Eamonn Brady MPSI looks at treatment and advice options for some of the more common eye infections
Section 1: Causes and types
Eye infections are among the most frequent ocular complaints encountered in Irish community pharmacy. While most are self-limiting, recognising the likely cause and understanding clinical features allows pharmacists to triage and refer appropriately.
The eye’s natural defense mechanisms, tear film, corneal epithelium, and blinking help prevent microbial invasion. Disruption through trauma, foreign bodies, systemic illness, or daily contact lens use increases infection risk.
Contaminated cosmetics or lens solutions are also frequent causes.
Causative organisms and distribution
European data indicate:
- Bacterial: Approximately 65-to-70 per cent of cases.
- Viral: Approximately 20-to-25 per cent of cases.
- Fungal: Approximately 2-to-5 per cent of cases.
- Parasitic: <1 per cent of cases.
Most bacterial eye infections involve:
- Staphylococcus aureus or S.epidermidis: Cause blepharitis (inflammation of the eyelid margins) and styes.
- Streptococcus pneumoniae and Haemophilus influenzae: Cause purulent conjunctivitis.
- Pseudomonas aeruginosa: Causes contact lens-related keratitis (corneal inflammation), particularly among daily users.
Viral causes (approximately 25 per cent of cases)
- Adenoviruses: Cause epidemic keratoconjunctivitis (red, watery eyes).
- Herpes simplex virus (HSV): Causes recurrent herpetic keratitis (corneal ulceration).
- Varicella-zoster virus: Causes shingles-related eye disease (herpes zoster ophthalmicus).
Fungal causes (Approximately 2-to-5 per cent of cases)
Follow trauma involving organic material or occur in immunocompromised patients. Common organisms include Fusarium, Aspergillus, and Candida.
Parasitic causes (<1 per cent of cases) Acanthamoeba keratitis — rare but serious, mostly in daily contact lens users who clean or store lenses in tap water.
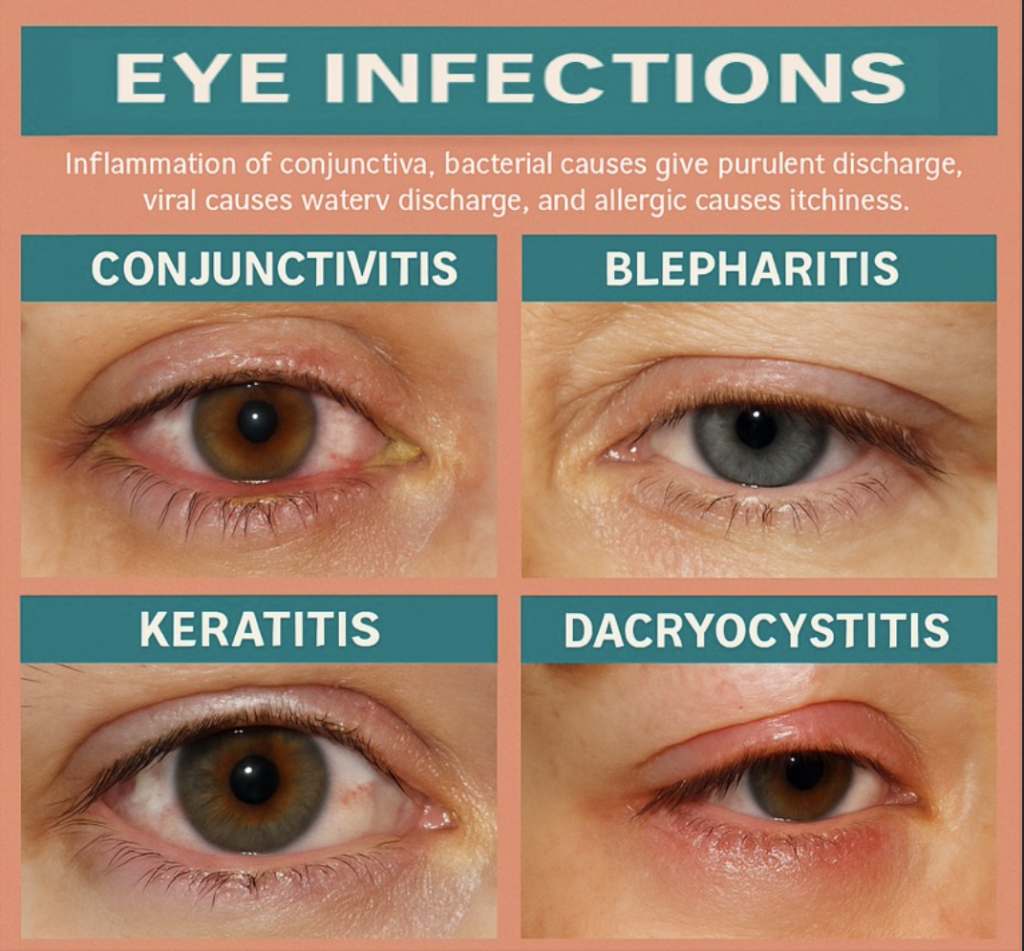
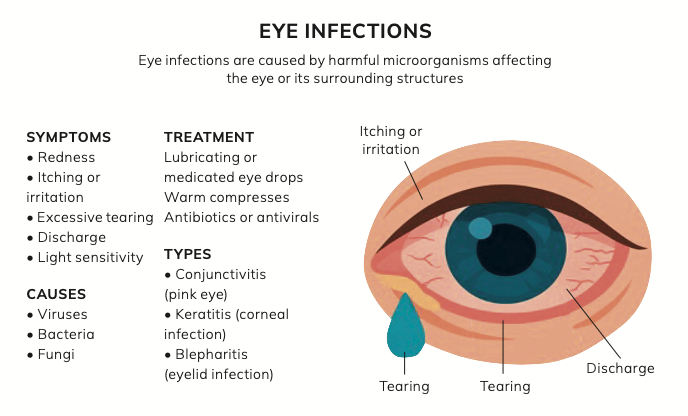
Main types of eye infection
- Conjunctivitis: Inflammation of the conjunctiva; bacterial causes give purulent discharge, viral causes watery discharge, and allergic causes itchiness.
- Blepharitis: Chronic lid margin inflammation causing crusting, redness, and irritation.
- Keratitis: Corneal inflammation (cornea = clear front of the eye) that can lead to ulceration (open sore on the cornea).
- Dacryocystitis: Infection of the lacrimal sac (tear drainage sac) due to blocked nasolacrimal duct.
