall blood cholesterol level.
- Smoking.
- Drinking excessive amounts of alcohol — the recommended amount is three-to-four units a day for men, and two-to-three units a day for women.
2. Treatable risk factors
- Hypertension (high blood pressure).
- Diabetes.
- A high triglyceride blood level.
- Medical conditions, such as kidney and liver diseases, and an under-active thyroid gland
3. Fixed risk factors
- A family history of heart disease or stroke — it is more likely to have high cholesterol if one has a close male relative (father or brother) aged under 55, or a female relative (mother or sister) aged under 65, who has been affected by coronary heart disease or stroke.
- A family history of cholesterol-related conditions, for example, if a close relative, such as a parent, brother, or sister has familial hypercholesterolemia, or combined hyperlipidaemia.
- Being male — men are more at risk of having high blood cholesterol than women.
- Age — the older we get, the greater the likelihood of developing atherosclerosis.
- Early menopause in women.
- Ethnic group — people who are of Indian, Pakistani, Bangladeshi, or Sri Lankan descent have an increased risk of high blood cholesterol. If a patient has a fixed risk factor (or several fixed risk factors), it is even more important to take steps to address any lifestyle, or treatable, risk factors.
Reduction in death rate from CHD in Ireland over the last 35 years
According to research published in the Journal of Epidemiology and Community Health in 2006, changes in three classic cardiovascular risk factors (smoking, cholesterol, and blood pressure) contributed to a 61.9 per cent decrease of total coronary heart disease (CHD) mortality in Ireland between 1985 to 2000; this was consistent with studies in other developed countries. In Ireland in 2000, heart disease was the leading cause of death, being responsible for 41 per cent of all deaths. In 2020, CSO figures show that diseases of the circulatory system (which includes CHD) were responsible for 26.3 per cent of all deaths.
A high cholesterol level may only be revealed with symptoms of atherosclerosis
Smoking reduction is a big factor, but better diagnosis of cholesterol and hypertension, along with better and earlier treatment interventions, is a big factor in this drop in deaths from heart disease. The better availability and affordability of statins in controlling cholesterol is also seen as a major factor in this reduction of deaths from CHD.
Diagnosis
To measure cholesterol, a simple blood test is often carried out. Before the test is done, it is best not to eat for 12 hours (usually including night-time when asleep). This ensures that all food is completely digested and will not affect the outcome of the test. A GP, practice nurse or pharmacist can carry out the blood test and will take a sample either using a needle and a syringe, or by pricking a finger.
The blood sample that is taken during the blood test will be used to determine the amount of LDL, HDL, and triglycerides in blood. Blood cholesterol is measured in units called millimoles per litre of blood (mmol/litre). It is recommended to have a total blood cholesterol level of less than 5mmol/litre, and an LDL cholesterol level of under 3mmol/litre.
Anyone can have their blood cholesterol level tested, but it is particularly important to have it checked if:
- Aged over 40.
- A family history of cardiovascular disease, for example, if one’s father or brother developed heart disease or had a heart attack, or a stroke before the age of 55, or if one’s mother or sister had these conditions before the age of 65.
- A close family member has a cholesterol-related condition, such as familial hypercholesterolaemia, or combined hyperlipidaemia.
- Are overweight or obese.
- Have high blood pressure (hypertension).
- Have a medical condition, such as a kidney condition, an under-active thyroid gland, or acute inflammation of the pancreas (acute pancreatitis). This is because these conditions can cause an increased level of cholesterol.
- In assessing risk of cardiovascular disease, heart attack, or stroke, cholesterol ratio should not be taken on its own. Lifestyle factors should also be taken into consideration.
For example:
- Smoking.
- Diet.
- BMI (body mass index — weight in relation to height).
- Treatable risk factors, such as high blood pressure (hypertension) and diabetes.
- Fixed risk factors, such as age, sex, and ethnicity.
Complications of high cholesterol
High cholesterol levels can be made worse by any other medical conditions. Medical problems such as an under-active thyroid gland, an overactive pituitary gland, liver disease, or kidney failure, can all contribute to high cholesterol levels.
Some people have inherited disorders, such as familial hypercholesterolemia, or combined hyperlipidaemia, that prevent fats from being used properly and eliminated from the body. This allows the level of cholesterol to build up in the blood.
