Dr Donna Cosgrove PhD MPSI provides a clinical overview of the complexities of cardiovascular disease
Introduction
Cardiovascular disease (CVD) describes disease of the heart and blood vessels caused by the process of atherosclerosis, and includes coronary heart disease (CHD), stroke, and other circulatory diseases.1 CVD is the most common cause of death in Ireland, accounting for 36 per cent of all deaths.2 According to the WHO, more than 17 million people worldwide died from CVD in 2008. The largest number of deaths relate to CHD and are mainly due to myocardial infarction (7.3 million).2 Strokes were responsible for 6.2 million.3 Of these deaths, more than three million occurred before the age of 60 and could have largely been prevented. CVD also has significant cost implications: The cost to the NHS in England was estimated at £7,880 million in 2010.1
Atherosclerosis and Coronary Heart Disease
Atherosclerosis is an inflammatory process that affects the cardiovascular system.3 CHD occurs when the coronary blood vessels are blocked by a build-up of cholesterol: This causes narrowing of the lumen and makes the inner surfaces of the blood vessels irregular and less pliable, which is detrimental to regular blood flow.2,3
When the blood vessel endothelium is exposed to raised levels of low-density lipoprotein (LDL), cholesterol and additional substances like free radicals, the endothelium becomes permeable to lymphocytes and monocytes. These cells migrate into the wall of the blood vessel, resulting in a series of reactions and attracting LDL cholesterol to the site. This cholesterol is engulfed by monocytes, which are then transformed into macrophages. Smooth muscle cells migrate to the site from deeper layers of the vessel wall (the media). Then, a fibrous cap, consisting of smooth muscle and collagen, is formed.3 At the same time, the macrophages involved in the original reaction begin to die, forming a necrotic core. These lesions (atheromatous plaques) grow bigger as cells and lipids accumulate in them and begin to bulge into the vessel lumen. As the process continues, thinning of the fibrous cap and a fissuring of the endothelial surface of the plaque occur, which may cause rupture. With rupture, lipid fragments and cellular debris are released into the vessel lumen and exposed to thrombogenic agents on the endothelial surface, resulting in the formation of a thrombus.
If the thrombus is big enough, and a coronary blood vessel or a cerebral blood vessel is blocked, the blood flow to the heart is cut off. The decrease in the supply of oxygen and nutrients causes chest pain (angina) due to ischaemia3 and can damage the heart muscle, resulting in a heart attack (MI). Symptoms of MI include sweating; light-headedness; nausea; and breathlessness, like angina, although not relieved by a nitrate spray.
Although LDL cholesterol tends to build up on the walls of the coronary arteries, increasing risk of heart disease, HDL cholesterol carries cholesterol away from the cells and back to the liver, where it is broken down or excreted. The current recommendation for healthy cholesterol levels is a total blood cholesterol level of less than 5mmol/litre, a HDL level of >1mmol/litre, and an LDL level of under 3mmol/litre.2
Risk Factors
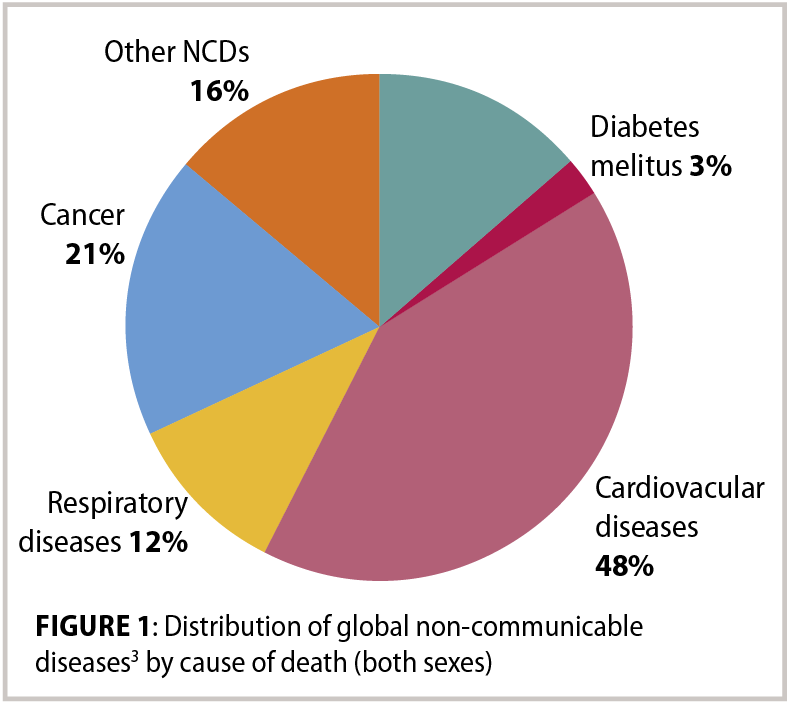
The atherosclerotic process can start to develop before adulthood. There is strong evidence that tobacco use, physical inactivity, unhealthy diet, excessive alcohol intake, hypertension, diabetes, raised blood lipids, obesity, poverty, low educational status, advancing age, male gender, genetic disposition and psychological factors all contribute to this process.1,3 Behavioural risk factors for atherosclerosis such as tobacco use, physical inactivity, an unhealthy diet, and harmful use of alcohol are risk factors for many non-communicable diseases (NCDs), not just atherosclerosis, thus a large percentage of NCDs are preventable through the reduction of these risk factors.
Hypertension
