Men’s health encompasses a wide range of issues that are unique to men and affect their physical and mental wellbeing. These issues can be related to sexual health, reproductive health, mental health, cardiovascular health, or a wide range of other issues. In comparison to women, men often take more risks with their health, are less likely to be aware of disease symptoms and use primary care services less often.(1) All these reasons give rise to men having poorer health outcomes than women. This is reflected in a lower life expectancy
for men, with women expected to live for 3.9 years longer in Ireland.(2)Even though men appear to have worse health outcomes, men’s health doesn’t have the same recognition as a distinct field in research. A study has shown that over a 48-year period, the term ‘women’s health’ appeared in the title or abstract of papers in PubMed almost 10 times more than the term ‘men’s health’. (3) The HSE organise a men’s health week to encourage improvements in men’s health through the likes of smoking cessation, healthy eating, reducing substance abuse and increasing physical activity.(4) There are many prominent conditions that are particularly important in men’s health, and these are outlined below.
ERECTILE DYSFUNCTION (ED)
ED can be defined as the inability to attain or maintain an erection for satisfactory sexual intercourse. ED can occur occasionally or more regularly and can vary in severity from mild (a soft erection) to severe (not able to attain an erection at all).(5) The cause of erectile dysfunction is often multifactorial and can be physical, psychological, lifestyle-related, drug-induced, or due to surgery. Ageing is an important risk factor contributing to ED, although many co- morbidities are present as an individual ages which can also play and important role.(6)
Cardiovascular disease is a significant risk factor for ED, with almost of men with coronary artery disease also having significant erectile dysfunction. This is partly due to the fact that the coronary arteries and the cavernosal arteries develop atherosclerotic plagues similarly. The cavernosal arteries have a smaller diameter than coronary arteries and therefore ED can often be observed before coronary artery disease develops. Studies have shown that men with ED have 44% more cardiovascular events than with men without ED. There are several other conditions that have a strong correlation with ED, and these include hypertension, hyperlipidaemia, diabetes, and hypogonadism.(6)
Lifestyle factors can also play a role and must be considered when evaluating ED. Diets high in saturated fat, obesity, alcohol, smoking and recreational drug use are associated with an increased risk of ED. There can be psychological factors to consider with ED. Stress, depression and performance anxiety are all associated with ED.(7) A total of 25% of ED cases are thought to be due to prescription medication. Antidepressants (particularly selective serotonin reuptake inhibitors (SSRIs)), antihistamines, thiazide diuretics, antifungals and some antihypertensives are among the main drugs that have ED as a possible adverse side effect. Finally, prostate cancer patients that have had prostatectomy surgery experience ED in 85% of cases.(6)
TREATMENT
Phosphodiesterase-5 (PDE-5) Inhibitors
There are different treatment options available for ED. Oral PDE-5 inhibitors are the first line treatment of ED, with sildenafil and tadalafil the most commonly used. PDE-5 inhibitors are effective in treating ED caused by a range of etiologies. They work by inhibiting phosphodiesterase which causes a decrease in the breakdown of cyclic guanosine monophosphate GMP and leads to increase in cavernosal smooth muscle relaxation and arterial blood flow. Sexual stimulation is still required after taking PDE-5 inhibitors to release nitric oxide from the vascular endothelium to initiate an erection. They have a high rate of efficacy, with a success rate of up to 76%. If treatment initially fails with a PDE-5 inhibitor, the patient should try at least
one more as up to 50% will respond to a different drug. PDE-5 inhibitors should not be used with nitrates due to potentially dangerous hypotension, with caution necessary with all antihypertensives and alpha-blockers. Approximately 40% of patients will experience some side effects but are usually mild and include headache, indigestion, dizziness, and light sensitivity. There are reports of blindness or deafness, but these are very rare. PDE-5 inhibitors have maximum recommended dosing of once daily.(6) The recommended dose of sildenafil is 50mg as required. Depending on tolerability and efficacy, the dose can
