Donna Cosgrove MPSI provides a clinical overview of some of the mental and physical considerations in men’s health
“A men’s health issue is a disease or condition unique to men, more prevalent in men, more serious among men, for which risk factors are different for men, or for which different interventions are required for men.”1 Men’s health encompasses a broad range of areas, including reproductive and sexual health, cancer treatment and prevention, cardiovascular disease, and mental health.
The Men’s Health Forum in Ireland (MHFI) was established across Ireland to address the poor health status of males in the country. Research published by MHFI in 20222 indicates that neoplasms, circulatory system disease, respiratory system disorders and external causes of injury and poisoning are the major causes of death of males in Ireland (Figure 1) . However, compared to a 2004 report, death rates from these have reduced due to, ie, the adoption of healthier lifestyles, screening programme uptake, better diagnostic tools and treatment options, improvement in health literacy and help-seeking behaviours, and increased life span.
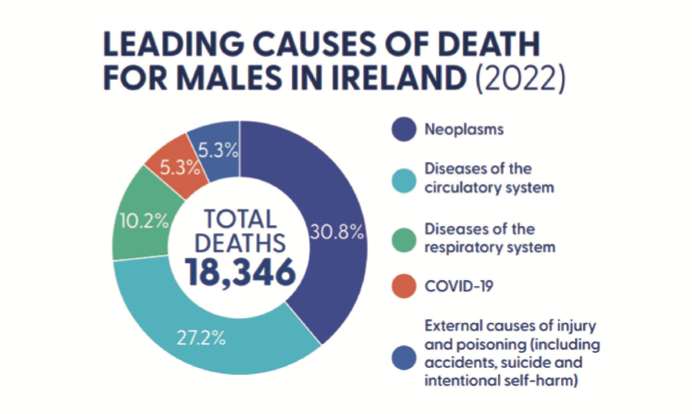
Figure 1: Leading causes of death for males in Ireland, 20222
Important points in this Men’s Health in Numbers report include the following:
- Overweight and obesity: In 2022, 23 per cent of males were overweight, and 40 per cent were obese.
- Smoking: The rate of smoking in males has fallen from 24 per cent in 2015 to 21 per cent in 2023. Overall, male deaths by suicide have fallen, from 445 in 2012 to 331 in 2022.
- Cancer: 30.8 per cent of male deaths in Ireland are attributable to cancer, with the most common types being lung (21 per cent), prostate (12 per cent), colorectal (11 per cent), pancreas (6 per cent) and oesophagus (6 per cent).
- Prostate cancer: This is the most frequently diagnosed cancer among males in Ireland.
- The mortality rate for all invasive cancers has decreased: The survival rate has increased from 40 per cent (1994-1998) to 65 per cent (in 2014-2018).
- Heart attacks: 77 per cent of people treated for a major heart attack in 2021 were men.
- The rate of STIs has increased: The number of males diagnosed with gonorrhoea in 2010 was 478, compared to 3,922 in 2022. There were 243 new diagnoses of HIV among males made in 2012 and 586 made in 2022.
Mental health
In the UK and Ireland, men are three-to-four times more likely to die by suicide than women.3 In particular, men who are less well-off and living in the most deprived areas are up to 10 times more likely to die by suicide than men from affluent areas. Middle-aged men (40-to-59) also experience higher suicide rates than other groups (Figure 2). This trend in suicide rates has persisted for decades.
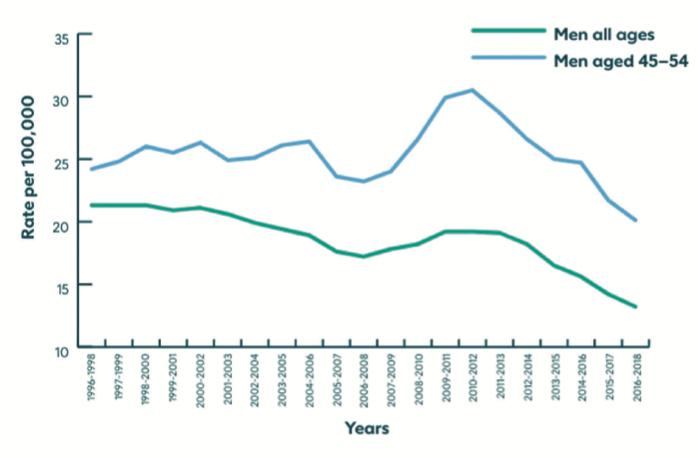
Figure 2: Suicide rates in middle aged men (45-54) and men of all ages3
The Samaritans published a report on the wellbeing and support services available for less well-off, middle aged men, including their experiences navigating available services.3 The report indicated that:
- Strong social connections are one of the strongest predictors of positive emotional wellbeing, with persistent loneliness being a risk to this.