Hypertension affects more than one billion individuals worldwide. It puts a strain on the heart, contributing to CHD and causing an estimated 9.4 million deaths every year.2,5 The benefits of decreasing blood pressure are long established based on observational studies and trials of hyper- and normotensive patients. A review of studies concluded that a 10mmHg reduction in systolic blood pressure has been shown to reduce the risk of major CVD events by 20 per cent, CHD by 17 per cent, stroke by 27 per cent, heart failure by 28 per cent, and all-cause mortality by 13 per cent.5 This was evident across multiple groups of patients, which suggests that blood pressure-lowering provides benefits that are somewhat generalisable. Even patients with lower blood pressure at baseline benefitted from these notable effects. The authors of this review5 suggest a case-by-case assessment by clinicians of each patient’s risk factors to decide on the blood pressure level at which to start antihypertensive medication, rather than a decision based on an arguably arbitrary fixed threshold for blood pressure, which is just a single risk factor for CVD.

The best approach to reduce blood pressure, however, is still unclear: Generally, the commonly-prescribed antihypertensives are effective overall in contributing to preventing cardiovascular disease, but there are some modest but significant differences between treatments in terms of specific clinical outcomes: Calcium channel blockers appear to be more effective than other classes of drugs for stroke prevention, whereas diuretics work better for prevention of heart failure. Beta blockers appeared to be inferior to other classes of antihypertensives for the prevention of major cardiovascular disease events, stroke, renal failure, and all-cause mortality.
Smoking
Tobacco use is a huge contributor to the development of health problems, including heart attacks, strokes, sudden death, heart failure, aortic aneurysm and peripheral vascular disease.3 Smoking increases the risk of heart disease by 24 per cent. Carbon monoxide and nicotine present in cigarette smoke place a strain on the heart by increasing heart rate and risk of blood clots, and additional chemicals also damage the lumen of the coronary arteries.2
Physical activity
Regular physical activity can prevent obesity. Insufficient physical activity not only contributes to heart disease, but is the fourth-leading risk factor for mortality. According to the WHO Global Atlas on cardiovascular disease prevention and control, 31.3 per cent of adults aged 15 or older are not sufficiently active, a figure that may have increased since its publication in 2011. People who do not engage in enough physical activity have a 20-to-30 per cent increased risk of all-cause mortality compared to those who engage in at least 30 minutes of moderate-intensity physical activity most days of the week.3 Participating in 150 minutes of moderate physical activity each week (or 75 minutes of vigorous intensity aerobic activity, or a mix of both) can reduce the risk of ischaemic heart disease by approximately 30 per cent and the risk of diabetes by 27 per cent.3
Alcohol
There is a complex relationship between alcohol consumption and CHD/cerebrovascular disease. There is a direct relationship between higher levels of alcohol consumption and binge-drinking (60 or more grams alcohol per day) with risk of CVD. Low levels of drinking alcohol, conversely, may be associated with a reduced risk of negative cardiovascular outcomes. Various mechanisms have been suggested for the protective effect, ie, beneficial effects of alcohol on the HDL cholesterol level, thrombolytic profile and platelet aggregation.3 If alcohol is consumed, the recommended weekly limit of 14 standard drinks should be adhered to, with these units spread out over at least three days. Binge drinking should always be avoided.2

Diet
People at high risk of or with CVD should be advised to reduce their saturated fat intake and increase their mono-unsaturated fat intake. Unsaturated fat will help reduce cholesterol levels.