The major complications of raised blood cholesterol are heart attacks, strokes and arterial disease. The risks of all of these are increased if the patient is/has:
- Overweight.
- A smoker.
- Has high blood pressure.
- Strong family history of these conditions.
- Diabetic.
Prevention
Patients can prevent high blood cholesterol by eating a healthy, balanced diet that is low in saturated fat. Including a small amount of unsaturated fats in the diet is a healthy choice, as this type of fat can actually reduce cholesterol levels. Current thinking is that the traditional Mediterranean diet, with its emphasis on raw olive oil in many foods and low animal fat content, is effective in ensuring cardiovascular health.
After a few months, if the cholesterol level has not dropped, advice may be to take cholesterol-lowering medication
Foods high in unsaturated fats include:
- Oily fish.
- Avocados.
- Nuts and seeds.
- Sunflower, rapeseed, and olive oil.
- Vegetable oils.
Treatment
When diagnosed with high cholesterol, the first method of treatment will usually involve making dietary changes (adopting a low-fat diet), and ensuring plenty of regular exercise. After a few months, if the cholesterol level has not dropped, advice may be to take cholesterol-lowering medication.
Diet
Ensuring a healthy diet by changing to one that is low in saturated fats can reduce levels of LDL or bad cholesterol. If in a high-risk category of getting cardiovascular disease, altering diet will not lower risk sufficiently. A healthy diet includes foods from all different food groups, including carbohydrates (cereals, wholegrain bread, potato, rice, pasta), proteins (for example, from lean meat, such as chicken and oily fish like mackerel or sardines), and fats (varieties that are unsaturated, such as low-fat mono- or poly-unsaturated spreads, and vegetable or sunflower oil). Eat at least five portions of a variety of different fruit and vegetables daily.
Cholesterol-lowering medication
There are several different types of cholesterol-lowering medication which work in different ways. Commonly-prescribed medication includes:
- Statins (HMG-CoA reductase inhibitors). Statins, such as simvastatin and atorvastatin, work by blocking the enzyme (chemical) in the liver that is needed for making cholesterol. Statins are used to reduce cholesterol to less than 4mmol/l and LDL cholesterol to less than 2mmol/l. They are therefore useful in preventing and treating atherosclerosis, which can cause chest pain, heart attacks, and strokes. Statins sometimes have mild side-effects which can include constipation, diarrhoea, headaches, and abdominal pain.
- Aspirin may be recommended, depending on age and several other factors. A low daily dose of aspirin can prevent blood clots from forming. (Children under 16 years should not take aspirin).
- Niacin is a B vitamin that is found in foods and in multivitamin supplements. In high doses, available by prescription, niacin lowers LDL cholesterol and raises HDL cholesterol. Minor side-effects include flushing or tingling skin, itching, and headaches. More research is needed to prove the effectiveness of niacins in reducing cholesterol.
- Other medications, such as cholesterol absorption inhibitors (ezetimibe), and bile-acid sequestrants (ie, cholestyramine), are sometimes used to treat high cholesterol. However, bile-acid sequestrants may be less effective than other forms of treatment and have more side-effects. PCSK9 inhibitors are a new type of cholesterol medication for resistantly high cholesterol administered in subcutaneous form either twice-weekly or monthly.
- If the patient has high blood pressure (hypertension), the GP may also prescribe medication to lower it.
