Eamonn Brady MPSI provides an overview of some of the more common foot conditions that present in the pharmacy
In this article, I discuss three distinct subjects relating to foot problems that pharmacists encounter regularly. In this article I will discuss:
- Fungal nail infection.
- Flat feet.
- Foot care for older people.
Fungal nail infections
Fungal nail infection affects at least 3 per cent of the population at any one time. Fungal nail infections are four times more prevalent in toenails than fingernails. It is rare in children and affects men more than women and increases with age.
Symptoms
The nails become thickened and discoloured, usually a yellow colour, but can turn black, white, or green. Fungal nail infection is generally not painful, and most people seek treatment for cosmetic reasons, as they feel it looks embarrassing. The nail can become brittle. If not treated, surrounding skin can become scaly and discoloured (white/yellow) and it can cause pain on the nail bed.
The two treatment options are oral antifungals or topical antifungals, ie, nail paint
Causes
Several types of fungus can cause nail infections. Ninety-three per cent of fungal nail infections spread from nearby fungal skin infections, including athlete’s foot (tinea pedis) and ringworm (tinea corporis). Other organisms
that are responsible for fungal nail infections include yeasts and moulds. Fungal nail infection often spreads from nail-to-nail.
Risk factors:
- Hot, sweaty feet (ie, during exercise) or warm/humid environment.
- Nail damage caused by the likes of false nails, etc.
- Immunocompromised patients, diabetics and those with psoriasis.
Athlete’s foot
It is estimated that 20-to-30 per cent of athlete’s foot cases lead to a fungal nail infection. Athlete’s foot mostly infects skin between the toes, causing redness, flakiness, and an intense itch. A warm and damp environment is ideal for athlete’s foot to develop, ie, sweating.
Treating a fungal nail infection
A doctor may decide to send nail clippings to a lab to confirm if it is a fungal nail infection rather than another cause, like psoriasis. The two treatment options are oral antifungals or topical antifungals, ie, nail paint. Oral antifungals work quicker than topical options. Treatment will bring the nail back to its original appearance in about half of cases. Sometimes the treatment will clear the infection but not bring the nail back to its original appearance (20 per cent of cases). Topical antifungals like creams and sprays work well for fungal skin infections but are not effective for fungal nail infections, as they are wipe or wash off easily.
Oral antifungals
Terbinafine and itraconazole are two oral antifungal options. Terbinafine is the most effective of the oral antifungal medicines, but still takes months to work. Toenails are harder than fingernails, so take longer to treat. A fingernail can need six months of treatment, and a toenail up to 12 months. The usual adult dose of terbinafine is 250mg daily for between six weeks and three months for fingernails, and for three-to-six months for toenails.
Visible improvement is generally after two months for fingernails and three months for toenails. Stopping too early risks the fungal infection returning. Oral antifungals will clear fungal skin infections too. Possible but rare side-effects of oral antifungals include headache, itching, nausea, taste disturbance and diarrhoea. They should be avoided in patients with liver problems and, if the patient shows signs of liver problems (ie, jaundice, nausea, vomiting, dark urine), they should be stopped.
Antifungal nail paint
Nail paint is not as effective as oral medication. It works better if the infection is only at the end of the nail. A fingernail can take six months’ treatment, and a toenail as much as 12 months. Amorolfine nail lacquer can be prescribed by a GP and since 2012, amorolfine has become available over-the-counter in pharmacies without the need for a prescription after consultation with a pharmacist.
Flat feet
During childhood, usually between the ages of three and 10, a space develops on the inner side of our feet where the bottom of the foot is off the ground. These are referred to as the ‘arches’ of our feet. The height of this arch varies. People with a low arch or who have no arch are classified as having flat feet. Sometimes this is referred to as having ‘fallen arches’, though this term is misleading, as most with ‘fallen’ arches actually have a low arch.
Causes
Flat feet can run in families, and both feet are usually affected. Occasionally, flat feet are due to a problem in the
way the foot forms in the womb. For example, a joint may be misformed or two or more bones may fuse together. In these situations, the feet are stiff and flat, and the problem is usually noticeable during childhood.
Another form of the problem is when the foot tends to roll inwards too much while standing or walking. This can be due to weak ligaments in the heel joint or at the base of the big toe, which can cause excessive rolling-in of the foot. Muscle imbalances and associated altered alignment further up the kinetic chain, such as in the knee, hip and lower back, can also contribute to this flat foot presentation.
