Eamonn Brady MPSI provides a clinical overview of treating coughs, colds and flu in the pharmacy
There is no cure for a cold or influenza (flu), as they are caused by viruses, but the symptoms can be relieved so that they are not noticeable. These symptoms include runny/blocked nose, sneezing/coughing, aches and pains, high temperature and sore throat. The flu comes on suddenly, whereas a cold develops over several hours.
Flu is a much more ‘hard-hitting’ illness than a cold and will usually leave the sufferer confined to bed for a few days (more about flu symptoms later in this article).
The symptoms of a cold, while unpleasant, usually allow the sufferer to continue his or her normal daily activities, although with Covid-19 in our community, movements must be restricted until Covid-19 is ruled out. Symptoms of a cold are generally confined to the head, while a patient with the flu will feel sick all over. The treatment is the same for each condition, regardless. Colds and flu generally last for about seven days at most and need no specific treatment other than painkillers for aches, pains and temperature and simple measures, such as decongestant rubs or vaporisers. Antibiotics are of no benefit.
Covid-19 must always be assumed
Covid-19 has complicated things, as when people get cold- or flu-like symptoms, it first must be considered whether it is Covid-19. People should phone their GP (Covid-19-related GP phone consultations are free of charge) and their GP will advise if they should get a Covid-19 test. If getting a test, the person should self-isolate until they get a negative result. Even if the Covid-19 result is negative, the person should still restrict movements until 48 hours after the cold/flu-like symptoms ease.
Covid-19 is a coronavirus, like the common cold, but the symptoms can be a lot more severe. While the symptoms of influenza can be like Covid-19, influenza is a completely unrelated virus to Covid-19.
For this article, I will concentrate on colds and flus (rather than Covid-19), but for those who contract Covid-19 and are lucky enough to have mild symptoms, the treatment of the symptoms like high temperature and cough are the same as to treat colds and flus. Anyone who develops breathing difficulties with Covid-19, especially those in more vulnerable categories, must get medical advice from their GP promptly.
Cold and flu treatment
The age of the patient will influence your choice of products. Runny nose and congestion are both treated by decongestants. Sneezing is treated by an antihistamine. A cough may be due to irritation or to post-nasal drip. An expectorant mixture can help. Headaches are due to inflammation of the sinuses and nasal passages and muscular or joint pain is common — this will need a painkiller.
Sinus pain worsens on leaning forward or lying down and may develop into an infection. High temperature is more common in the flu than with a cold — paracetamol is very useful to bring down a high temperature. A sore throat is usually the first sign of a cold, and one of the common OTC sore throat lozenges will help.
Precautions
Many cold and flu remedies contain several drugs, so anyone on prescription medication should speak to their pharmacist. Anyone who is pregnant, has heart disease or lung disease or the very young or old should also be seen by the pharmacist.
So, for example, if someone suffers from high blood pressure, it is best to avoid many cold and flu remedies which contain decongestants, as these products tend to raise blood pressure.
Asthmatics and people with stomach complaints such as stomach ulcers should avoid products which contain aspirin and non-steroidal anti-inflammatories (NSAIDs) like ibuprofen. This is because aspirin and NSAIDs can trigger asthma attacks in some asthmatics and irritate stomach ulcers. There is a vast number of preparations available for the treatment of cold and flu symptoms, some of which are combination preparations and may be capable of treating many symptoms at once.
Dry cough mixtures contain ingredients such as pholcodeine, codeine and dextromethorphan. Dry cough mixtures come in drowsy or non-drowsy versions
Cough
Essentially, there are two types of cough — a DRY or a CHESTY cough. During a cold, a cough is often caused by a nasal drip irritating the back of the throat. Chesty coughs occur when mucus (also called phlegm or catarrh) builds up in the airways, and the cough occurs so that the body can clear the mucus. Chesty cough mixtures with an expectorant, like guaifenesin or carbocisteine, liquefy the catarrh so that it can be coughed-up easier. There are other cough mixtures that cause drowsiness which can be used at night to help sleep. Sugar-free versions of cough mixtures are available for diabetics.
Dry cough mixtures contain ingredients such as pholcodeine, codeine and dextromethorphan. Dry cough mixtures come in drowsy or non-drowsy versions. There are also cough mixtures available that contain decongestants, which can be effective with a congested head as well as a cough.
