Dr Donna Cosgrove MPSI gives a clinical overview of the different types of cholesterol and the various considerations in choosing a treatment.
Introduction
Globally, about a third of ischaemic heart disease can be attributed to high cholesterol.1 Cholesterol levels in the population are increasing due to both ageing and atherogenic lifestyles, despite being largely preventable with lifestyle management and medical treatment.2 In North America, the prevalence of dyslipidemia is estimated to be about 53 per cent.
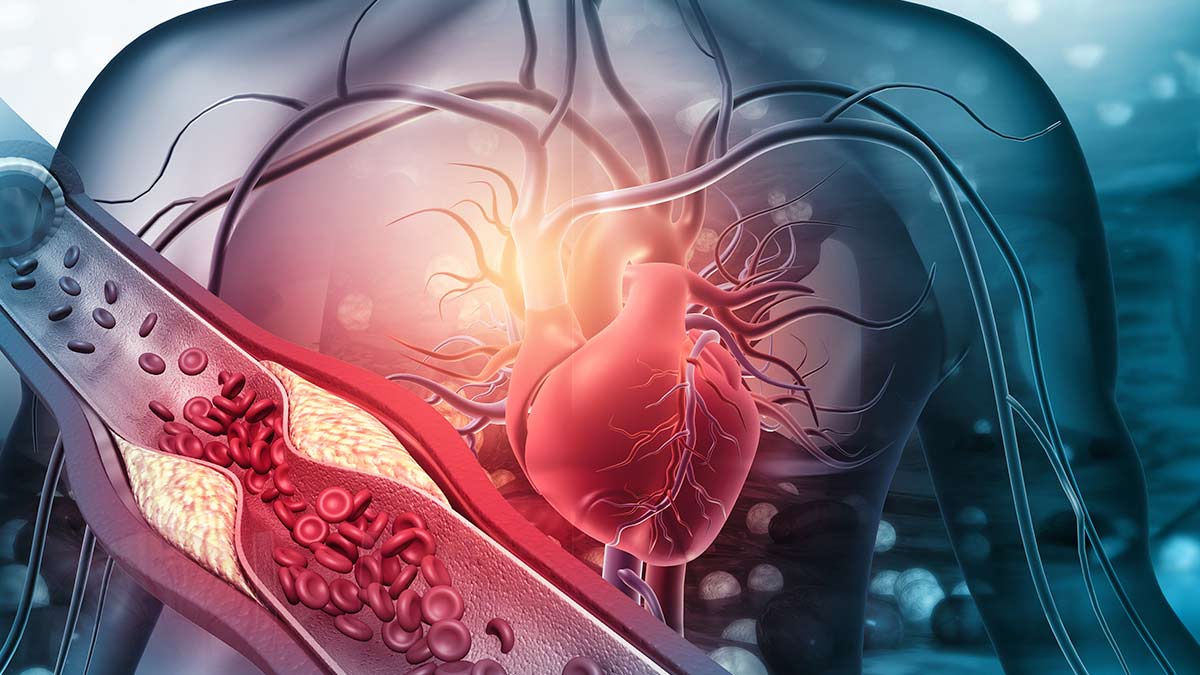
Cholesterol is consumed in the diet from the small intestine and transported to the liver, and also manufactured in the liver by HMG-CoA reductase. High levels of low-density lipoprotein (LDL-C) can lead to atherosclerosis: LDL-C can deposit in the arteries, become oxidised, and trigger an inflammatory response. Atherosclerotic plaques are formed, causing narrowing of the arteries.
The main risk factors for atherosclerotic cardiovascular disease (ASCVD) are:3
- Smoking
- Dyslipidaemia (ie, high levels of LDL-C, very low density lipoprotein (VLDL-C), triglycerides, and lipoprotein (a); and low levels of high-density lipoprotein (HDL-C)
- Hypertension
- Hyperglycaemia
- Age
- Lifestyle and genetic factors
Secondary causes of dyslipidaemia include excess alcohol intake, uncontrolled diabetes, hypothyroidism, liver disease, and nephrotic syndrome.