be increased to 100mg or reduced to 25mg. Sildenafil should be taking on an empty stomach due to poor absorption.(8) The recommended dose of tadalafil is 10mg, increasing to 20mg if required.(9)
In 2021, Viagra Connect (50 mg sildenafil) was launched as an over-the-counter (OTC) medication in the Republic of Ireland. A pharmacist must carry out a thorough consultation to ensure it is suitable for the patient and will ask questions on concomitant medication use, concomitant conditions, and cardiovascular health. The general health of the patient should be established, and they should be told to visit their GP within six months of starting Viagra Connect. Patients should be fully counselled on how to take the medication, potential side effects, warning signs to look out for and general lifestyle advice.(10)
OTHER TREATMENT OPTIONS
Other pharmacological and non- pharmacological treatment options exist and may be explored. L- arginine is an amino acid that is essential for the production of nitric oxide in the body. Several studies have demonstrated efficacy of L-arginine supplementation (1,500 mg to 5,000 mg) in treating mild to moderate ED.(6) Vacuum erection devices are another treatment option for ED patients. It involves placing a cylinder over the penis with an airtight seal and then using a vacuum pump to create negative pressure and increases blood flow to the penis. This treatment is generally safe, effective, inexpensive, and non-invasive. The use of the device requires training for optimal performance.(6) and adverse effects can include haematoma and capillary bleeding.(7)
If PDE-5 inhibitor therapy fails, intracavernosal injections or intraurethral suppositories may be used. Intracavernosal injections involve the injecting of vasoactive substances directly into the penis using
a small needle. These substances include prostaglandin E1, papaverine and phentolamine. Efficacy can be up to 94% but dropout rates can be high due to high cost and problems with the concept of penile injections. Intraurethral suppositories involve placing a prostaglandin E1 inside the urethra, where it is gently massaged to disperse the medication before sexual intercourse.(7)
LIFESTYLE MODIFICATIONS
Lifestyle management can have a very important role in managing ED, particularly in younger individuals. Reversible risk factors that may cause ED should be identified
and include poor diet, smoking status, alcohol intake, obesity, and medication. Weight loss in obese patients, as well as increasing exercise can play a vital role as part of a treatment plan. Chronic alcohol consumption and smoking can contribute to ED. Smoking cessation and reducing alcohol intake can be important in the management of ED. If ED is thought to be drug-induced, the patient may benefit from a change in medication. Patients with psychological issues may also benefit from counselling with an appropriate professional. All these lifestyle modifications are recommended to precede or accompany any other treatment choices.(7)
TESTICULAR CANCER
Although testicular cancer accounts for approximately 1% of male tumours, it is the most common cancer in men aged 15-45 years. It is one of the most curable malignancies when identified early and treated appropriately. The incidence has been increasing significantly in recent years. The prognosis is generally excellent with a greater than 95% five-year survival rate with proper treatment. Environmental risk factors for testicular cancers can include testicular trauma, cryptorchidism and various infections including human immunodeficiency virus (HIV), human papillomavirus (HPV), Epstein-Barr virus (EBV), cytomegalovirus (CMV). There are genetic risk factors to be considered also.(11) Typical symptoms that should be monitored by all males include a painless swelling or lump in the testicles or a change in shape or texture of the testicles. The size of the lump can vary but should always be referred to a doctor. Other symptoms can include increased firmness, difference in appearance or a feeling of heaviness of a testicle. A dull ache or acute pain can also be a symptom of testicular cancer. All men should know how to carry out a testicular self-examination and should carry one out regularly (12) (13).
