The management of wounds is best carried out by an organised multidisciplinary team that can offer support to the individual — and the pharmacist is one of the significant players in the process
In Ireland, estimates indicate that up to 50% of acute hospital beds are occupied by patients with a wound. Furthermore, it is estimated that more than 23% of all hospital inpatients have a pressure ulcer, many of which develop during their hospital stay, and are avoidable.(1) Due to population and demographic factors such as rise in population growth in Ireland (16% in the last 10 years), and the increase in the number of people over 65 (which will triple in the next 30 years), prevalence and incidence of wounds is predicted to increase here also. The climbing rates of illnesses like obesity, diabetes, and lower extremity arterial disease will also add to this burden. Even now, about 68% of community nurses’ time is spent treating wounds. The estimated annual cost of wound care to the HSE is €788.5m.(1)
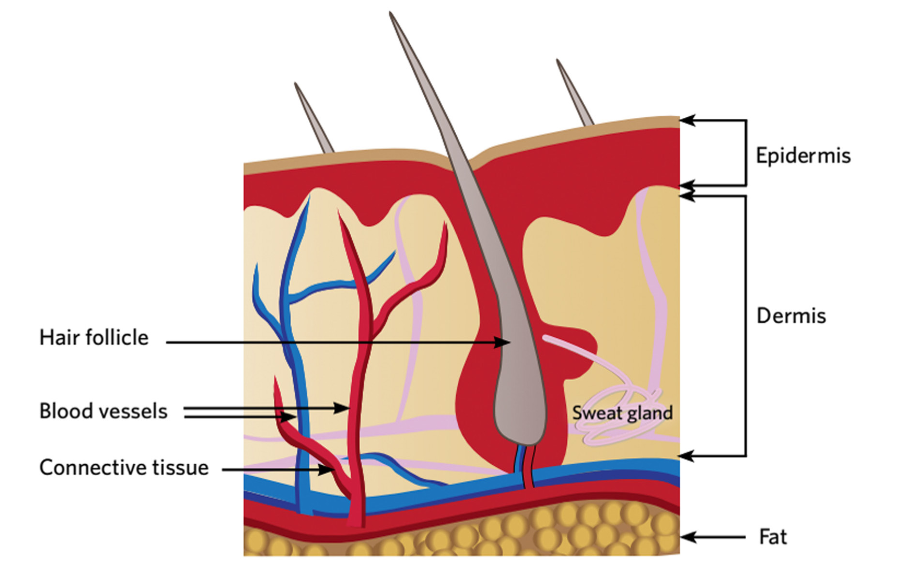
FIGURE 1: The layers of the skin
Pharmacists are often the first point of contact for people with wounds. The pharmacist’s role in wound care includes providing first aid, identifying and advising on the treatment of different wound types, dispensing prescribed medicines to treat infected wounds, providing education and support to those living with chronic wounds, and referral to other healthcare colleagues where appropriate. It is well established that the management of wounds is best carried out by an organised multidisciplinary team that can offer support to the individual, although often there is little information about the role, responsibilities and skills of pharmacists in wound management. Resources to help are available however:
in 2020, a multidisciplinary team from pharmacy and nursing backgrounds in the UK created a document(2) to help inform pharmacy colleagues about the principles of best practice and evidence in wound care and dressing selection to assist pharmacy teams to manage wounds in the community. The HSE and Office of the Nursing and Midwifery Services Director have also published national wound care guidelines.(1)
Skin Health
The skin contributes about 15% of body weight, and is responsible for acting as a barrier to chemical, physical
and mechanical barriers, as well as microorganisms and allergens. As well as its protective function, it has roles in thermoregulation, metabolism, sensation, synthesis and communication. In healthy people, the skin is strong and resilient. Skin integrity has been recognised as an important concept, and preventive measures can be taken in people with frail skin (e.g. older people, those with comorbidities, incontinence, or taking medications that affect the skin). Moisturising regularly, which promotes general skin health and reduces the risk of damage (e.g. skin tears, superficial pressure ulcers) should be a vital part of skincare in people with frail skin. Nutrition and hydration are also important contributing factors to skin health. Potential polypharmacy issues may need consideration due to some medications possibly causing changes to skin.(3) Medications most likely to impair wound healing and damage skin integrity include(4)
- Antibiotics;
- Anticonvulsants;
- Angiogenesis inhibitors;
- Steroids;
- NSAIDs (given long term, and especially in higher doses)
Conversely, drugs such as ferrous sulphate, insulin, thyroid hormones, and vitamins may facilitate wound healing.