The QRISK tool (available online) offers a way to calculate estimated cardiovascular disease (CVD) risk4 within the next 10 years in people aged 25 to 84 based on an individual’s risk factors (but is not recommended for those at high risk of CVD, eg, in type 1 diabetes, chronic kidney disease, or familial hypercholesterolaemia). All people at risk of CVD should opt for a heart healthy diet, ie, low in saturated/trans fats, high in fruit, vegetables, and whole grains2, and a healthy lifestyle. Advice on and management for the following should be offered:4
- A cardioprotective diet (the Irish Heart Foundation has produced a leaflet5 about healthy cholesterol, available online)
- Aerobic and muscle strengthening
- Weight management
- Reducing alcohol consumption
- Smoking cessation
Although medications can start to reduce cholesterol levels within a week, it may take between 6-12 months to notice the impact of lifestyle modifications.
Healthy cholesterol levels
The Irish Heart Foundation lists the following cholesterol and triglyceride ‘healthy levels’:6
- Total cholesterol: ?5mmol/l
- LDL cholesterol: ?3mmol/l
- HDL cholesterol: ?1mmol/l
- Triglycerides: ?2mmol/l
For people with heart disease or diabetes:
- Total cholesterol: ?4.5mmol/l
- LDL cholesterol: ?1.8mmol/l
When looking at lipid levels initially, the total blood cholesterol and HDL-C should be measured for the best CVD risk estimate. However, rather than using black-and-white cut-off values alone, a full lipid profile (total, HDL-C, LDL-C, triglycerides) and a family history should be included in judgement of the likelihood of a familial lipid disorder.4
Familial hypercholesterolaemia
Familial hypercholesterolaemia (FH) is an inherited disorder that leads to pronounced elevation of LDL-C, leading to atherosclerotic plaque deposition in the coronary arteries and proximal aorta at an earlier age.7 This increases risk of cardiovascular events (stroke, myocardial infarction). Cholesterol deposits around the body may be visible, eg, xanthomas, which are deposits in the tendons, can be seen around the Achilles tendon or hands, and xanthelasmas can occur around the eyelids.
The clinical diagnosis is based on an elevated cholesterol, LDL >4.9mmol/l, with a triglyceride concentration within a normal range, and a premature family history of CVD.8 The Irish Heart Foundation estimates at least 10,000 people in Ireland have FH (with most likely to be undiagnosed). The Irish College of General Practitioners estimate that this figure could be as high as 20,000. When an individual is diagnosed with FH, cascade screening of family members may be facilitated in certain practices or clinics.
Pharmacological management
The Japanese biochemist, Prof Akira Endo, discovered statins from his work on fungal metabolites.3 HMG-CoA reductase inhibitors reduce hepatic cholesterol production, and lead to increased synthesis of LDL-C receptors, which remove LDL-C and VLDL-C from the bloodstream. From meta-analysis of statin randomised controlled trials (RCT), we now know that for every mmol/L reduction in LDL-C, there is an estimated 22 per cent reduction in ASCVD events.
Individual statins vary in their degree of cholesterol-lowering effect – rosuvastatin is twice as effective as atorvastatin (when compared mg per mg), and atorvastatin is twice as effective as simvastatin. Ezetimibe blocks absorption of cholesterol in the intestine and increases the activity of LDL receptors, reducing LDL-C by about 15-25 per cent.
Before starting statin treatment, there should be an informed discussion about the risks and benefits, as well as discussing the benefits of lifestyle changes.4 This should include advice regarding the risk of muscle-related side effects – ie, that it is small, and the risk of rhabdomyolysis is very low. Prior to starting statins, in addition to a full lipid profile, renal function, transaminase level, and TSH should be measured. In primary prevention of CVD a reduction of at least 40 per cent is the aim.
Atorvastatin 20mg is recommended for most patients as the first-line treatment for primary prevention of CVD. Atorvastatin 80mg is recommended for people with CVD. If the target is not reached with the recommended dose, ezetimibe can be added to further reduce CVD risk. However, adherence to medication and lifestyle measures should also be discussed. If someone experiences adverse effects with a high intensity statin (ie, atorvastatin 20-80mg; rosuvastatin 10-40mg), there are a few options:
- Stop the statin and try again after symptoms have resolved to see if they are related to the statin
- Change to a different statin (eg, rosuvastatin)
- Reduce the dose
- Change to a lower intensity statin
- If a statin is contraindicated/not tolerated at any dose, offer ezetimibe instead.