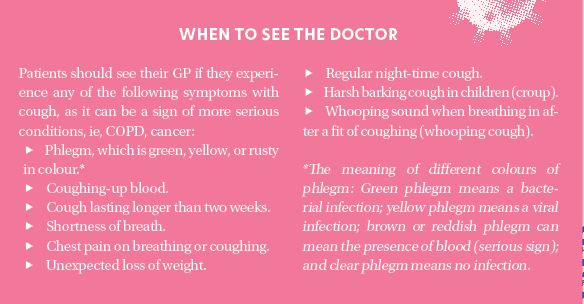
Self-help for coughs
Stop smoking
If you are determined to continue smoking, at least stop for the duration of the cough. This gives the lungs an opportunity to try to clear the infection. When you stop smoking, you will find you cough more for a few weeks as your lungs clear the tar that coated your lungs while you smoked.
Steam inhalations
Steam inhalations can be useful, particularly in productive (chesty) coughs. Simply putting hot steaming water (not boiling) in a basin, putting a towel over one’s head and inhaling the steam can accelerate the clearing of catarrh. The steam helps to liquefy lung secretions and the warm, moist air is comforting. Adding a little eucalyptus to the steaming water is a favourite of some people.
Increase fluid intake
A high fluid intake helps to hydrate the lungs and hot drinks can have a soothing effect.
Could the cough be due to blood pressure medication?
A type of blood pressure medication can cause a persistent dry cough in some people. The class of drug that causes this cough is ACE inhibitors. Examples include ramipril, perindopril, and lisinopril. About 10-to-15 per cent of people who use this class of blood pressure medication experience a dry cough. The incidence of cough appears to be higher in women. It is a persistent dry cough which is worse when lying down and generally does not start for 24 hours after starting an ACE inhibitor.
If the dry cough occurs, the doctor will need to change to another drug, ie, an angiotensin 2 inhibitor. The cough will subside once the ACE inhibitor is stopped.
Coughs in children
Coughs are more common during school term and are caused by common viruses which are commonly passed from child-to-child in school. While rarely serious, coughs and colds are an inconvenience and lead to many missed school days. Some tips to help prevent coughs and colds: Examples, which have become more common due to Covid-19, include ensuring your child wash their hands regularly and properly, especially after touching their nose or mouth and before handling food.
Teach them to always sneeze and cough into tissues to prevent spreading infection. Sharing unwashed cups and utensils is another common way to pick up colds and flu. Chesty coughs are especially common as kids return to school, but an antibiotic is rarely needed. Only 20 per cent of chest infections are bacterial, so antibiotics are ineffective in most cases.
Guidelines for cough and cold remedies for children
Guidelines came out in 2011 restricting the sale of cough and cold remedies to children aged under six years. The Health Products Regulatory Authority, or HPRA (known previously as the Irish Medical Board, or IMB) brought these guidelines out not because of any safety concern in children under six, but because they recognised that coughs and colds in children are frequent and normally self-limiting, and there is no real evidence to support the use of these products in children under six.
So, due to these guidelines, pharmacies can no longer sell products containing cough suppressants, decongestants or antihistamines for under-sixes. Common OTC remedies can no longer be given to children under six. For a child under six, the best advice is rest and plenty of fluids. Most coughs and colds in children under six will pass quickly but if it is not improving or there is signs of a bacterial chest/nasal infection (green mucus is a sign), an antibiotic may be needed, however over 80 per cent of coughs and colds are viral, so no antibiotic is needed.
Saline drops or spray are a good and safe option to clear sinuses in children over six. Decongestant rubs or drops that can be put on the child’s chest or hankie beside the bed can be comforting for the child. Paracetamol liquid is still recommended for high temperature in under-sixes. For children over six, there are many OTC products and there is no one that stands out as best. Always double-check the dose before giving, as there are different doses for different ages.
Prevention
As so many different viruses can cause the common cold, no vaccination against it has yet been developed. Some prevention tips are:
- Wash your hands regularly and properly, especially after touching your nose or mouth and before handling food.
- Always sneeze and cough into tissues to prevent spreading infection.
- Do not share cups or kitchen utensils with others. Use your own cup, plates, and cutlery.
Influenza
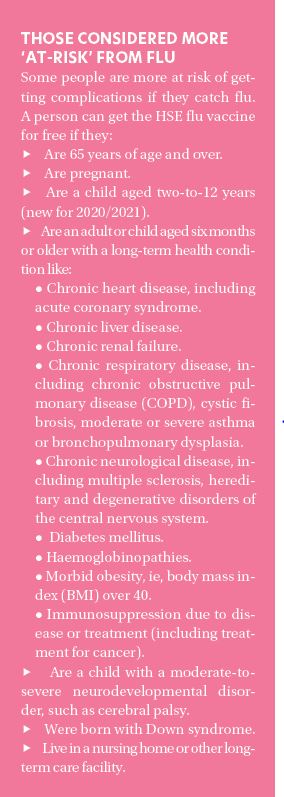
Influenza (flu) is a highly infectious acute respiratory illness caused by the influenza virus. It can affect people of any age. The seasonal flu vaccine (flu jab) protects against four strains of flu virus. These are the strains most likely to be circulating this flu season based on WHO evidence and based on virus circulation in the Southern Hemisphere.