Foods high in unsaturated fat include oily fish, avocados, nuts and seeds, sunflower, rapeseed, olive and vegetable oils.2 Wholegrain varieties of starchy food are preferred, and daily intake of sugar and food products containing refined sugars should be reduced. At least five portions of fruit and vegetables should be consumed per day, and two portions of fish per week, including a portion of oily fish, and at least four-to-five portions of unsalted nuts, seeds and legumes.1 Dietary salt consumption is an important contributor to hypertension and cardiovascular risk, and daily intake should not exceed 6g.3
Maintaining Cardiac Health
Several prospective human studies have demonstrated the cardioprotective effect of fish, ie, the Physicians’ Health Study, which followed 20,551 male physicians for up to 11 years.6 A 52 per cent reduction of sudden cardiac death in males who consumed fish once a week was reported compared to those who ate fish less than once a month. This cardioprotective effect has been attributed to its content of the omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA).
One meta-analysis of clinical trials investigating the cardioprotective effect of omega-3 supplements showed significant effects on triglycerides, blood pressure, heart rate and CRP, with small, significant increases in both LDL-C and HDLC, although the authors say that the quantity of EPA and DHA required for these effects is still unknown.6
Conversely, a Cochrane review7 of the use of long-chain omega-3 fats (79 trials involving over 112,000 people) found no evidence to suggest that they have any important positive or negative effects on mortality, CVD events or other measures of cardiovascular health. There was evidence that increasing ALA (in, ie, walnuts or enriched margarine) probably slightly reduces CVD risk, but effects were very small.
The review concludes that supplemental long?chain omega?3 fats are probably not useful for preventing or treating cardiovascular disease, although long?chain omega?3 fats can help to reduce serum triglycerides and raise HDL a little.
Regardless of the reported lack of association of omega-3 with heart health, fish and seafood are nutrient?dense and rich in a variety of other nutrients (such as vitamin D, calcium, iodine, selenium), so are useful foods, even without the potential cardiovascular benefits. NICE guidelines advise against recommending omega 3 oils for CVD prevention, and likewise for plant stanols or sterols.1
Treatment of Cardiac Disease
In severe cases of CHD, surgical procedures to treat blocked arteries are sometimes required, such as coronary angioplasty or a coronary artery bypass. In a small number of people, a heart transplant may be performed. However, in most cases, patients can successfully manage CHD with medicines, ie, ACE inhibitors, channel blockers, beta blockers, low-dose aspirin, nitrates and statins.2 The NICE guideline groups statins into three different intensity categories according to the percentage reduction in LDL cholesterol they produce: Low intensity if the reduction is 20-to-30 per cent; medium intensity is 31-to-40 per cent; and high intensity is above 40 per cent.
In addition to adherence to prescribed regimens, it is important for individuals being treated for, or at risk of, CVD to keep the behavioural risk factors in mind and reconsider their lifestyle in light of these.
Self-care is an integral part of daily life and is all about the individual taking responsibility for their own health and wellbeing with support from the people involved in their care.
Self-care includes the daily actions undertaken in order to stay fit and maintain good physical and mental health, prevent illness or accidents, and care more effectively for minor ailments and long-term conditions.2