Eamonn Brady MPSI presents a clinical overview of diverticular disease and diverticulitis and how they affect the large intestine
Diverticular disease and diverticulitis are two closely-related digestive conditions that affect the large intestine (colon). Small bulges occur on the lining of the intestines; these pouches or bulges can become inflamed or infected, which leads to symptoms. Symptoms of diverticular disease include lower abdominal pain and bloating. Diverticulitis is more serious than diverticular disease and symptoms include more severe abdominal pain and a high temperature of 38ºC or above.
Diverticula
Diverticula (plural) is the medical term used to describe the small pouches that stick out of the side of the large intestine (colon). Diverticula are quite common and are associated with ageing. The pressure of hard stools passing through the large intestine that has become weakened with age causes the pouches to form.
Approximately 50 per cent of the population suffers from diverticula by the time they are 50 years old, and 70 per cent have diverticula by the time they are 80 years old. Most people with diverticula do not have any symptoms; this is known as diverticulosis.
Diverticular disease
One-in-four people who develop diverticula will experience symptoms such as abdominal pain. Having symptoms associated with diverticula is known as diverticular disease.
Diverticulitis
Diverticulitis describes infection that occurs when bacteria become trapped inside one of the pouches, leading to inflammation and triggering more severe symptoms. Diverticulitis can lead to serious complications, such as an abscess inside the intestine.
Symptoms of diverticular disease and diverticulitis
Diverticular disease
The most common symptom of diverticular disease is intermittent (stop-start) pain in the lower abdomen, mainly in the lower left-hand side. The pain is often worse when eating, or shortly afterwards. Passing stools and passing wind (flatulence) may relieve the pain. Other symptoms of diverticular disease include a change in normal bowel habits, such as constipation or diarrhoea (or episodes of constipation followed shortly by diarrhoea), bloating and rectal bleeding.
Diverticulitis
The main symptom of diverticulitis is a constant and severe pain. The pain usually starts below the navel (belly-button) before moving to the lower left-hand side of the abdomen. For genetic reasons, Asian people tend to develop diverticula in a different part of their colon, meaning the pain may occur in the lower right-hand side of the abdomen in Asian people. Apart from severe stomach pain, other symptoms of diverticulitis include a high temperature of 38ºC or above; nausea; vomiting; a frequent need to urinate; pain when urinating; constipation; and bleeding from the rectum.
When to seek treatment
It is important to get diverticulitis treated quickly. The sooner diverticulitis is treated with antibiotics, the lower the risk of complications developing. If a person has the symptoms of diverticular disease and the condition has previously been diagnosed, they do not usually need to contact their GP because the symptoms can be treated at home. If a person has not been diagnosed with the condition, they should contact their GP to rule out other conditions that have similar symptoms, such as irritable bowel syndrome (IBS) or ulcerative colitis.
Who does it affect?
Diverticular disease is one of the most common digestive conditions. Men and women are equally affected by diverticular disease and diverticulitis, although the condition is more likely to appear at a younger age (under 50) in men. Diverticular disease rates are high in Western countries, including Europe and North America, and low in African and Asian countries. Diet is thought to be the reason for this, explained by the fact that people in Western countries tend to eat less fibre in their diet compared to the diet of people in less-developed countries.
Causes
Diverticular disease
It is not known why only one-in-four people with diverticula develop symptoms of diverticular disease. Several factors have been identified that appear to increase the risk of developing diverticular disease, including:
- Smoking.
- Being overweight or obese.
- Having a history of constipation.
- Physical inactivity.
- Use of non-steroidal anti-inflammatory drugs (NSAIDs) type of painkillers, such as ibuprofen or diclofenac.
Diverticulitis
Diverticulitis is caused by an infection of one or more of the diverticula. It is thought that an infection develops when a hard piece of stool gets trapped in one of the pouches. This gives bacteria in the stool the chance to multiply and spread, triggering an infection.
Diagnosis
Diverticular disease can be difficult to diagnose from the symptoms alone because there are many other conditions that cause similar symptoms, such as IBS. As a first step, blood tests can rule out other conditions such as coeliac disease (abnormal immune response to gluten found mainly in wheat).
Colonoscopy
To confirm diverticula, the inside of the large intestine needs to be examined. This can be done with a colonoscopy. During a colonoscopy, a thin tube with a camera at the end (a colonoscope) is inserted into the rectum and guided into the colon. Before the procedure begins, a laxative is given to clear out the bowels. A colonoscopy is carried out under local anaesthetic, so it is not painful. A sedative can be given for relaxation if the person is uncomfortable.