A statin at any dose reduces CVD risk. Statins also reduce the risk of haemorrhagic stroke.9
The PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitors alirocumab (Praluent) and evolocumab (Repatha) increase the clearance of LDL-C from the bloodstream.10,11 These are available under the High Tech Scheme.
Statin drawbacks
Statins are usually well tolerated but nonetheless statin-associated symptoms (SAS) have been identified, including statin-associated muscle symptoms (SAMS), diabetes, and central nervous system effects.9 SAS are rare in clinical trials.
- SAMS is the most frequent (10-15 per cent of patients). There are no validated clinical tests or diagnostic criteria for statin-associated myalgia. For this reason, the diagnosis of SAMS, based on symptoms like myalgia and cramps, is subjective. Creatine kinase (CK) levels are often normal in patients with possible SAMS, whereas many asymptomatic patients taking statins have elevated CK levels.
- All statins appear to produce a small increase in the risk of new onset diabetes, but this is greatly outweighed by their bene?t. A meta-analysis estimated just one additional case of diabetes per year would occur for every 498 patients treated with intensive versus moderate statin therapy, ie, intensive statin therapy would prevent 3.2 CVD events for each new case of diabetes mellitus (DM). The mechanism behind this is unknown, but may be related to LDL-C reduction. This implies that it may also occur with other powerful lipid-lowering agents, eg, PCSK-9 inhibitors.
- It has been observed in multiple studies that statins are linked to a reduction in cognitive decline and Alzheimer’s Disease in older adults; and other studies have shown neither a positive or negative effect. Based on the FDA adverse events reporting system, a warning is now included in the States about a potential link to ‘memory loss and confusion’, although this has been controversial given the lack of strong evidence linking statins and declining cognitive function.
- Elevated LFTs are associated with statin use especially in the first three months, but liver failure associated with statin use is very rare.
- Similarly, in terms of renal function, studies do not suggest any detrimental effect.
- There is a possible association between statins and depression, although the evidence is inconclusive. Membrane cholesterol is important for serotonin receptor function, meaning a reduction in cholesterol could in theory alter serotonin binding and signalling.
Multiple trials12.13 have looked specifically at side-effect rates associated with statins. The SAMSON (Self-Assessment Method for Statin Side-effects or Nocebo) trial13 included participants who previously experienced side effects from statins that were significant enough to abandon statin therapy. In this study, each of these participants underwent a protocol of statin (atorvastatin), placebo, and no tablets for one year (a three-arm crossover design), where each individual acts as their own control. Results showed that side effects mainly arose from taking a tablet in general rather than taking a statin. This ‘nocebo effect’ has been suggested to be responsible for up to 90 per cent of side effects from statins.
Cholesterol reducing foods and supplements
Due to reported side effects attributed to and reluctance to take statins, many people seek alternative ways to reduce cholesterol that include functional foods and supplements. NICE guidance does not advise the use of plant stanols/sterols, or omega-3 fatty acid compounds for CVD prevention; or the use of coQ10/vitamin D to increase adherence to taking statins.4 On the other hand, a review published in Nature Reviews Endocrinology2 refers to a reduction of 5-15 per cent in LDL-C levels with a 2-3g intake of plant sterols daily (but no impact on total cholesterol).
A Cochrane review looking at the effects of omega-3 fats on cardiovascular health ultimately found that increasing levels of eicosapentaenoic acid/docosahexaenoic acid (EPA/DHA) has little or no effect on cardiovascular health and mortality.14 There is some low quality evidence that alpha-linolenic acid (ALA) might slightly reduce cardiovascular events and related mortality. There is also evidence that eating two servings of oily fish per week can reduce triglyceride levels. Elsewhere, there is evidence to suggest that fish oils reduce triglyceride levels (25-30 per cent reduction with a dose of 2-4g fish oils daily).2
Soluble fibre (found in oats and barley) can bind to cholesterol and bile acids in the gut which inhibits their absorption. Studies have identified that an increased intake of soluble fibre is associated with lower levels of total and LDL cholesterol.2
Red yeast rice, produced by fermentation of rice by a species of mould, contains the active ingredient monacolin k, which is in fact the first statin that was isolated and used for treatment (lovastatin). Lovastatin/monacolin k containing red yeast rice supplements reduce total and LDL-C and triglycerides and may be helpful in people who prefer more alternative approaches to prescription medication.
