A Clinical Look At Menstrual Disorders, Including Symptoms And Treatment Options
WHAT IS MENSTRUATION?
Menstruation or menstrual period (commonly referred to as ‘period’ for short) is normal vaginal bleeding that occurs as part of the monthly cycle in women of reproductive age. Every month, the woman’s body prepares for pregnancy. If no pregnancy occurs, the uterus (better known as the womb) sheds its lining.
The menstrual discharge contains both blood and tissue FOCUS ON from inside the uterus that passes out of the body via the vagina. Periods usually start between ages of 11 and 14. ‘Menarche’ is the medical term to describe the onset of first period. Periods continue until menopause, which occurs for most women in their late 40s or early 50s. Periods last between three-to-five days per month.
In addition to bleeding from the vagina, women may experience:
- Abdominal or pelvic cramping type pain.
- Tender and sore breasts.
- Lower back pain.
- Mood swings and irritability.
- Headache and fatigue.
- Food cravings.
Premenstrual syndrome (PMS for short) is a group of symptoms that start before the period. PMS can include emotional and physical symptoms. Most women do not experience major problems with periods. However, some women experience menstrual disorders of varying degrees of severity.
Menstrual disorders can include:
- Menorrhagia.
- Endometriosis.
- Postponement of menstruation.
- Dysmenorrhoea.
In the first section of this article (Part 1), I briefly discuss background and treatment options for some of the most common menstrual disorders. However, I will focus in more detail on dysmenorrhoea, including its causes and treatment options, for the main part of this article.
PART 1: COMMON MENSTRUAL DISORDERS MENORRHAGIA (BRIEF OVERVIEW)
Menorrhagia is menstrual bleeding that is prolonged (more than seven days) and abnormally heavy.
TREATMENT OPTIONS (IN BRIEF)
To stop acute bleeding: Norethisterone 5mg, orally, three times a day for 10 days. For long-term control: If contraception required:
- First choice: Combined oral contraceptive, orally, daily.
- Second choice: Progesterone intrauterine system (Mirena).
For long-term control: If contraception not required:
- First choice: Tranexamic acid 1,000mg, orally, three times a day for up to four days after period has begun.
- Second choice: NSAID such as ibuprofen, mefenamic acid or naproxen during the period. Trial lower doses of NSAIDs initially, only increasing to higher doses if more relief is required. NSAIDs should be prescribed for the shortest possible duration, ie, three or four days. NSAIDs are best avoided if the patient has cardiovascular, gastrointestinal, or renal risk factors.
NSAIDs are best avoided if the patient has cardiovascular, gastrointestinal, or renal risk factors
ENDOMETRIOSIS (BRIEF OVERVIEW)
Endometriosis is a condition caused by tissue that normally only lines the uterus starting to grow in other places, including the ovaries, Fallopian tubes, and stomach. In more medical parlance, endometriosis is defined as the presence of ectopic endometrial tissue in the peritoneal cavity.
Endometriosis can lead to symptoms including:
- Painful periods.
- Pain at time of ovulation.
- Dyspareunia (pain during or after sex).
- Heavy or irregular bleeding.
- Pain in the pelvic area, lower back, or legs.
- Pain during bowel movements or urination.
- Nausea.
- Fatigue.
Adenomyosis (the infiltration of the myometrium by endometrial cells) often occurs with endometriosis and can exacerbate pain during menstruation. The myometrium is the middle layer of the uterine wall and is made up of uterine smooth muscle cells and vascular tissue. Its main function is to induce uterine contractions.
Where endometriosis requires drug treatment, a progestogen (ie, norethisterone) administered on a continuous basis is an option. For severe endometriosis, progestogen and/or a synthetic progestogen (ie, dydrogesterone) can be given alone, on a cyclical basis or in conjunction with an oestrogen.
If contraceptive required:
Treatment option is an oral combined contraceptive daily.
If contraception NOT required:
- First choice: Norethisterone 10mg, orally, daily for four-to-six months; start on day five of menstrual cycle; increase dose to 20-to-25mg daily (in divided doses) if spotting occurs, then reduce once bleeding has stopped.
- Second choice: Dydrogesterone 10mg, orally, two or three times a day; take continuously.
POSTPONEMENT OF MENSTRUATION (BRIEF OVERVIEW)
While postponement of menstruation is not a ‘menstrual disorder’ like menorrhagia, endometriosis or dysmenorrhoea, many women at some stage decide to postpone periods on a temporary basis for reasons like life events, such as getting married or going on holidays, or for medical reasons, such as period pain.