Diverticulitis is caused by an infection of one or more of the diverticula
Barium enema x-ray
Another technique for confirming the presence of diverticula is a barium enema x-ray. Barium is a liquid that shows up on x-rays. It is used to coat the inside surface of organs that do not show up on x-ray, such as the colon. As with a colonoscopy, the person is given a laxative to clear out the bowels before having a barium enema x-ray. During the procedure, a tube is inserted into rectum. The barium liquid is squirted into the tube and up into the rectum. A series of x-rays are then taken.
Diagnosing diverticulitis
When a person has a previous history of diverticular disease, the GP will usually be able to diagnose diverticulitis from symptoms and a physical examination. A blood test may be taken because a high number of white blood cells indicate infection.
Further tests will be needed if there is no previous history of diverticular disease. This is to rule out other possible conditions, such as gallstones or a hernia. A barium enema x-ray may be used, as well as a computerised tomography (CT) scan. A CT scan may also be used if symptoms are particularly severe. This is to check whether the infection has spread to other parts of the body or a complication, such as an abscess, has occurred.
Treatment
Eating a high-fibre diet can help control symptoms. Some people will notice an improvement after a few days, although it can take around a month to fully feel the benefits. Most cases of diverticular disease can be treated at home. The over-the-counter (OTC) painkiller, paracetamol, is recommended to help relieve symptoms. NSAIDs, such as aspirin and ibuprofen, are not recommended because they irritate the lining of the stomach and can upset the stomach and increase the risk of internal bleeding.
Heavy or constant rectal bleeding occurs in about one-in-three cases of diverticular disease. This can happen if the blood vessels in the large intestine are weakened by the diverticula, making them vulnerable to damage. The bleeding is usually painless but losing too much blood can be potentially serious and patients may need a blood transfusion. Signs of heavy bleeding (apart from the amount of blood) include:
- Feeling very dizzy.
- Mental confusion.
- Pale, clammy skin.
- Shortness of breath.
In this situation, immediate medical attention is needed.
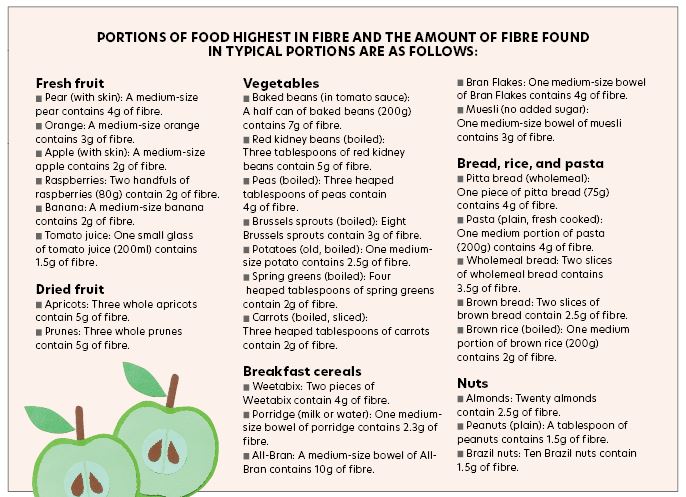
Fibre
Not eating enough fibre is thought to be a main reason why diverticula develop. Fibre makes stools softer and larger so that less pressure is needed by the large intestine to push stools out of the body. Eating low-fibre food produces small, hard stools. These are more difficult for the muscles of the large intestine to move and will cause the person to strain. The pressure of moving the hard, small pieces of stools through the large intestine creates weak spots in the outside layer of muscle. This allows the inner layer to squeeze through these weak spots, creating the diverticula.
People with diverticular disease are recommended to eat between 18g-to-30g of fibre daily. However, a more specific target may be required, depending on individual height and weight. Sources of fibre include:
- Fresh fruit such as peaches, oranges, pears, bananas, and apples.
- Vegetables such as baked beans, kidney beans, peas, broccoli, and cabbage.
- Dried fruit such as apricots and prunes.
- Nuts such as almonds, peanuts, and sunflower seeds.
- Breakfast cereals such as bran flakes.
- Brown versions of bread, rice, and pasta.
If fibre intake is low, it is recommended to gradually increase fibre intake over the course of a few weeks. This will help to prevent the side-effects associated with a high-fibre diet, such as bloating and flatulence. If these symptoms occur initially after increasing fibre intake, they will reduce after a few weeks as the intestines get used to increased fibre. Drinking plenty of fluids will help to prevent side-effects. Fibre supplements, usually in the form of sachets of powder that are mixed with water, are available from pharmacies, ie, Fybogel.
Diverticulitis treatment
Mild diverticulitis can be treated by a GP and hospital treatment will not be needed. A GP will prescribe antibiotics for the infection and paracetamol will ease the pain. Sticking to a fluid-only diet for a few days may be recommended until symptoms improve. This is because trying to digest solid foods may make symptoms worse. Solid foods can then be gradually re-introduced over a two- or three-day period.