- Men can feel constrained by expectations of the male ‘role’ placed on them by society, ie, the perceived role as father, brother, partner, son, meaning that it isn’t their place to open up and be seen as a burden.
- Purposeful activity is very important for wellbeing: Employment, hobbies, interests.
- The men interviewed found that there was limited effective support available, ie, before ‘crisis point’. There were missed opportunities like the point of job loss, contact with health professionals, or with the justice systems, that could have been useful points of engagement and referral to appropriate services.
Prostate cancer
Nearly 4,000 men are diagnosed with prostate cancer every year in Ireland.4 Early, localised prostate cancer is cancer that has not spread beyond the prostate. There may be no symptoms in early prostate cancer, but it may be suspected after a PSA test. Symptoms of prostate cancer don’t usually manifest until the prostate is large enough to affect the urethra, at which stage symptoms include:
- Increased urinary frequency and urgency.
- Straining.
- Feeling of incomplete bladder emptying.
- Weak flow.
- Blood in urine/semen.
Some of these may just be signs of benign prostate enlargement, however, rather than cancer.
The risk of developing prostate cancer:
- Increases with age.
- Is higher in black men.
- Is lower in Asian men.
- Is heritable.
- Is higher in obesity.
- Is potentially increased in men with high calcium intake.
There is no single definitive test for prostate cancer. Rather, there are multiple tests available to diagnose the condition that include:
- Blood tests (ie, prostate-specific antigen, PSA, test).
- Digital rectal examination.
- MRI scan.
- Biopsy (transperineal or transrectal).
PSA tests may not be reliable, as values can be raised by other conditions unrelated to cancer. However, a raised PSA level may mean additional tests are required. Additionally, one-in-seven normal PSA test results may have prostate cancer (false negative).
Management options include watchful waiting, active surveillance, radiotherapy (with or without hormone therapy), and prostatectomy.6 There is evidence that future urinary and sexual function is better for men who are offered active surveillance or radiotherapy rather than prostatectomy.
Watchful waiting is often chosen in older men when any cancer present is not likely to have any impact on their natural lifespan.5 Active surveillance includes having regular PSA tests, MRI scans and/or biopsies to identify any cancer progression as early as possible. If treatment is preferable, radical prostatectomy (with or without radiotherapy) is an option for localised prostate cancer. After this procedure, ejaculation is not possible, so it may be necessary for the patient to speak about storing a sperm sample for IVF. Brachytherapy, a type of radiotherapy delivered via implanting tiny radioactive seeds or needles into the tumour, is an alternative option. Hormone therapy, often used with radiotherapy, blocks the effects of testosterone in the body, particularly the proliferation of the prostate cancer cells. Another procedure called trans-urethral resection of the prostate (TURP) helps relieve the pressure on the urethra, treating problematic urinary symptoms, although this does not treat the cancer.
Male sexual dysfunction
Sexual dysfunction in males becomes more common as men get older. This includes erectile dysfunction, diminished libido and ejaculatory disorders.7 Healthy and normal function depends on interactions between many systems: Vascular, neurobiological, hormonal and psychological. Nitric oxide, the vasodilator, has an important role in erectile dysfunction (ED). Low nitric oxide synthase levels have been found in cigarette smokers and patients with diabetes and testosterone deficiency which may explain why these factors are linked to ED.
The Massachusetts Male Aging Study (MMAS) reported that male sexual dysfunction is usually initially seen in the early 40s, and increases with age. At age 40, 40 per cent of men taking part in the MMAS acknowledged some degree of impaired function, however, data from the National Health and Social Life Survey indicated that 31 per cent of younger men (18-to-59 years) also reported sexual dysfunction.
The most common type of sexual dysfunction in men is ED. Risk factors for ED, apart from increasing age, include cardiovascular disease, diabetes, hypertension, dyslipidaemia, hypogonadism, smoking, depression and medication use. Many commonly prescribed medications can impact sexual function (Table 1).
| Class | Type |
| Antidepressants (ED and low libido) | Most, but especially SSRIs |
| Antihypertensives (ED) | Diuretics Beta blockers (Angiotensin receptor blockers, nebivolol and alpha blockers may have a beneficial effect) |
| Anti-androgens | Bicalutamide |
| Opioid analgesics (low libido) | Oxycodone Morphine |
| Other | Spironolactone Sympathetic blockers (e.g. clonidine) Ketoconazole Cimetidine |
| 5-alpha reductase inhibitors (low libido) | Finasteride Dutasteride |
Table 1: Medications linked to sexual dysfunction in males
Reduced libido is thought to affect between 5 and 15 per cent of men, and increases with age. Low libido and ED are sometimes due to the same issue such as depression or hypogonadism. The development of ED itself is linked to an increased risk of depression.