Ultrasound imaging in combination with physical examination has close to 100% sensitivity in the diagnosis of testicular cancer. Tumour markers can also be used in the diagnosis of testicular cancer. A hard intratesticular mass is usually diagnostic of testicular cancer but other diagnoses to consider mass include epididymo-orchitis, hematoma, inguinal hernia, and hydrocele. Treatment of testicular cancer can vary depending on several factors. Orchiectomy (surgical removal of one or more testes) is the initial management strategy, with chemotherapy and radiotherapy also treatment options.(11)
Complications are common with testicular cancer and the treatment of it. Complications secondary to the disease include metastasis, fatigue, anxiety, and venous thromboembolism. Metastasis in other organs is the main adverse variable in the prognosis of the disease. Patients should be observed for metastasis and additional imaging with computed tomography (CT) scans should
be performed for staging when metastatic disease is suspected. Complications secondary to treatment can include infertility, infection, tinnitus, hearing loss, peripheral neuropathy, and hypogonadism. Adequate counselling should be provided to patients regarding the possibility of infertility. Sperm banking should be considered, particular in patients with bilateral testicular pathology, for use in later life.(11)
HYPOGONADISM
Hypogonadism refers to decreased function of the gonads and can lead to diminished production of testosterone.(14) Primary hypogonadism is caused by testicular failure and can be due to injury, infection, tumour, chemotherapy, or alcohol abuse. It is characterised by low serum testosterone levels, and high luteinising hormone (LH) and follicle-stimulating hormone (FSH) concentrations. It is associated with low LH and FSH levels. Secondary hypogonadism is associated with low LH and FSH levels and can be due to several reasons including Kallmann’s syndrome, pituitary tumours, radiation treatment and various medications.(15) Hypogonadism is commonly under-reported, with some studies suggesting that approximately 40% of men older 45 have hypogonadism.(14) There are several signs and symptoms related to low testosterone levels that are indicative of hypogonadism. These symptoms include reduced libido, erectile dysfunction, decreased testicular volume, depressed mood, increased body fat, decreased muscle mass, increased fatigue, low sperm count, decreased physical performance, and loss of body hair. As none of these symptoms are unique to hypogonadism, therefore one or more of these symptoms must be present along with a low testosterone concentration for a diagnosis to be confirmed. Total serum testosterone can be measured using a blood test. Testosterone is subject to circadian rhythm so the blood test should be performed in the morning. Although there is no definite score that indicates a man is hypogonadal, 300 ng/dl is considered a low testosterone level and 230 ng/dl is a score below which individual will benefit from testosterone replacement treatment (TRT).(14)(15)
There are several TRT options including oral, buccal, transdermal gels, transdermal patches, and intramuscular injections. The treatment objective is to increase blood testosterone levels to the normal range. Testosterone gels are the most commonly used treatment option. Testosterone gels have the advantages of being convenient, relatively inexpensive, have patient preference and can maintain stable serum testosterone concentrations. Gels should generally be applied to be shoulders or upper arms and have a once daily dosing regimen. Studies have demonstrated that patients have an improvement in libido, mood, sexual function, and energy once testosterone
levels are restored to a stable normal range. Reduction in body fat, increase in muscle mass and improvement in BMD can be observed after up to six months of treatment. There are a number of contraindications