Options to postpone period:
- Norethisterone 5mg, orally, three times a day. Start three days before anticipated onset of period. Menstruation will occur 48 hours after treatment finishes;
- Or medroxyprogesterone 10mg, orally, daily for seven-to-10 days.
PART 2: FOCUS ON DYSMENORRHOEA DYSMENORRHOEA
Dysmenorrhoea is defined as monthly painful cramps at the time of menstruation that require treatment for pain to allow normal daily activities. Dysmenorrhoea can be either primary or secondary.
PRIMARY DYSMENORRHOEA
Primary dysmenorrhoea is painful periods not associated with another identifiable pelvic condition or disease. It is more common in the years after menarche (first period). Primary dysmenorrhoea peaks between the ages of 20 and 24 years and decreases from there on.
It affects 40- to-50 per cent of young women to a lesser or greater degree. Between 15-to-30 per cent of young women suffer from severe primary dysmenorrhoea, which limits activity and causes missed school and work days.
and secondary dysmenorrhoea, Prescribing in Practice, Prescriber Magazine, November 2017
Primary dysmenorrhoea generally starts within a year of menarche, which correlates to when ovulatory cycles first occur. If dysmenorrhoea presents more than a year after menarche, it is more likely to be secondary dysmenorrhoea.
Risk factors for primary dysmenorrhoea include early age starting periods (ie, less than 12), low body mass index, and a family history of dysmenorrhoea.
The pain associated with primary dysmenorrhoea tends to be crampy and spasmodic in nature and tends to start a few hours after the onset of menstrual flow, and peaks 24-to-36 hours into the period. It is rare for the pain to last for more than two-tothree days, and other symptoms can include backache, nausea, vomiting and diarrhoea.
PATHOPHYSIOLOGY
Primary dysmenorrhoea is caused by the excessive secretion of prostanoids, including prostaglandins. During the period, prostaglandin’s role is to trigger muscles in the uterus to contract, which causes the uterus to expel its lining. However, many young women are prone to higher levels of prostaglandins, which causes more severe menstrual cramps, and severe contractions may constrict the blood vessels around the uterus, thus reducing uterine blood flow, leading to hypoxia (low oxygen levels) and pain.
Other symptoms accompanying primary dysmenorrhoea, such as nausea, vomiting and diarrhoea, are also typical of excess prostaglandins. Prostaglandins are mediators of inflammatory and anaphylactic reactions, so while they have a key role, too much can promote inflammation, which leads to symptoms of primary dysmenorrhoea.
SECONDARY DYSMENORRHOEA
Secondary dysmenorrhoea is a consequence of another condition or disease affecting the pelvic area. It typically affects women from their 30s upwards and is associated with other symptoms, such as dyspareunia (painful sexual intercourse), dyschezia (painful defecation), and disturbances of the menstrual cycle. The commonest cause of secondary dysmenorrhoea is endometriosis. I gave a brief overview of endometriosis earlier in this article.
OTHER CAUSES OF SECONDARY DYSMENORRHOEA
Secondary dysmenorrhoea may be caused by pelvic infection that can lead to adhesions surrounding the ovaries that can obstruct/block the Fallopian tubes, leading to hydrosalpinges. Hydrosalpinges are blocked or severely compromised Fallopian tubes that significantly reduce fertility and need an operation to reverse; however, the success rate of operations to reverse hydrosalpinges is poor. Fibroids are another cause of dysmenorrhoea, as they cause uterine enlargement and are associated with menorrhagia (menstrual bleeding that lasts longer or is heavier than normal), leading to dysmenorrhoea. Uterine fibroids are non-cancerous growths on the uterus that are common during child-bearing years. Uterine fibroids do not increase risk of uterine cancer and rarely develop into cancer. Many women have no symptoms from fibroids, however if fibroids cause severe menorrhagia or dysmenorrhoea, then treatment such as surgical options may be required, ie, surgical removal of fibroids. Other abnormalities of the endometrium (lining of the uterus) include polyps that can cause menstrual cycle disturbances and pain during menstruation. There are rarer causes of dysmenorrhoea, such as cervical stenosis, which is narrowing of the passageway of the cervix (lower part of the uterus).