- Endophthalmitis: Infection inside the eyeball — medical emergency with severe pain and reduced vision.
References
1. Health Service Executive (HSE). Community Eye Care Guidance. Dublin: HSE; 2023.
2. NationalInstituteforHealthandCare Excellence (NICE). Conjunctivitis – Infective: Antimicrobial Prescribing (NG234). London:
NICE; 2024.
3. Royal College of Ophthalmologists (RCOphth). Guidelines for the Management of Acute Red Eye. London: RCOphth; 2022.
4. CentersforDiseaseControlandPrevention (CDC). Contact Lens Health Week – Educational Materials. Atlanta, GA: CDC; 2023.
5. CollegeofOptometrists(UK).BacterialKeratitis Clinical Management Guidelines. London: College of Optometrists; 2023.
Section 2: Treatment and management
Pharmacists in Ireland are often first consulted for ‘eye infections’, but the priority is identifying those needing medical review. Unlike the UK, chloramphenicol remains prescription-only (POM). For mild bacterial infection, Brolene (propamidine isetionate) is the main OTC option.
Bacterial conjunctivitis
Self-limiting within five-to-seven days, but antibiotics shorten symptoms,
- Prescription-only: Chloramphenicol 0.5% drops or 1% ointment; fusidic acid 1% viscous drops.
- OTC: Brolene: One-to-two drops up to four times daily (limit to three-to-five days; refer if no improvement).
Advice
- Wash hands before and after touching eyes.
- Discard old cosmetics or contact lenses.
- Avoid sharing towels.
- Clean eyelids with cooled boiled water or sterile wipes.
Blepharitis and styes
Both cause sore, red, crusted lids.
- Warm compresses (five-to-10 min, twice daily) and lid scrubs improve drainage.
- Brolene ointment can assist mild bacterial blepharitis (at time of writing in October 2025, still long-term out of stock and due back 15/01/2026).
- Persistent or recurrent cases may require topical antibiotics (GP review).
- Avoid eye make-up until healed.
Contact lens-related infections
- Most contact lens users wear them daily (disposed at end of day). Poor hygiene or overnight use can cause bacterial keratitis (corneal inflammation that may lead to ulceration).
- Symptoms: Pain, photophobia (light sensitivity), blurred vision.
- Never treat with OTC drops: Immediate ophthalmology referral required.
- Emphasise daily cleaning, disinfection, and lens-free periods during infection.
Viral infections
- Adenoviral conjunctivitis: Watery discharge and redness; contagious. Use lubricating drops and cold compresses.