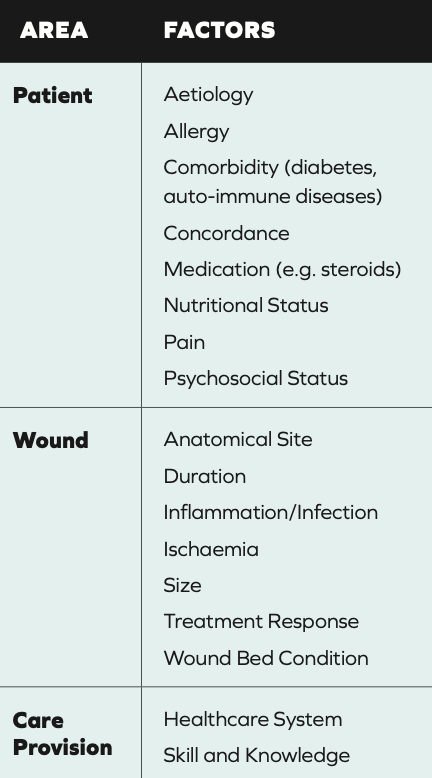
TABLE 1: Factors affecting Wound Healing Ability(1)
Wound Healing
A wound is defined as a breach in the skin.(1) Acute wounds generally heal in a timely manner and precise process, producing a healed wound with anatomic and functional integrity, e.g. abrasions, lacerations, burns, skin tears, bites, surgical wounds.(2)
Chronic wounds are those for which healing is impaired, e.g. venous leg ulcers, diabetic foot ulcers, pressure ulcers.(1,2) Often in chronic wounds, the inflammatory process is dysfunctional because of factors that impact the person, wound or healing environment.
Healthy wound healing has four processes: haemostasis, inflammation, proliferation and maturation. Local and systemic factors (Table 1), and certain diseases (diabetes, Raynaud’s, heart disease and rheumatoid arthritis) can impact this. Ageing makes the skin more vulnerable and slower to repair.
(2) In children, wounds heal faster as a result of more rapid creation of granulation tissue. There is a higher level of collagen and elastic produced, but the overall healing process is the same as in adults.(1)
Certain life stages are associated with a more frequent development of skin problems or issues around healing:
- Early in life (when the skin is not fully mature);
- When individuals are suffering from dermatological or other systemic and chronic diseases;
- At advanced age;
- During severe illness or at the end of life (2)
Minor wounds are usually healed within weeks, but more complicated wounds heal much more slowly. A chronic or hard to heal wound can be defined as one that has not healed in 12 weeks, or one that has not reduced in area by 40% in four weeks with appropriate treatment. Depending on the wound type and complexity, specialist treatment may be required.(2)
Macro and micronutrients and adequate hydration are very important for the wound healing process as well as general skin health. Deficiencies in these can prolong inflammation, leading to the reduced production of collagen and other cells needed for healing. Protein is required for collagen synthesis, angiogenesis, fibroblast proliferation, immune function, tissue remodelling, wound contraction and skin structural proteins. The recommended adult protein intake for this is between 1.25 and 1.5g/kg/day.
Exudate is a very important component of the healing process in a healthy wound. Volume, viscosity and colour should all be considered to determine wound health. Unhealthy tissue around the wound can be classified as dry, macerated, excoriated or inflamed. Early identification of loss of integrity in this tissue is very important to stop any increase in wound size and healing delays. The appearance of the wound bed itself differs depending on the healing stage:(1)
- Epithelialisation occurs when epithelial tissue (usually pink, sometimes translucent) migrates across the wound surface;
- Granulation tissue is rich in macrophages and fibroblasts. Its extracellular matrix includes collagen, hyaluronic acid and fibronectin. It is often uneven and granular in appearance, and is bright red;
- Over-granulation is overgrowth of granulation tissue raised above the wound surface. This can slow epithelialisation if not addressed;
- Infection can be difficult to identify as signs vary between different wounds. Tissue may be friable, dull or beefy red in colour;
- Fungating refers to a malignant process where there is ulcerating (crater) and proliferative growth. Some wounds are a mixture of both;
- Slough is composed of dead cellular debris and usually yellow/white. Fibrin deposits are often present and make the removal of slough difficult;
- Necrosis is the result of tissue death secondary to ischaemia. This is black or brown in appearance and may be dry and leathery in texture. It will delay healing.