Uterine fibroids do not increase risk of uterine cancer and rarely develop into cancer
DIAGNOSIS OF DYSMENORRHOEA
As mentioned earlier, age of onset is the key to distinguishing between primary and secondary dysmenorrhoea. Primary dysmenorrhoea affects younger women, starting soon after onset of menstruation. The pain is confined to the time of month and only lasts two-tothree days. Secondary dysmenorrhoea mainly affects older women, with pain commencing prior to the onset of bleeding and continuing throughout. Secondary dysmenorrhoea is associated with secondary effects of other underlying conditions, such as dyspareunia (pain during and after sexual intercourse) and dyschezia (painful bowel movements). For primary dysmenorrhoea, examinations will find no clinical problem in the uterine and general pelvic area, while clinical examinations for secondary dysmenorrhoea can often find a significant clinical problem that is the underlying cause of dysmenorrhoea. The uterus can be enlarged in women with fibroids, and pelvic tenderness can manifest as discomfort or pain with even a gentle-touch examination by the clinician in women with pelvic inflammatory disease. Transabdominal ultrasound is an alternative examination method, especially in the likes of teenagers who are less comfortable with physical examination. Pelvic ultrasound is often the first step in investigating causes of dysmenorrhoea and modern advances in ultrasound allow the clinician to identify the likes of endometriosis, adenomyosis (condition where the inner lining of the uterus breaks through the muscle wall of the uterus), uterine fibroids and congenital uterine anomalies, all of which are causes of secondary dysmenorrhoea.
TREATMENT
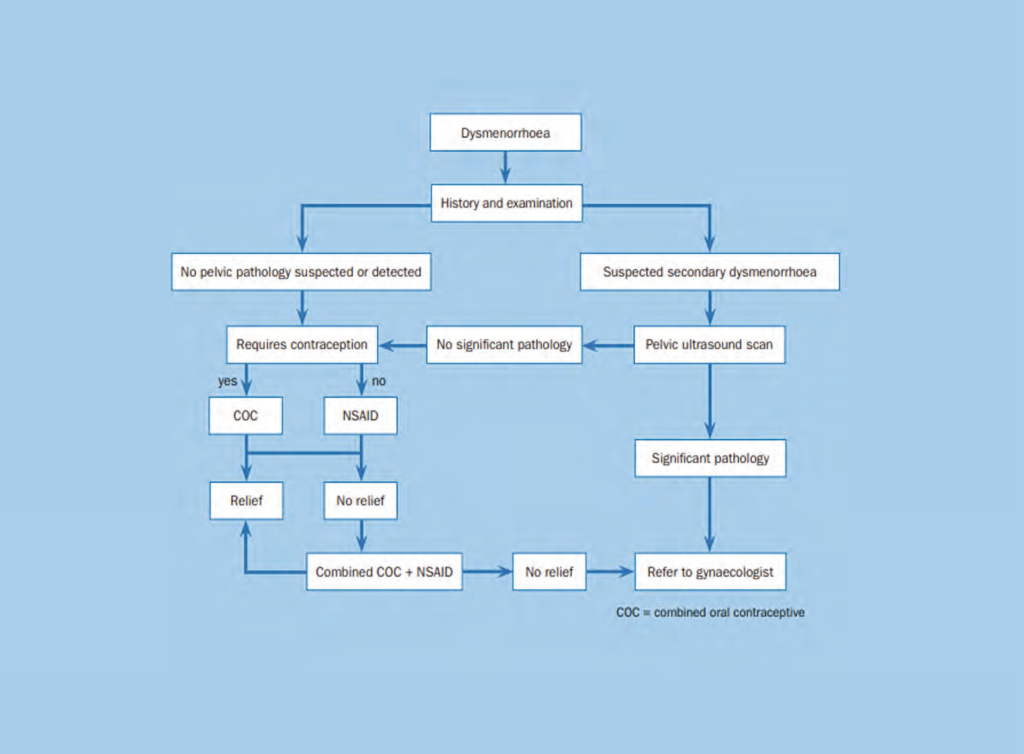
A treatment pathway for women presenting with primary or secondary dysmenorrhoea in primary care is shown in Figure 1.
NSAIDs
Many NSAIDs (non-steroidal anti-inflammatory drugs) are effective at relieving menstrual pain in dysmenorrhoea, with the exception of aspirin. Studies have shown 45-to-53 per cent of women taking NSAIDs for dysmenorrhoea had moderate or excellent pain relief compared with 18 per cent for those taking placebo. NSAIDs have been proven to allow continuation of normal daily activities and reduce absenteeism from school and work compared to placebo for dysmenorrhoea. There is little evidence of superiority of one NSAID over another. NSAIDs are associated with significant side-effects, such as stomach irritation, however the three-day regimen used to treat primary dysmenorrhoea rarely causes side-effects; side-effects from NSAIDs are more associated with more continual or long-term use and gastrointestinal side-effects, with irritation of the stomach lining being the most common. When released on the market over 20 years ago, COX-2 inhibitors (ie, etoricoxib) were thought to be potentially more effective than more traditional COX-1 selective agents (ie, naproxen) for dysmenorrhoea; however, it has been proven that COX-2 inhibitors are not superior to COX-1 selective agents in terms of pain relief. In relation to COX-2 inhibitors versus COX-1 inhibitors, COX 2 inhibitors have less GI side-effects, but this must be balanced against the higher risk of cardiovascular side-effects with COX- 2 inhibitors versus COX-1 inhibitors.