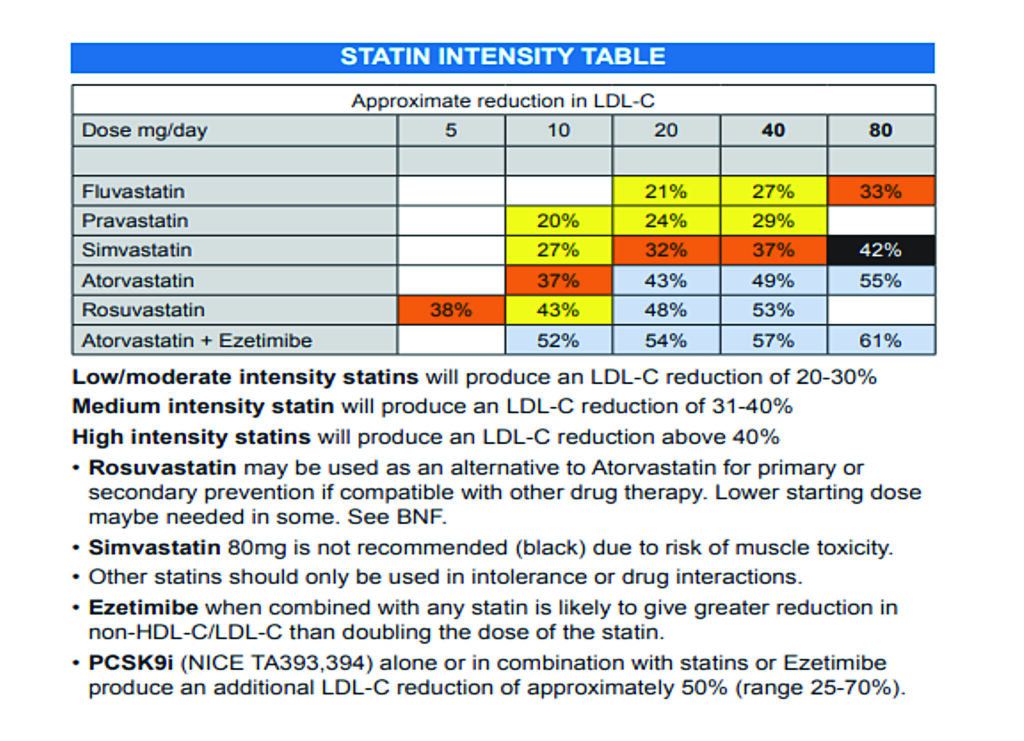
Statins
Statins are world’s most prescribed drugs and are effective medications in reducing cholesterol in most patients. There are several types of statins on the market, but they all work in the same way. Examples of statins available on the market are atorvastatin, pravastatin, rosuvastatin, simvastatin and fluvastatin.
Statins are only available with a doctor’s prescription in Ireland. Since 2004, simvastatin 10mg has been available over-the-counter in pharmacies in the UK; however, they are sold under strict guidelines under the supervision of the pharmacist and the patient must meet specific criteria, ie, patients targeted are those at a 10-to-15 per cent risk of an event in 10 years.
Clinical trials show that statins are very effective at reducing cholesterol and hence heart disease. Statins are one of the major reasons for the significant fall in the death rate from heart disease in Ireland since they were first launched over 30 years ago. Statins work by blocking the enzyme HMG-CoA reductase, which plays an important role in the production of cholesterol in the liver. They are therefore useful in preventing and treating atherosclerosis, which can cause chest pain, heart attacks, strokes and cardiac deaths.
Most statins must be taken at night, as most cholesterol is made while we sleep. The only statin which does not have to be taken at night is atorvastatin, which can be taken morning or night. Statins are more effective in reducing LDL cholesterol than other cholesterol medications.
How effective are statins?
A study published in the British Medical Journal in 2003 showed that on average, statins reduce LDL cholesterol by 1.8mmol/litre. This resulted in a 60 per cent reduction in the risk of cardiovascular events such as heart attacks, clots, and sudden cardiac death, and a 17 per cent reduction in the risk of stroke.
Which statin is best?
No major study has shown one statin to be significantly more effective than others. The CURVEs study in America in 1998 indicated that atorvastatin was more effective than other statins at lowering cholesterol and this was one of the major reasons that atorvastatin became the most prescribed statin in the intervening years and Lipitor became a ‘blockbuster’ drug for Pfizer.
However, the effectiveness of atorvastatin over other statins has since been somewhat challenged since. For example, another study published in the American Heart Journal in 2006 showed that there was no significant difference between atorvastatin and other statins (simvastatin and pravastatin) at reducing heart disease. A study published in the International Journal of Endocrinology and Metabolism in 2017 (study was on an Asian population) indicated effects of statins on lipid profile are dose-dependent and showed that rosuvastatin has the best effect on lipid profile.
However, overall studies indicate there is no real reason to recommend one statin over another. Atorvastatin has the benefit that it can be taken in the morning. The HSE recommends simvastatin as first choice on State PCRS schemes for cost reasons, however all generic statins have become similarly priced in Ireland in recent years with the advent of reference pricing by the HSE.
When should statins be prescribed?