‘Pronation’ of the foot is another term for rolling of the foot, thus an ‘over-pronated foot’ is a term for excessive rolling of the feet. Regular rolling-in of the middle of the foot causes the heel and the front of the foot to point outwards more than usual. A common method of telling if a person has developed over-pronated feet is to stand up on tiptoes, or by pushing the big toe up as far as it can go. If an arch appears, the foot is sufficiently flexible and there are no issues.
While over-pronated feet usually develop in childhood, there are times when flat feet develop when the person gets older. Flat feet may develop due to a ruptured tendon (a ruptured tibialis posterior tendon, which is rare), tear of the spring ligament (also rare), arthritis, nerve damage due to diabetes, or injury which leads to stiffness and distortion of the joints of the feet. Conditions of the nervous system or muscles, including cerebral palsy, spina bifida or muscular dystrophy, can cause flat feet, as they can cause muscle weakness or lack of movement in the muscles.
These conditions lead to the feet becoming stiff, which get worse as the condition develops.
Other contributing factors can include shoes which limit toe movement, such as high heels (walking barefoot may have a protective effect). Tight Achilles tendon or calf muscles can also make a person more prone to flat feet. Obesity also can contribute to flat feet.
Tight Achilles tendon or calf muscles can also make a person more prone to flat feet
Are flat feet hereditary?
It is estimated that about 20 per cent of the population suffer from flat feet, but only a small proportion of these are born with flat feet. Some cases of flat feet are hereditary. Flat feet that run in families are due to feet being shaped in an abnormal way or over-pronation of feet in those with lax joints.
When is treatment needed?
Most flat feet cases do not cause any problem, so no treatment is needed. Reasons to look for treatment include:
- Pain (not eased by any type of footwear). Flat feet do not usually cause pain but can put strain on muscles and ligaments (connect two bones together at a joint). This can cause leg pain when walking. Pain from flat feet can occur in a number of areas, including inside the ankle, at the arch of the foot, the outer side of the foot, calf, knee, hip or back.
- Wearing out shoes quickly.
- Feet appear to be getting flatter.
- Feet tire easily.
- Swelling on the inside bottom of feet.
- Feet are stiff.
- Lack of feeling in the feet or weakness.
There is some evidence that flat feet can contribute to osteoarthritis of the feet and that flat feet can reduce the shock-absorbing qualities of the feet, leading to back problems and back pain.
Treatment
No treatment is required if flat feet do not cause problems. Well-fitted shoes, especially extra-broad fitting types of shoes, can help. For people suffering from over-pronated feet, a special insole that prevents feet rolling over too much can ease the problems. These specialised insoles can be advised by a chiropodist or a physiotherapist, who are specialists in assessing for and measuring the specialist insoles.
These insoles are also called orthotics. If pain occurs, rest, ice, and over-the-counter non-steroidal anti-inflammatories, or NSAIDs (ie, Ibuprofen) can give relief; however, painkillers should only be a temporary solution and the cause of the problem should be identified and corrected.
Children with an abnormal foot that has not developed properly may require an operation to straighten the foot or to separate bones that have fused. Operations are rarely needed, as these are rare causes of flat feet in children. Most children with flat feet have a mobile form of flat feet, which generally does not need treatment, or if treatment is needed due to pain or excessive wear of shoes, an insole is often sufficient to rectify the problem.
Flat feet that develop due to a disorder of the nervous system may require specialised insoles, shoes, or braces to support feet or legs. In some of these cases, an operation will be required to straighten the feet. Flat feet due to ruptured tendons or arthritis may need to be treated with painkillers and an insole initially. Again, an operation may be required to straighten the foot in these cases.
Other actions that can help include wearing footwear with lower heels and wide toes, losing weight if appropriate, and doing appropriate exercises that strengthen muscles in the feet, which can include walking barefoot, exercises called toe-curls (flexing the toes) and heel-raises (standing on tiptoes).
Heel cord stretching exercises
These stretch and lengthen the Achilles tendon and posterior calf muscles. A chartered physiotherapist is best for advising on appropriate exercises.
How to do:
Stand facing a wall with hands on the wall at about eye level. Put the leg needing stretching about a step behind the other leg. Keeping the back heel on the floor, bend the front knee until a stretch is felt in the back leg. Hold the stretch for 15-to-30 seconds. Repeat two-to-four times. Aim to do this exercise three-to-four times a day.