Wound Assessment
There are three main objectives of wound care:(1)
1. The wound should be allowed to heal in a moist wound environment, unless the clinical goal is to maintain a dry wound bed, e.g. ischaemic foot.
2. Address the issues observed in the assessment process.
3. Promote wound healing.
When a patient presents with a wound, correct wound assessment is important
in order to guide appropriate treatment. Effective assessment also helps reduce variation in practice, so ideally a structured assessment tool should be used. The TIME principle is a well-established concept
in wound care that provides a structural framework for assessment. It is based on identifying the barriers to healing and implementing a plan of care to remove these
barriers and promote healing. Although there are variations, the four key principles are:(2)
T – Tissue within the wound
I – Infection and/or Inflammation M – Moisture balance
E – Edge of the wound.
Wound size is also a useful baseline indicator. Wound Assessment Tool examples are provided in the Appendices to the HSE Wound Management Guidelines (1).
The wound assessment should include: ?Type of wound and aetiology; ?Location;
- Duration;
- Exudate description;
- Condition of the wound bed;
- Size of wound (measurement); ?Condition and sensation of peri-
wound skin; - Presence of Infection;
- Presence and nature of pain;
- Objectives of wound healing.
The outcome of this should support management choices.(1)
Where assessment is not possible in the pharmacy setting, the goal may be to provide ‘stop gap’ assistance or first aid, while referring the patient to the appropriate services. It is important to be realistic about what is possible, and it may be the case that ‘something’ is better than nothing, depending on the patient’s needs and availability of products, information and support. Resources and facilities vary significantly, meaning that differing levels of service provision are available. We must work with whatever is available, while always aiming for best practice and patient-focused care.
Individual patient concerns should be addressed, as well as their capacity, environment, support, psychosocial factors and quality of life issues. The individual needs to understand the underlying cause of the wound and treatment rationale. Involving the patient and family must be done as much as possible to improve concordance with treatment. Wound and patient assessment should be done with the aim to take action, and to set treatment goals, e.g. through dressing selection and other wound care products, providing information and support, or directing to further information or services.(2)

TABLE 2: Principles of TIME, possible associated issues, and actions for improving wound healing(2)
WOUND BIOBURDEN AND BIOFILM
The internal component of the wound microenvironment includes cells that play a role in healing and regulation of healing. The external component involves microbes that normally live on the skin, and the environmental factors that impact this colonisation. This microenvironment plays a key role in the wound healing process.(1) Many wounds containing microorganisms heal successfully, however, sometimes there is a disruption to the interplay between the internal and external microenvironments and bacteria may invade, multiply, and cause tissue damage.
Biofilms are created when communities of bacteria adhere to a wound surface. These shed bacteria and fragments of biofilm which can disperse and attach to other parts of the wound bed, or other wounds. Wounds that have a biofilm are up to 500- 50,000 times more tolerant to antibiotic treatment. In contrast to resistance, which reduces the effectiveness of the drug concentration, tolerance increases resilience to antibiotic treatment duration, e.g. when bacteria transiently arrest their growth. It can be difficult to clinically recognise the presence of a biofilm.
WOUND INFECTION
In acute wounds, potential infection may be indicated by(1)
- Inflammation;
- New/increasing pain;
- Local heat;
- Swelling;
- Advancing redness;
- Increase in serous or purulent discharge;
- Abscess or malodour.
- Development of new pain or change in existing pain is one of the strongest indicators of infection. In immunocompromised, older patients or those taking anti-inflammatories, these classical signs may not be present. Early diagnosis of wound infection and treatment is critical to minimise the risk that this develops into systemic infection. The World Union of Wound Healing Societies has defined additional signs of wound infection:(5)
- Loss of appetite;
- General lethargy, malaise;
- Inability to undertake normal activities;
- Deterioration in glycaemic control in patients with diabetes;
- There may be other subtle changes in the wound bed, e.g., wound bed colour may appear darker, less vascular and there may be an increase in slough.
Management of wound infection involves maximising the host response, treating the wound bed, and treating
the general wellbeing of the patient.(1) A multidisciplinary response is advised. Appropriate use of systemic antibiotics is very important. The national guidelines should be followed for information relating to the prescribing of antibiotics and antibiotic stewardship, found at www. antibioticprescribing.ie, http://www.hpsc.ie/ and https://www.hiqa.ie.