Oral contraceptives
Contraceptives suppress ovulation, which improves symptoms of dysmenorrhoea. Inhibition of ovulation and reduced volume of endometrium during menstruation reduces the volume of prostaglandins produced, thus relieving menstrual cramps and menstrual pain. The combined oral contraceptive can also be taken continuously to reduce the number of cycles the patient goes through. Evidence shows that even very low-dose combined oral contraceptive preparations are effective in treating dysmenorrhoea. Combined oral contraception is also available as transdermal skin patches and vaginal rings. Combined oral contraception has shown in clinical trials to give significant pain relief compared to placebo for primary dysmenorrhoea.
Intrauterine devices
The Mirena coil, which is a levonorgestrel- releasing intrauterine system for contraception, has been proven to give improved pain scores and reduced menstrual flow in women with endometriosis and adenomyosis. By contrast, the copper IUS is associated with increased menstrual pain, so is best avoided where dysmenorrhoea is an issue. A smallerframe levonorgestrel-releasing intrauterine system (Jaydess) is an option for younger women who have not yet given birth to a child (nulliparous women).
Dydrogesterone
Another option for dysmenorrhoea in women who do not require contraception is the synthetic progestogen called dydrogesterone (Duphaston) at a dose of 10mg twice a day from day five to day 26 of the menstrual cycle.
Contraceptives suppress ovulation, which improves symptoms of dysmenorrhoea
OTHER PHARMACOLOGICAL TREATMENTS
Drugs that cause myometrial relaxation (ie, relax uterine muscles) may be considered to relieve primary dysmenorrhoea. However, these drugs are not licensed for this use and therefore should only be prescribed by specialists in women’s health where all other treatment options have failed. Nitric oxide is more effective when compared with placebo for pain relief. However, the glyceryl trinitrate (GTN) patch is less effective when compared to diclofenac and has more side-effects, such as headache. Similar results have been obtained with the calcium channel blocker nifedipine for pain relief (ie, less effective and more side-effects compared to diclofenac). Beta2-agonists (ie, terbutaline inhaler or nebuliser) have also been trialled to treat dysmenorrhoea, however they were shown to have low efficacy as well as significant side-effects, meaning their use for dysmenorrhoea is not recommended.
NON-PHARMACOLOGICAL TREATMENTS
Many non-pharmacological treatments for dysmenorrhoea have been trialled. Transcutaneous electrical nerve stimulation (TENS) has been shown to have little benefit in reducing menstrual pain. A meta-analysis on the effectiveness of acupuncture in the treating of primary dysmenorrhoea published in Cochrane in 2006 gave conflicting results when compared to placebo and diclofenac. Acupuncture has the obvious advantage of a favourable adverse event profile compared to NSAIDs, but more studies are needed to prove its benefits for dysmenorrhoea. While dietary supplements have been examined for effectiveness in treating dysmenorrhoea, none have shown significant effect. High-dose vitamin D supplementation showed some promise in trials, but more research is required. The benefit of spine manipulation and herbal medicine remains inconclusive due to poor-quality clinical trial data so again, more research is needed.
WHEN TO REFER
Referral from primary care to secondary care (ie, from a GP to a women’s health specialist/gynaecologist) should occur on the detection of endometriosis, adenomyosis and fibroids. It has been reported that 50-to-70 per cent of teenagers who do not respond to the likes of NSAIDs and the combined oral contraceptive pill have pelvic endometriosis, which requires referral to a specialist.
References: Available upon request Disclaimer: Brands mentioned in this article are meant as examples only and not meant as preference to other brands.
CONTRIBUTOR INFORMATION
Written and researched by Eamonn Brady (MPSI), owner of Whelehans Pharmacies in Mullingar Tel 04493 34591 (Pearse St) or 04493 10266 (Clonmore). www. whelehans.inet. Eamonn specialises in the supply of medicines and training needs of nursing homes throughout Ireland. Email ebrady@whelehans.ie