Treatment of sexual dysfunction in men aims to improve libido, acquire/sustain erections, and treat premature ejaculation.8 Choice of treatment varies depending on desired outcome, and aetiology (vasculogenic, neurogenic, psychogenic). Therapies that treat ED include PDE-5 inhibitors, penile self-injections with vasoactive drugs, intraurethral suppositories, vacuum erection devices, or penile prosthesis. PDE-5 inhibitors are generally considered as first-line pharmacotherapy due to their efficacy levels, ease of use and favourable side-effect profile.
Different drugs in this class appear to demonstrate comparable efficacy. If these are not effective, vacuum devices, penile self-injectable drugs and intraurethral alprostadil are second-line options. If depression or anxiety is a significant contributing factor, psychotherapy alone or in combination with pharmacotherapy can help.
Sildenafil and tadalafil are all phosphodiesterase (PED-5) inhibitors which enhance cyclic GMP activity. Cyclic GMP mediates the nitric-oxide induced vasodilation in initiating/maintaining an erection. Intracavernosal levels of cGMP are increased by PDE-5 inhibitors, increasing the number and duration of erections.
PDE-5 inhibitor counselling points:
- Sildenafil: Oral administration one hour before sex, effective for up to four hours. Dose is 50-to-100mg on an empty stomach. Sildenafil has the best safety record of all PDE-5 inhibitor drugs.
- Tadalafil: Tadalafil has a longer duration of action than sildenafil. Dose for as-needed treatment is 10-to-20mg about 30 minutes before sexual activity. Lower doses (2.5-to-5mg) are available for once-daily administration, and appear to be as effective as taking higher doses as needed, eliminating any issues around onset and duration of action.
- Stimulation is required for erection with all PDE-5 inhibitors.
- PDE-5 drugs may lower blood pressure due to their vasodilator action, and are contraindicated in certain cardiovascular diseases, men taking nitrates, and used cautiously in men taking alpha blockers due to an increased risk of hypotension.
- The most common ADRs reported are flushing, headaches and dyspepsia (12, 11 and 5 per cent respectively with sildenafil).
- ‘Blue vision’ is occasionally reported in men using sildenafil: The PDE-5 inhibitor can react with PDE-6, present in the retina, which plays a role in colour vision. This is transient, lasting two-to-three hours.
- Lifestyle measures and pharmacological treatment for cardiovascular risk factors, ie, smoking, obesity, hypertension, and dyslipidaemia, can help with prevention and treatment of ED.
Health promotion, education and early interventions are vital for improving men’s health outcomes. Diet and lifestyle changes can change the trajectory for many diseases including cardiovascular, reproductive and sexual health, and cancer risk. In other areas including mental health, the importance of factors such as social connection and purposeful activity are becoming more widely acknowledged, and can help foster a more holistic discussion on health and wellbeing in men.
References
- Devine, P. (2024), Men’s Health in Numbers: Republic of Ireland Men’s Health Report Card 2024. Dublin: Men’s Health Forum in Ireland. Available https://www.mhfi.org/MensHealthInNumbers2.pdf
- Fletcher, R. (1997). Report on Men’s Health Services. Prepared for NSW Department of Health by Men’s Health Advisory Group. Family Action Centre, University of Newcastle. NSW 2318, Australia.
- Samaritans. (2020). Out of sight, out of mind: why less well-off, middle aged men don’t get the support they need. Available https://media.samaritans.org/documents/Samaritans_-_out_of_sight_out_of_mind_2020.pdf
- Irish Cancer Society. Prostate Cancer. (2024). Available https://www.cancer.ie/cancer-information-and-support/cancer-types/prostate-cancer#:~:text=Prostate%20cancer%20is%20a%20common,spread%20outside%20your%20prostate%20gland.
- National Health Service. (2021). Prostate Cancer. Available https://www.nhs.uk/conditions/prostate-cancer/
- National Institute for Health and Care Excellence. (2021). Prostate Cancer: Diagnosis and Management [NG31]. https://www.nice.org.uk/guidance/ng131/resources/prostate-cancer-diagnosis-and-management-pdf-66141714312133
- Rosen, R.C., Kera, M. (2024). Epidemiology and etiologies of male sexual dysfunction. Retrieved July 31st, 2024, from https://www.uptodate.com/contents/epidemiology-and-etiologies-of-male-sexual-dysfunction
- Khera, M. (2024). Treatment of male sexual dysfunction. Retrieved July 31st, 2020, from https://www.uptodate.com/contents/treatment-of-male-sexual-dysfunction?search=ed%20treatment&source=search_result&selectedTitle=1%7E150&usage_type=default&display_rank=1#H1