- Antibiotics are ineffective.
- Herpes simplex keratitis: Painful, watery eye with possible corneal ulcer: Urgent referral for antiviral therapy (aciclovir).
- Herpes zoster ophthalmicus: Shingles affecting the eye; severe pain and rash on the forehead or nose. Require systemic antivirals within 72 hours.
Fungal and parasitic infections
- Fungal keratitis: Occurs after trauma involving plant matter.
- Acanthamoeba keratitis: Causes severe pain out of proportion to redness.
Both require hospital-based treatment (natamycin, amphotericin, or PHMB drops). Contact lens hygiene education is essential to prevention.
Supportive care
- Lubricants (hypromellose or carmellose sodium) relieve irritation.
- Cold compresses for viral infections; warm compresses for lid infections.
- Avoid contact lenses until full recovery.
- Discard eye drops after 28 days to prevent contamination.
Section 3: Complications and referral pathways
Complications can be severe but are rare, generally only occur if untreated.
Major complications
- Corneal ulceration (open sore on cornea): can scar or perforate.
- Orbital cellulitis (deep eye socket infection): presents with swelling and pain on movement.
- Chronic blepharitis: leads to lash loss and thickened lids.
- Herpetic scarring: From recurrent HSV keratitis.
- Fungal perforation: Can cause vision loss.
Red-flag symptoms (require same-day review)
- Severe pain or photophobia (light sensitivity).
- Unilateral redness (one eye only) with blurred vision.
- Visible white spot on cornea.
- History of trauma or daily contact lens use.
- Eye swelling or difficulty opening eyelid.
- Infants with purulent discharge.
Referral pathways
- Optometrist: Non-urgent slit-lamp examorlenscomplications.
- GP: If systemic antibiotics or antivirals are needed.
- Emergency Department: For vision loss, shingles eye involvement, or trauma.
Long-term complications
- Corneal scarring, reduced acuity.
- Persistent dry-eye symptoms after adenoviral infection.
- Recurrent herpes keratitis risk of permanent damage.
- Psychological distress is due to chronic discomfort.
Follow-up
Encourage return within 48 hours if there is no improvement. Reassess compliance, application technique, and hygiene practices.
References
1. HSE. Community Eye Care Guidance, Dublin: Health Service Executive, 2023. 2. NICE. Conjunctivitis – infective: antimicrobial prescribing (NG234), 2024.
3. CDC. Contact Lens Health Week – Educational Materials, 2023.
Section 4: Prevention and public health measures
Hygiene
- Wash hands regularly.
- Avoid touching or rubbing eyes.
- Usepersonaltowelsandpillowcases.
- Discard contaminated make-up or daily contact lenses used during infection.
- Do not touch dropper tips to lashes; discard bottles after 28 days.
Contact lens safety
Since most wear lenses daily, stress these key rules:
- Never rinse lenses or cases with tap water.
- Remove lenses before swimming or sleeping.
- Replace lens cases every one-to- three months.
- Ensure regular optometrist checks.
Vaccination and systemic health
- Shingles vaccine reduces risk of herpes zoster ophthalmicus.
- Influenza and MMR vaccines prevent viral eye complications.
- Good diabetes control helps prevent recurrent bacterial infections.
Additional clinical notes
- Advise patients with blepharitis to maintain long-term lid hygiene even after resolution.
- In allergic eye conditions, distinguish itching (allergy) from pain (infection).
- For recurrent infections, check for incomplete tear drainage (chronic dacryocystitis).
- Encourage review for any patient with recurrent ‘red eye’ to rule out uveitis (inflammation inside the eye).
Section 5: OTC pharmacy products for eye infections
From a pharmacist’s perspective, managing minor eye infections in the community practice relies heavily on effective over the counter (OTC) treatments and good patient counselling. Eye infections such as bacterial conjunctivitis, styes, and blepharitis are among the most common eye-related presentations in pharmacies. Pharmacists play a key role in triaging patients — identifying those suitable for self-care versus those requiring referral for more serious conditions, such as uveitis or keratitis.
Currently available OTC products for bacterial conjunctivitis include Brolene (propamidine isetionate) eye drops, which act as a mild antibacterial agent. Other preparations, such as GoldenEye drops, contain similar active ingredients but have been inconsistently available.
Lubricating artificial tear formulations (ie, Hylo-Forte, Systane, Optrex Dry Eye) are frequently recommended for symptomatic relief and to promote ocular comfort. For eyelid hygiene, especially in blepharitis, products such as Blephaclean wipes and Blephasol lotion are useful to remove crusting and debris along the lash line. Warm compresses and lid massage remain mainstays for managing styes and meibomian gland dysfunction.