Treatment at hospital
For severe diverticulitis, hospital treatment may be needed. Hospital treatment is recommended if:
- Unable to drink enough fluids to stay hydrated.
- Unable to take antibiotics by mouth.
- The pain cannot be controlled using paracetamol.
- General state of health is poor.
- Weakened immune system.
- GP suspects complications.
- Symptoms fail to improve after two days of treatment at home.
IV antibiotics are generally used, as well as an intravenous drip for hydration and nutrition for those admitted to hospital with diverticulitis. Most people start to improve within two-to-three days.
Surgery
In the past, surgery was recommended as a preventative measure for people who had two episodes of diverticulitis as a precaution to prevent complications. This is no longer the case, as studies have found that in most cases, the risks of serious complications of surgery (estimated to be around one-in-100) usually outweigh the benefits.
However, there are exceptions to this, such as:
- A history of serious complications arising from diverticulitis.
- Symptoms of diverticular disease from a young age (it is thought that the longer a person lives with diverticular disease, the greater the chances of having a serious complication).
- A weakened immune system.
Colectomy
Surgery for diverticulitis involves removing the affected section of the large intestine. This is known as a colectomy. There are two ways that a colectomy can be performed:
- An open colectomy, where the surgeon makes a large incision in the abdomen and removes a section of the large intestine.
- Laparoscopic colectomy — a type of keyhole surgery where the surgeon makes a few small incisions in the abdomen and is guided by a camera to remove a section of large intestine.
Open colectomies and laparoscopic colectomies are thought to be equally effective in treating diverticulitis and have a similar risk of complications. Laparoscopic colectomies have the advantage of having a faster recovery time, and they cause less post-operative pain.
Stoma surgery
In some cases, the surgeon may decide that the large intestine needs to heal before it can be reattached, or that too much of the large intestine has been removed to make reattachment possible. In such cases, stoma surgery provides a way of removing waste materials from the body without using all of the large intestine. Stoma surgery involves the surgeon making a small hole in the abdomen that is known as a stoma.
There are two ways that stoma surgery can be carried out: An ileostomy, where a stoma is made in the right-hand side of the abdomen. The small intestine is separated from the large intestine and connected to the stoma, and the rest of the large intestine is sealed. The person wears a pouch connected to the stoma to collect waste material.
A colostomy, where a stoma is made in the lower abdomen and a section of the large intestine is removed and connected to the stoma. As with an ileostomy, the person wears a pouch to collect waste material. In most cases, the stoma will be temporary and can be removed once the large intestine has recovered from the effects of the surgery. This will usually take at least nine weeks. If a large section of the large intestine is affected by diverticulitis and needs to be removed, the person may need to have a permanent ileostomy or colostomy.
Results of surgery
In general terms, surgery is usually successful, although it does not achieve a complete cure in all cases. Following surgery, an estimated one-in-12 of people will have a recurrence of the symptoms of diverticular disease and diverticulitis.
Complications
Complications of diverticulitis affect one-in-five people with the condition. Those most at risk of developing complications are younger people (under 50 years of age).
Abscess
An abscess inside the large intestine is the most common complication of diverticulitis. An abscess is a pus-filled cavity or lump in the tissue. Abscesses are usually treated with a technique known as percutaneous abscess drainage (PAD). A radiologist uses an ultrasound or CT scanner to locate the site of the abscess.
Fistula
A fistula is another common complication of diverticulitis. Fistulas are abnormal tunnels that connect two parts of the body together, such as the intestine and the abdominal wall or bladder. If infected tissues come into contact with each other, they can stick together. After the tissues have healed, a fistula may form. Fistulas can be potentially serious, as they can allow bacteria in the large intestine to travel to other parts of the body, triggering infections, such as an infection of the bladder (cystitis). Fistulas are usually treated with surgery to remove a small section of the colon that contains the fistula.
A fistula is another common complication of diverticulitis
Peritonitis
In rare cases, an infected diverticula splits, spreading the infection into the lining of the abdomen. An infection of the lining of the abdomen is known as peritonitis. Peritonitis can be life-threatening and requires immediate treatment with antibiotics. Surgery may also be required to repair any damage and to drain any pus that has built up.
Intestinal obstruction
If the infection has badly scarred the large intestine, the large intestine may become partially or totally blocked. A totally blocked large intestine is a medical emergency because the tissue of the large intestine will start to decay and eventually split, leading to peritonitis. A partially-blocked large intestine is not as urgent, but treatment is still needed. If left untreated, it will affect the ability to digest food. It will also cause considerable pain. In some cases, the blocked part of the large intestine can be removed during surgery. However, if the scarring and blockage is more extensive, a temporary or permanent colostomy may be needed.
References on request
Written and researched by Eamonn Brady (MPSI), owner of Whelehans Pharmacies in Mullingar