In Ireland, over 20 per cent of adults are at risk of coronary heart disease due to high cholesterol. There is some controversy around who should be prescribed statins. The general guideline for people who have no previous heart problems is that they should be used if cholesterol is high (over 6mmol/litre) and there is a cardiovascular risk of greater than 20 per cent over the next 10 years.
Cardiovascular risk over 10 years is risk of having any cardiovascular event, such as stroke or heart attack, over the next 10 years. It depends on many factors, such as age, sex, weight, blood pressure, cholesterol, family history of heart disease, and whether a smoker or diabetic. For those who have already suffered a cardiovascular event, such as a stroke, statins are recommended if total cholesterol is over 3.5mmol/l. Guidelines state that they should be considered in all diabetic patients aged over 40. Statins are very frequently prescribed in the elderly, as elderly patients generally have a higher risk of heart disease.
Side-effects of statins
Like all medications, statins can cause side-effects. The most serious side-effect of statins is a muscle complaint called myalgia. It is characterised by muscle pain and weakness. If it occurs, the statin should be stopped, as it can lead to a potentially fatal condition called rhabdomyolysis. It is estimated that one-in-1,000 people using statins may suffer from myalgia and one-in-10,000 may suffer from rhabdomyolysis. Patients must report to their doctor immediately if suffering from muscle pain, tenderness or weakness while taking a statin. The myalgia from statins is reversible if the statin is stopped promptly.
Statins can also raise liver enzymes, which can lead to liver problems. It is very important to conduct a liver function test for those starting statins. Current guidelines are to get a liver function test before starting a statin, three months after starting, and again after 12 months.
Gastrointestinal effects (nausea, indigestion, constipation, diarrhoea, and flatulence) are the most common side-effects of statins. Headache, dizziness, and rash occur less frequently. Sleep disturbance can occur, although it seems to be more of a problem with simvastatin and atorvastatin. Most people who take statins have no problems and they are proven to save lives by preventing heart disease.
For those who have already suffered a cardiovascular event, such as a stroke, statins are recommended if total cholesterol is over 3.5mmol/l
Can co-enzyme Q10 reduce muscle problems from statins?
Statins can reduce naturally-occurring coenzyme Q10 in the body. Co-enzyme Q10 has a role in muscle cell energy production, so some studies have proposed that a co-enzyme Q10 supplement could reduce the risk of muscle-related side-effects. However, scientific studies to determine how effective coenzyme Q10 is in reducing statin-related muscle pain have mixed results. Some studies show a benefit, while other studies show no effect. So, as co-enzyme Q10 rarely has any side-effects, a trial to determine if it helps any potential muscle problems would do no harm.
Non-statin cholesterol medication
Statins are less effective than fibrates in reducing triglycerides. Fibrates are another type of cholesterol-lowering medicines but are rarely used nowadays mainly due to gastrointestinal side-effects such as nausea, ie, gemfibrozil (Lopid). Other non-statin drugs used to lower cholesterol include ezetimibe, which reduces the absorption of cholesterol and is used instead of a statin if a statin is not tolerated or in addition to a statin if a statin is not reducing cholesterol sufficiently.
PCSK9 inhibitors
PCSK9 inhibitors are a new class of cholesterol-lowering drugs that show excellent results in bringing down non-HDL levels in certain high-risk patients. They work by blocking a protein called PCSK9, which has a role in moderating cholesterol levels in the blood.