Symptoms of flu include sudden fever, chills, headache, muscle pain, sore throat, non-productive dry cough, exhaustion, and weakness
You can get the flu vaccination at your GP surgery or local pharmacy. The flu vaccine is free if you have medical card or doctor visit card. It is also free this year to over-65s, for children aged under 12 years, people with any long-term illness, and healthcare workers. There have been well-documented shortages of the flu vaccines this year but despite this, the HSE is confident that most people in vulnerable categories got vaccinated through their GP or pharmacy.
Symptoms of flu
Symptoms of flu include sudden fever, chills, headache, muscle pain, sore throat, non-productive dry cough, exhaustion, and weakness. Flu characteristically causes a temperature of 38-to-40°C that lasts for three-to-four days.
Difference between cold and flu
A cold will develop slowly over a few days, with symptoms like a sore throat and a blocked or runny nose. The symptom of flu hits suddenly and severely, with symptoms like fever and muscle aches. Often, people suffering from a bad cold wrongly believe they have flu. Flu causes extreme exhaustion, muscle aches, severe sweats and leaves a person so weak, they will not be able to get out of bed. Work and other normal routines are not possible with flu.
Complications of flu
Most people recover from flu in two-to-seven days, but in some, it can last for up to two or three weeks. Flu can be severe and can cause serious illness and death, especially in the very young and in the elderly. Serious respiratory complications can develop, including pneumonia and bronchitis. Older people and those with certain chronic medical conditions are at particular risk of these complications. Pregnant women and women up to six weeks after giving birth have also been found to be at increased risk of the complications of flu. Eighty-to-90 per cent of reported deaths from influenza occur in the elderly, mainly from bacterial pneumonia (200 deaths per year in Ireland), but also from the underlying disease. The good news is that with social distancing, mask-wearing and increased uptake in flu vaccines, incidence of influenza is likely to be a lot lower this flu season, as the flu virus has had less chance to spread. The incidence of flu in Australia was a lot lower in 2020 due to the measures brought in to combat Covid-19.
Some people should get the vaccine to protect themselves, their families and those they care for. These include those who:
- Work in healthcare.
- Are a carer or live with someone who is at risk of flu because of a long-term health condition.
- Are a carer or live with someone who has Down syndrome.
The flu vaccine is free for healthcare workers.
Flu vaccine side-effects
There may be a mild fever and aching muscles for a couple of days after having the vaccine. The arm where the vaccine was given may also be a bit sore. Serious side-effects from the flu vaccine are very rare. There is no aluminium, thiomersal, mercury, gelatin or porcine gelatin in the quadrivalent inactivated influenza vaccine used in the 2020/2021 campaign.
Flu vaccine for children
Children are more likely than adults to get severe complications of flu. Children who are sick with flu miss days in crèche, childcare and school. They also miss out on their usual activities, such as hobbies and sports. Children aged two-to-12 can now get the nasal flu vaccine for free. The flu vaccine will help protect a child against flu and reduce the spread of flu to others, for example, their brothers and sisters, parents, and grandparents.
The vaccine is given as a single spray in each nostril of the child’s nose. The child can breathe normally while getting the vaccine. There is no need to take a deep breath or sniff. The vaccine is not painful and is absorbed quickly. It will work even if the child has a runny nose, sneezes, or blows their nose after the vaccination. Most children need only one dose of the vaccine each year. Some children with chronic health conditions, like chronic heart or lung conditions, may need two doses. The doses are given four weeks apart for these high-risk children if they have never had a flu vaccine.
Side-effects of the nasal flu vaccine
The most common side-effects are mild and include:
- A runny or blocked nose.
- Headache.
- Muscle aches.
Some children get a fever after the vaccine. It is usually mild and goes away on its own. If the child has a fever or a headache, paracetamol or ibuprofen can help. Aspirin, or any medicines that contain aspirin, should never be given to children unless prescribed by a doctor (due to risk of Reye syndrome). This is especially important in the four weeks after getting the flu vaccine. Serious side-effects such as a severe allergic reaction are rare. There is no evidence that you can catch flu from the nasal flu spray.