As with many diseases, a link between blood cholesterol levels and gut bacteria has been identified. Recent research from the Framingham Heart Study15 showed that elevated levels of gastrointestinal Oscillibacter species were associated with more favourable levels of triglycerides and glucose, and higher HDL-C. The mechanism behind this appears to be the metabolism of cholesterol in the intestine by Oscillibacter using bacteria-specific enzymes. This may eventually lead to another avenue of cholesterol treatment.
References
- World Health Organisation. Raised Cholesterol. (2024) Available at: www.who.int/data/gho/indicator-metadata-registry/imr-details/3236.
- Hunter, PM, & Hegele, RA (2017). Functional foods and dietary supplements for the management of dyslipidaemia. Nature Reviews Endocrinology, 13(5), 278-288.
- Grundy SM, Feingold KR. Guidelines for the Management of High Blood Cholesterol. [Updated 2022 May 28]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available at: www.ncbi.nlm.nih.gov/books/NBK305897/.
- National Institute for Health and Care Excellence. (2023). Cardiovascular Disease Risk: Assessment and Reduction [NG238]. Available at: www.nice.org.uk/guidance/ng238/resources/cardiovascular-disease-risk-assessment-and-reduction-including-lipid-modification-pdf-66143902851781.
- Irish Heart Foundation A Healthy Cholesterol (2018). Available at: www.irishheart.ie/wp-content/uploads/2020/05/47376-IHF-HEALTHY-CHOLESTROL.pdf.
- Irish Heart Foundation. (2020). Cholesterol. Available at: www.irishheart.ie/how-to-keep-your-heart-healthy/cholesterol/.
- Ison HE, Clarke SL, Knowles JW. Familial Hypercholesterolemia. In: Literature Cited. University of Washington, Seattle, Seattle (WA); 1993. PMID: 24404629.
- Homeniuk, R, Gallagher, J, & Collins, C. (2022). A mixed methods study of the awareness and management of familial hypercholesterolaemia in Irish general practice. Frontiers in Medicine, 9, 1016198.
- Thompson, PD, Panza, G, Zaleski, A, & Taylor, B (2016). Statin-associated side effects. Journal of the American College of Cardiology, 67(20), 2395-2410. Available at: www.jacc.org/doi/abs/10.1016/j.jacc.2016.02.071.
- DrugBank Online. (2024). Evolocumab. Available at: https://go.drugbank.com/drugs/DB09303.
- DrugBank Online. (2024). Alirocumab. Available at: https://go.drugbank.com/drugs/DB09302.
- Wood, FA, Howard, JP, Finegold, JA, Nowbar, AN, Thompson, DM, Arnold, AD, … & Francis, DP (2020). N-of-1 trial of a statin, placebo, or no treatment to assess side effects. New England Journal of Medicine, 383(22), 2182-2184.
- Howard, JP, Wood, FA, Finegold, JA, Nowbar, AN, Thompson, DM, Arnold, AD, … & Francis, DP. (2021). Side effect patterns in a crossover trial of statin, placebo, and no treatment. Journal of the American College of Cardiology, 78(12), 1210-1222. Available at: www.jacc.org/doi/abs/10.1016/j.jacc.2021.07.022.
- Abdelhamid, AS, Brown, TJ, Brainard, JS, Biswas, P, Thorpe, GC, Moore, HJ, … & Hooper, L (2018). Omega?3 fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database of Systematic Reviews, (11). Available at: www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD003177.pub3/full.
- Li, C, Stražar, M, Mohamed, AM, Pacheco, JA, Walker, RL, Lebar, T, … & Xavier, RJ (2024). Gut microbiome and metabolome profiling in Framingham heart study reveals cholesterol-metabolising bacteria. Cell, 187(8), 1834-1852.