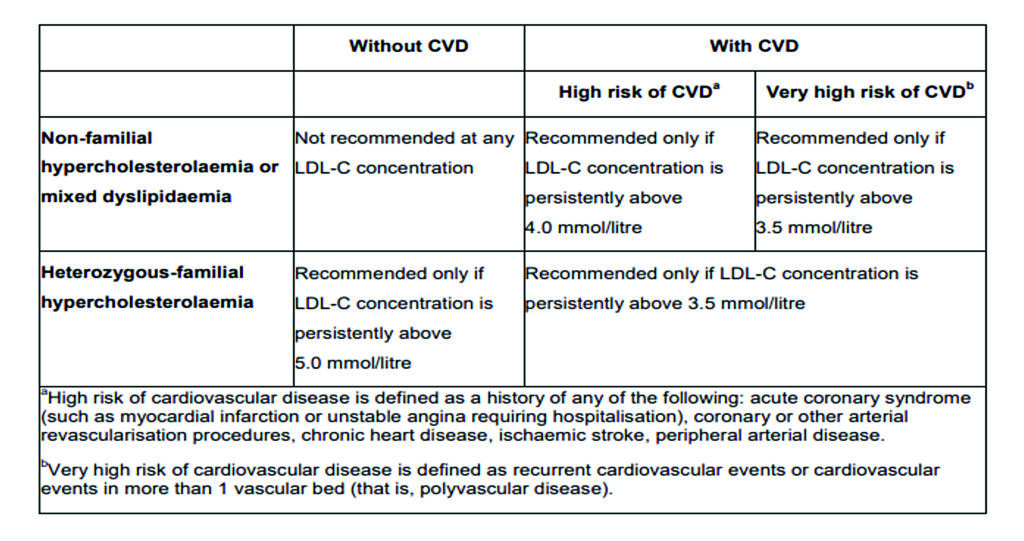
In June 2016, NICE recommended two PCSK9 inhibitor drugs for the NHS — Repatha (evolocumab) and Praluent (alirocumab) for treating certain patients with primary hypercholesterolaemia or mixed dyslipidaemia who cannot tolerate statins or who have reached the maximum statin dose without sufficient cholesterol reduction.
Researchers on the FOURIER trial investigating the effectiveness of evolocumab in the UK described it as “probably the most important trial result of a cholesterol-lowering drug in over 20 years”. Results showed a 59 per cent drop in cholesterol levels compared to placebo and a 15 per cent lower risk of cardiovascular events.
According to NICE, additional lipid-lowering therapies should be considered if:
- Target LDL-C level is not attained on statins alone, add ezetimibe and trial for at least three months.
- Target LDL-C level is still not attained, consider PCSK9 inhibitor, subject to NICE criteria in Table 1, in addition to existing lipid-lowering therapy.
PCSK9 inhibitors in Ireland
Repatha (evolocumab) and Praluent (alirocumab) are both licensed in Ireland. Repatha (evolocumab), for example, is a 140mg solution for injection in a Sureclick pre-filled pen and has been available under the High-Tech Scheme in Ireland from 1 July 2019. Specific criteria must be satisfied for a patient to be recommended for reimbursement of Repatha under the High-Tech Scheme.
The prescribing of Repatha under the High-Tech Scheme is confined to designated clinicians who have agreed to the terms of the HSE-Managed Access Protocol and have been approved by the HSE-Medicines Management Programme. The clinician must submit an online application for individual reimbursement approval for each patient. Applications for individual reimbursement approval will only be considered from approved clinicians. Pharmacists like myself have noticed a small number of high-risk patients with very stubbornly high cholesterol being prescribed PCSK9 inhibitors in the last two years under the high-tech scheme.
Other therapies
Omega 3s
High-strength omega 3 supplements such as Omacor are sometimes prescribed to lower triglycerides and are sometimes added to statin therapy when triglycerides are high. However, the HSE took omega 3 supplements off the PCRS reimbursement list for the GMS schemes (Medical Card and Drug Payment Schemes) due to the National Centre for Pharmacoeconomics (NCPE) indicating that evidence of their overall benefits was not strong enough to warrant the HSE paying for omega 3 supplements for the treatment of triglycerides.
For example, one study quoted by NICE indicated (for diabetic patients) that while Omacor reduced triglycerides in the blood of diabetic patients by 5.6 per cent, there was no reduction in estimated CVD risk. However, there is significant evidence of the benefit for the secondary prevention of myocardial infarction (MI) for up to four years after the patient’s first MI.
Lecithin
Lecithin reduces cholesterol by binding cholesterol and fats to water in the intestinal tract, hence reducing the absorption of cholesterol. Evidence indicates lecithin reduces LDL-cholesterol and can promote the HDL-cholesterol production. A study published in the Hindawi Journal of Cholesterol in 2010 suggested that soy lecithin-rich diets can be used as an adjunct in the treatment of hypercholesterolemia; however, no large enough study has yet been done, so further studies with a large number of patients should be done to find the ideal dose-response. A major source of lecithin is soy-bean oil. It can be purchased in powder or capsule form in pharmacies, health food stores, and supermarkets.
References: Available upon request
Disclaimer: Brands mentioned in this article are meant as examples only and not meant as preference to other brands.