to TRT and these include prostate cancer, breast cancer, uncontrolled heath failure, haematocrit level greater than 48%, untreated obstructive sleep apnoea and prostate specific antigen (PSA) above 4ng/ml. Prior to commencing therapy, a digital rectal exam (DRE), haematocrit, haemoglobin, PSA and testosterone levels should all be carried
out. A bone mineral density measurement may also be carried out as hypogonadism
is a major risk factor for male osteoporosis. Testosterone level should be monitored one month after initiating treatment. All tests should be repeated at three to six months during the first year of treatment.(14)(15)
PROSTATE DISORDERS
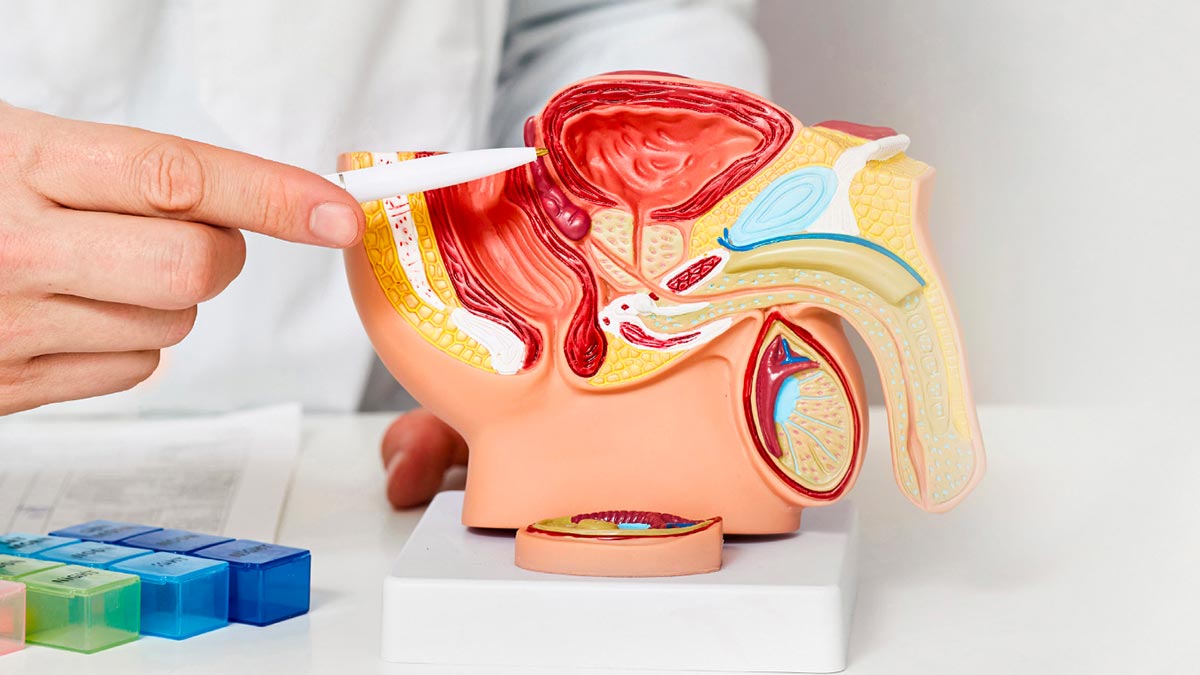
The prostate is a small gland found in men that produces fluid that is an important component of semen. In addition to this, the change of shape of the prostate helps to facilitate the switch between ejaculation and urination in men. Prostate problems are common, particularly in men aged over 50. The main disorders of the prostate are prostatitis, prostate cancer, and benign prostatic hyperplasia (BPH).(16)
BENIGN PROSTATIC HYPERPLASIA
BPH is a non-malignant growth of prostate tissue and is increasingly prevalent with advancing age. The prevalence has been estimated to be as high as 50-60% for
men in their 60s, increasing to 80-90% for males over the age of 70. Other risk factors for BPH include genetics, diet, diabetes, and heart disease. The etiology of BPH is thought to be due to the increased activity of aromatase and 5-alpha reductase enzymes, which occur as males age. These hormones cause a decrease in testosterone and an increase in estrogen and dihydrotestosterone (DHT) in the body and is associated with prostate enlargement. The main symptoms of BPH are in the lower urinary tract and include increased frequency of urination, increased urgency, nocturia, urinary hesitancy, weak urinary stream, and a sensation of incomplete voiding. Diagnosis is generally based on history of symptoms, a DRE and exclusion of other causes of similar symptoms.(17) Complications of BPH can include urinary retention, bladder calculi, haematuria, and chronic urinary tract infections.(18)
TREATMENT
Active surveillance may be used in males with minor symptoms, and they may be provided with lifestyle advice which may help their symptoms. Lifestyle modification including weight loss, reducing fluid intake in the evening and cutting intake of caffeine can all provide some symptom relief. However, pharmacological treatment is often necessary.(18)
Alpha-blockers including tamsulosin, doxazosin, silodosin, and alfuzosin are often used in the treatment of BPH. They exert their mechanism of action by blocking alpha 1-adrenoreceptors on prostate smooth muscle and bladder neck which leads to improvement in symptoms. The 5 alpha- reductase inhibitors work by blocking the conversion of testosterone to DHT and therefore causing shrinkage of the prostate. Finasteride and dutasteride are examples
of 5 alpha-reductase inhibitors. They can take several weeks to show improvement in symptoms, with up to six months needed for full effectiveness.(18) Dutasteride and tamsulosin is available as a combination product with a once daily dosing regimen.(19)
Increased urgency and increased urination frequency can be treated with muscarinic receptor antagonists such as solifenacin, tolterodine, and oxybutynin. They block muscarinic receptors on detrusor muscle and provide relief from these symptoms. If antimuscarinic therapy fails, a beta-3 adrenoreceptor agonist, such as mirabegron, may be considered. Combination therapy with both an alpha- blocker and alpha-reductase inhibitor has been shown to be effective in relieving symptoms. Surgery may be considered in patients with refractory disease.(18)
PROSTATITIS