WOUND PAIN
Pain from chronic wounds can have both nociceptive and neuropathic elements. (1) Nociceptive pain is directly from the damaged tissue (‘sharp’, ‘stabbing’) whereas neuropathic pain is due to damage or dysfunction to the nervous system (‘burning’, ‘tingling’). The body recognises pain as a stressor, triggering a stress response with an increase in adrenal release of cortisol.. This further delays the inflammatory response and healing. Pain impacts on quality of life, leading to reduced appetite and sleep, and potentiating the stress response further. Often, despite best efforts, the dressing change procedure is a major contributor to wound pain due to the tissue damage that can often happen. Analgesia, e.g. NSAIDs, if necessary should be given at a time for maximum effect. Distraction can be useful. Best practice in dressing removal is very important to avoid more damage to the skin or medical adhesive related skin injury (2).
- In wounds such as skin tears, mark the dressing with an arrow to indicate the correct direction of removal;
- Adhesive removers can be used when removing the dressing to minimise trauma;
- Take time to remove dressings slowly;
- Consider using a skin barrier product to protect the surrounding skin (e.g. to prevent maceration if the wound has high exudate levels);
- Use an emollient to soften and smooth wider skin area and prevent further damage;
- Continue to monitor the wound for changes or signs of infection.
The aseptic non-touch technique should be used.(1) Susceptible body sites must not come into contact with non-sterile items.
WOUND DRESSING
The enormous range of dressing types means that even dressing selection can be an advanced skill. Many healthcare professionals lack confidence in selecting the best dressing in practice. Importantly, the Wound UK document(2) notes that – particularly when combined with appropriate assessment – the risk of causing harm through ‘getting it wrong’ is very low. Pharmacists in the community should know the principles of assessment-based dressing selection to treat common wound types, and how to access more information and resources, but do not need knowledge of every single dressing available. Table 3 describes some common dressings.
A dressing does not heal the wound but rather provides the optimal environment for healing to take place. Dressings are applied to:(2)
- Provide rapid and cosmetically acceptable healing;
- Remove or contain odour;
- Reduce pain;
- Prevent or combat infection;
- Modify or inhibit matrix metalloproteinase activity within the wound;
- Contain exudate;
- Cause minimum distress or disturbance to the patient;
- Hide or cover a wound for cosmetic reasons.
- Factors influencing the dressing selection include:
- Type of wound/cause;
- Wound characteristics (e.g. granulating, epithelialising, sloughy, necrotic); ?Treatment goals (e.g. to manage exudate, manage infection risk); ?Anatomical location;
- Patient-related factors (e.g. pain levels, fragile skin, capacity to self-care); ?Cost.
- Patients should be informed to change dressings according to the manufacturers’ instructions and in line with treatment goals.
- Dressings impregnated with topical antimicrobials such as silver, iodine, PHMB, or honey are useful for infected wounds. Alternatively, some non- medicated wound dressings are also designed to sequester bacteria without the need for an antimicrobial agent. Charcoal dressings are useful for wounds with odour issues (as secondary dressings).
- A Cochrane review(6) found that the effects of cleansing with tap water, cooled boiled water or distilled water compared with cleansing with saline are uncertain, as is the effect of distilled water compared with cooled boiled water. Wound irrigation should be done if needed in order to remove debris.(1)
- There is evidence that modern or advanced dressings like hydrocolloids, alginates and hydrofibre dressings are more effective than conventional dressings (e.g. paraffin gauze), there is not conclusive evidence at this stage to promote one above the other. The wound should be reassessed at each change to determine if the current product and wear time is appropriate.
USE OF COMPRESSION
Lower limb ulcers are wounds on the lower leg and foot that are slow to heal. Venous insufficiency is the largest cause of leg ulceration, and there is strong evidence to show that the use of compression therapy helps healing of venous leg ulceration. People with diabetes are 23 more times likely to have a leg, foot or toe amputation than people without diabetes.(2)
There are some ‘red flags’ that contraindicate compression:
- Acute infection of the leg or foot (e.g. increasing unilateral redness, swelling, pain, pus, heat);
- Symptoms of sepsis;
- Acute or chronic limb- threatening ischaemia; ?Suspected acute deep vein thrombosis (DVT);
- Suspected skin cancer.
If the above red flags are not present, all patients with a lower limb wound should be given mild compression as soon as possible.
Compression applies graduated pressure to the leg. The highest pressure is at the ankle, and it gradually reduces towards the knee.