Pharmacists also play a key educational role, advising on hygiene measures — such as avoiding contact lenses during infection, using separate towels, and handwashing — to prevent spread. While OTC management remains limited in scope, patient reassurance and evidence- based advice are crucial components of community pharmacy care.
OTC shortages and future developments
In recent years, intermittent shortages have affected key OTC eye preparations in Ireland, limiting pharmacists’ options for treating minor infections. The most notable example was the prolonged shortage of Brolene, a first-line OTC antibacterial eye drop, which left pharmacists with few alternatives. At present, Golden Eye, another widely used OTC antibacterial, is also unavailable, leaving lubricants and
lid hygiene measures as the mainstay of conservative care. There is currently no OTC ointment formulation suitable for styes, which further restricts management options for minor eyelid infections.
These limitations have highlighted the need for expanded pharmacist prescribing rights. The proposed Minor Ailments Scheme, expected to be implemented in 2026, is a welcome development.
Under this scheme, pharmacists will likely be permitted to prescribe chloramphenicol (Chloromycetin), an effective broad-spectrum antibiotic, for bacterial conjunctivitis without GP referral. This advancement would bring Ireland in line with UK practice, improve accessibility, and reduce pressure on general practice services.
Until then, pharmacists continue to rely on symptomatic treatment, hygiene advice, and clinical judgement to manage eye infections safely and effectively.
Disclaimer: Brands mentioned in this article are examples only and not meant as preference to other brands.
Written by Eamonn Brady MPSI (Pharmacist). Whelehans Pharmacies, 38 Pearse St and Clonmore, Mullingar. Tel 04493 34591 (Pearse St) or 04493 10266 (Clonmore). www.whelehans.ie. throughout Ireland. Email info@whelehns.ie
References
1. NICE. Conjunctivitis – infective: antimicrobial prescribing (NG234). 2024.
2. HPRA. Prescription-Only Medicines List. Updated 2025.
3. HSE Clinical Programme in Ophthalmology. Community Eye Care Guidance. Dublin: HSE; 2023.
4. Eustace P. Pharmacological management of eye infections in primary care. Irish Pharmacy
Journal. 2022.
5. Kilduff M, et al. Contact lens-related keratitis: Irish data review. Ir Med J. 2021.
6. College of Optometrists (UK). Bacterial Keratitis Guidelines. 2023.
7. World Health Organisation. Global Burden of Eye Disease. 2023.
8. RCOphth. Guidelines for the Management of Acute Red Eye. 2022.
9. PSI. Professional Guidance for Pharmacists on Medicine Supply. 2024.
10. Loughman J, et al. Public eye health in Ireland: pharmacist contribution. IPN. 2023.
11. BNF 88. Propamidine Isetionate (Brolene) – Monograph. 2024.
12. NHS SPS. Use of Topical Antibiotics in Conjunctivitis. 2023.
13. McElnea EM, et al. Microbial Keratitis in Ireland: 10-Year Review. Br J Ophthalmol. 2020.
14. NICE. Herpes simplex keratitis: clinical management (NG219). 2022.
15.HSE. Vaccination Guidance: Shingles, Influenza, MMR. 2024.
16. CDC. Contact Lens Health Week – Educational Materials. 2023.
17. HPRA. Reporting Adverse Reactions to Ophthalmic Products. 2024.
18. HIQA. Infection Prevention in Community Care. 2023.
19. European Society of Ophthalmology. Ocular Antimicrobial Stewardship Guidelines. 2022.
20. RCOphth. Uveitis and Inflammatory Eye Disease – Clinical Review. 2023.
21. Health Products Regulatory Authority (HPRA). Brolene® Eye Drops Summary of Product Characteristics. 2024.
22. National Institute for Health and Care Excellence (NICE). Conjunctivitis – infective: antimicrobial prescribing (NG208). 2021.
23.Pharmaceutical Society of Ireland (PSI). Guidance for pharmacists
on the ale and Supply of Non- Prescription Medicines. 2023.
24. Clinical Knowledge Summaries (CKS). Blepharitis and Stye. NICE, updated 2023.
25.Irish Pharmacy Union (IPU). OTC Medicines for Eye Conditions – Professional Guidance. 2024.
26.Department of Health (Ireland). Community Pharmacy Minor Ailments Scheme Implementation Framework. 2025 (proposed).