Children
As noted earlier, most cases of flat feet in children do not need treatment. In the past, it was thought that flat feet in children required treatment with specialised shoes, insoles, or callipers to prevent problems as they grew into an adult. This is now recognised as being incorrect and these treatments are ineffective. It is now recognised that children treated in this way will end up the same as similar children who are not treated.
Additionally, children often refuse to wear the shoes, insoles, or callipers. No evidence shows treating flat feet in childhood prevent problems in later life and most of these children do not develop problems when they reach adulthood, even if left untreated. The only reason to seek treatment for a child’s feet would be if they cause pain or their shoes wear out excessively. In these cases, specialised insoles measured professionally by a chiropodist or physiotherapist will help.
Foot care in the older person
Feet consist of skin, bones, muscles, tendons, ligaments, nerves, and blood vessels. Feet are one of the most important organs of the body. Put simply, our feet allow us to get around and are constantly in use. Our feet allow us to balance our body effectively in walking, running, working, dancing and in many other daily activities. Our feet are vulnerable to repetitive mechanical stress and skin irritations due to repetitive daily usage. Foot problems get more common as we get older, as years of use start to take their toll and medical problems such as diabetes, arthritis and poor circulation can also cause foot problems.
Common foot problems in the older person
Common foot problems in the older person include dry and hard skin, corns, callouses, blisters due to friction, ingrown toenails, foot deformity (from birth or due to conditions like arthritis), fungal infection such as athlete’s foot and fungal nail infection, circulation problems, and verrucae.
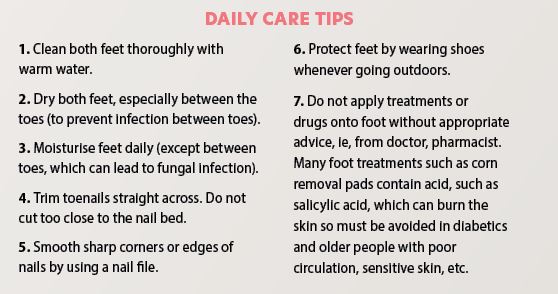
These problems are usually caused by inappropriate or inadequate foot care, mechanical causes (often due to inappropriate footwear), infection and underlying medical conditions, ie, diabetic neuropathy, or congenital foot deformity such as flat feet, etc. Many of these foot problems can be prevented through proper daily care.
Daily inspection
- Inspect feet for skin colour, dryness, swelling or tenderness.
- Look out for blisters, cracks, sores, ulcers, corns, and any ingrown toenails.
- Report any unusual sensations, such as tingling, lack of feeling or pain.
- If there is joint pain or deformity, prompt treatment is important
Selection of shoes and socks
Socks
- Use cotton socks, as they can absorb sweat.
- Change socks daily.
Shoes
Here are some tips for making sure shoes fit:
- Shoe size may change with age, so always have feet measured before buying shoes. The best time to measure feet is at the end of the day when feet are largest.
- Most people have one foot that is larger than the other; fit the shoe to the larger foot.
- Do not buy shoes by the size without trying them on first. The size marked inside the shoe may not fit.
- Walk in the shoes to make sure they feel right.
- Choose a shoe that is shaped like your foot. Styles like high heels or pointed toes can hurt feet.
- Stand up when trying on shoes to make sure there is about ½ inch between the toe and the end of the shoe.
- Make sure the ball of foot fits comfortably into the widest part of the shoe.
- Do not buy shoes that feel too tight and hope that they will stretch.
- The heel of the shoe should not slide up and down on the heel when walking.
- The upper part of the shoes should be made of a soft, bendable material to match the shape of the foot.
- Soles should give solid footing and not slip. Thick soles cushion feet when we walk.
- Low-heeled shoes are more comfortable, safer, and less damaging than high heels.
Be more active
Walking, dancing, swimming, and cycling are good and easy on the feet. Avoid hard-on-the-feet activities like running and jumping. Do a short warm-up and cool-down before and after exercise.
Chiropodist
A chiropodist assesses, diagnoses and treats diseases and abnormalities of the feet and lower limbs. A chiropodist can significantly improve a person’s quality of life by alleviating painful symptoms and promoting and maintaining mobility.