Compression increases venous blood flow up the leg, reducing oedema and underlying tissue inflammation. However, it is only effective if it is worn consistently. To help this, patients need product choice and to know that if they cannot tolerate one type of bandage/wrap/hosiery, there are alternatives to try. The key function of hosiery is preventing recurrence, so this means that compression therapy is a long- term treatment.

TABLE 3: Common Dressing types, suitable wounds and notes for use(2)
CONCLUSION
Although it should be noted that pharmacy teams are not always the most appropriate personnel to fulfil every role, they are often the only trained healthcare professional that the patient sees, providing the entry point through which the patient receives care.(2)
When considering the role of the pharmacist and pharmacy teams, this should always be viewed in the context of the patient journey and the patient outcome. The more patient-focused care is, then the more the outcome can be improved.
REFERENCES
1. Health Service Executive and Office of the Nursing and Midwifery Services Director. (2018). HSE National Wound Management Guidelines 2018. Available https://healthservice.hse.ie/ filelibrary/onmsd/hse-national-wound- management-guidelines-2018.pdf
2. Ousey, K., Atkin, L., Conway, B., et al. (2021). Wound care and dressing selection for pharmacy teams. London: Wounds UK. Available https://wounds-uk.com/.
3. LeBlanc, K., Campbell, K. E., Wood, E., & Beeckman, D. (2018). Best practice recommendations for prevention and management of skin tears in aged skin: an overview. Journal of Wound Ostomy & Continence Nursing, 45(6), 540-542.
4. Beitz, J. M. (2017). Pharmacologic Impact (aka” Breaking Bad”) of Medications on Wound Healing and Wound Development: A Literature- based Overview. Ostomy/wound management, 63(3), 18-35.
5. World Union of Wound Healing Societies. (2008). Wound infection in clinical practice. An international consensus. Int Wound J, 5 Suppl 3, iii-11.
6. Fernandez, R., Green, H. L., Griffiths, R., Atkinson, R. A., & Ellwood, L. J. (2022). Water for wound cleansing. Cochrane database of systematic reviews, (9).
TRUE/FALSE QUESTIONS
Q1: The skin contributes about 15% of body weight. True or false?
Q2: The recommended adult protein intake for this is between 3.5 and 4.5g/kg/day. True or false?
Q3: A chronic or hard to heal wound can be defined as one that has not healed in 12 weeks, or one that has not reduced in area by 40% in four weeks with appropriate treatment. True or false?
Q4: A hydrocolloid dressing is suitable for wounds with mild/moderate levels of exudate.
True or false?
Q5: Slough is the result of tissue death secondary to ischaemia. True or false?
Q6: A hydrogel dressing is suitable for wounds with moderate/ high exudate levels, sloughy wounds. True or false?
Q7: Wound size is a useful baseline indicator for wound assessment. True or false?
Q8: Dressings impregnated with topical antimicrobials such as silver, iodine, PHMB, or honey
are useful for infected wounds. True or false?
Q9: Analgesia, e.g. NSAIDs, should be given just after the dressing change procedure for maximum effect for pain due to dressing change. True or false?
Q10: Compression increases venous blood flow up the leg, reducing oedema and underlying tissue inflammation. It is effective if it is worn for 48 hours. True or false?
MCQs
Q1: Medications that can impair wound healing and damage skin integrity include:
I. Anticonvulsants
II. Insulin
III. Steroids
IV. NSAIDs (given long- term, and especially in higher doses)
All of the above None of the above
Q2: In acute wounds, potential infection may be indicated by:
I. Inflammation
II. New/increasing pain III. Local heat
IV. Swelling
All of the above
None of the above
Q3: Factors influencing the dressing selection include:
I. Type of wound/cause II. Wound characteristics III. Anatomical location IV. Cost
All of the above
None of the above
Q4: Which of these are red flags’ that contraindicate compression:
I. Lower limb ulcers
II. Acute or chronic limb- threatening ischaemia III. Suspected acute deep vein thrombosis
IV. Suspected skin cancer
All of the above None of the above
Q5: Which of the following is true when a patient presents with a wound:
I. Correct wound assessment is important in order to guide appropriate treatment. II. Effective assessment helps reduce variation in practice, so ideally a structured assessment tool should be used.
III. Patients should be informed to change dressings according
to the manufacturers’ instructions and in line with treatment goals. IV. There is no evidence that modern or advanced dressings like hydrocolloids, alginates and hydrofibre dressings are more effective than conventional dressings (e.g. paraffin gauze).
All of the above None of the above