Prostatitis is a condition that is characterised by inflammation of the prostate gland. Prostatitis can develop in men of all ages, but it is more common in men aged over 50. Symptoms of prostatitis can include
pain on urination, pain on ejaculation, difficulty passing urine, groin pain, fever, and tiredness.(20) Prostatitis can present as acute or chronic. Diagnosis can be difficult as there is no diagnostic laboratory test, but clinical diagnosis depends on patient history and physical examination. There is limited understanding of pathophysiological, therefore treatment is difficult, and patients may remain symptomatic for the long term.(17)
Prostatitis is often caused by bacterial infection and can often be treated with oral antibiotic according to sensitivities – with quinolones such as ciprofloxacin a common treatment option, or trimethoprim if
the patient is allergic to quinolones. Non-steroidal anti-inflammatory drugs (NSAIDs) can be used for pain relief.
Alpha blockers such as doxazosin, alfuzosin, tamsulosin, and silodosin used in combination with an analgesic and a benzodiazepine as a muscle relaxant is the most common treatment option.(17)
PROSTATE CANCER
Prostate cancer is the most diagnosed male malignancy and the fifth leading cause of cancer death in men. The significant risk factors for prostate cancer are increasing age, genetics, obesity, and ethnicity. The incidence of prostate cancer increases as people get older, but aggressiveness decreases with age. The overall five-year survival rate is estimated to be 99%. Symptoms can be very similar to those of BPH and prostatitis and can include frequent urination, nocturia, difficulty starting and maintaining a steady stream, dysuria, painful ejaculation, and erectile dysfunction. Early prostate cancer is generally asymptomatic and is therefore sometimes only diagnosed during screening programmes.(21)(22)
An elevated PSA level (greater than 4 ng/ml) is how many prostate cancers initially present. A DRE can be used to help in the diagnosis of prostate cancer, with tumours feeling stiff and irregularly shaped. Ultrasound and MRI (magnetic resonance imaging) are imaging techniques that are useful in detecting and diagnosing prostate cancer. Biopsy of the prostate is a definite method in diagnosing, where a sample is examined under a microscope.(21)
Active surveillance is an option for low- risk and older patients, where the disease is regularly monitored without invasive treatment. It is useful in the early stages and where the risks of treatment outweigh the benefits. Sometimes treatment is necessary if there are signs of tumour progression. Radiation therapy is a good treatment option for localised disease, with good survival rates and fewer side effects. Prostatectomy is another treatment option, with potential side effects including ED, urinary incontinence, urethral strictures, and inguinal hernias. Hormonal therapy is an effective treatment option and can be used in combination with other treatment option. Luteinising hormone- releasing hormone (LHRH) agonists such as goserelin and leuprorelin can be effective when PSA level is greater than 10 ng/ml, when combined with anti-androgen therapy, such as bicalutamide. Potential side effects of hormonal therapy include hot flushes, reduced libido, and reduced bone density.(21)
CONCLUSION
Men can be affected by several important conditions throughout their life. In general, men have worse health outcomes and a lower life expectancy than women. Men often ignore symptoms which can lead to late diagnosis and poorer health outcomes. A greater emphasises should be put on the promotion of men’s health and creating greater awareness of these conditions. Men should be encouraged to be actively involved with their health and seek help from a healthcare professional if they have any symptoms, in addition to regular check-ups. ?
References upon request
Disclaimer: Brands mentioned in this article are meant as example only and not meant as preference to other brands.