There can be some confusion about different terms relating to babies and the interchangeability of these terms. A neonate, or newborn infant, is a child under 28 days, an infant is up to 12 months old, and a toddler is older than 12 months. Infancy is a time of rapid growth and development of the body, second only to the foetal period. It is an important time for both physical and cognitive development. Proper nutrition is required to ensure adequate growth and development of organs, while social interactions are important for brain development.
Many infectious diseases are much more common in infants than any other age group. These infectious diseases are associated with morbidity and sometimes mortality in infants. These infections can be due to the infant’s environment, their lack of immune development, or epidemic.
There are a wide range of illnesses and conditions that are commonly contracted by infants. Most conditions are self-limiting and resolve within one or two weeks. However, they can still cause stress and worry to the parents or guardians of the infant. Parents or guardians are urged to trust their intuition and contact a doctor if they are worried. Urgent medical care should be sought if the infant is unresponsive, has difficulty breathing, has blue lips/tongue, is having seizures, or has a rash that doesn’t fade when it is pressed. The carer should also seek medical attention with symptoms such as coughing, diarrhoea, vomiting, fever, sweating during feedings, and sleeping more than usual. In Ireland, an infant can visit the general practitioner (GP) at two weeks and six weeks of age to ensure normal growth and development. Regular check-ups with the GP and following the childhood immunisation schedule is also vitally important for the child’s health.
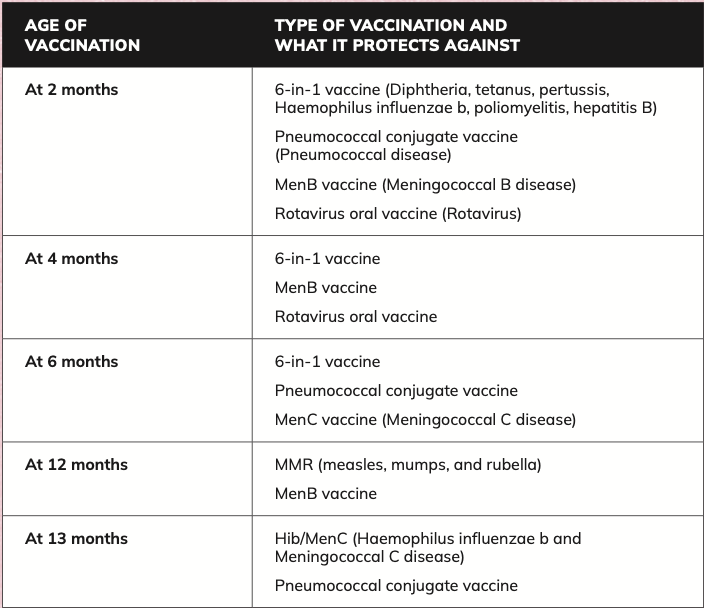
Vaccinations
Vaccinations are given during infancy due to the vulnerability of infants to a wide range of infectious diseases. Infants are at the highest risk of complications due to many diseases and therefore require protection. Routine childhood immunisation has yielded major reductions in the incidence of many infectious diseases. This has dramatically reduced morbidity, disability, and mortality caused by preventable diseases. Maintaining and improving vaccine coverage are required to continue low incidence levels of these diseases. In Ireland, there is a childhood immunisation schedule, with vaccinations given at five different stages in the first 13 months of life.
All vaccinations are free of charge from the infant’s GP. These vaccinations are outlined in Table 1.
Infection
Infectious diseases can occur at any age but can be a particular cause of concern in infants due to their immune systems not being fully developed. Some antibodies can pass from the mother to foetus, but antibody levels may not be sufficient to fight infection. Infections can be viral, fungal, or bacterial.
In Ireland, an infant can visit the GP at two weeks and six weeks of age to ensure normal growth and development. Regular check-ups with the GP and following the childhood immunisation schedule are also vitally important for a child’s health
Viral infections
Viral infections can present in a variety of ways in infants. Many viral infections have clinical presentations specific to the infecting virus but can also present differently, based on the age and immunocompetence of the patient. Most viral infections in infants are self-limiting and symptoms can be treated until the infant makes a full recovery. However, some viral infections can be much more serious.
Respiratory infections are normal in infants due to the large number of respiratory viruses in circulation and the infant’s lack of immunity, with eight or more colds per year normal for an infant. As a child gets older, they generally build up immunity gradually and get fewer respiratory infections. Common symptoms of respiratory viruses include sore throat, blocked/runny nose, sneezing, feeling unwell, fever, and cough. Croup is an inflammation of the airways that is caused by a viral infection of the larynx and trachea. Symptoms usually develop over a few days and can be worse at night. Symptoms can include a rasping barking cough, difficulty breathing, hoarseness, and fever. Most respiratory viruses are self-limiting and can be treated at home. Paracetamol and ibuprofen can be used to relieve pain and reduce fever. Ensuring adequate hydration is also important, while vitamin D supplementation can reduce the risk of respiratory viruses.
Respiratory syncytial virus (RSV) is a common respiratory virus that spreads in winter and early spring and is the primary cause of bronchiolitis and pneumonia in infants. Most symptoms are mild respiratory symptoms, with patients recovering within two weeks, without the need for further treatment. There is no specific anti-viral treatment for RSV in Ireland. RSV can sometimes be serious and if the following warning symptoms are observed, medical attention should be sought:
- Difficulty breathing;
- Blue lips or tongue;
- Long gaps in breathing;
- Rapid breathing.
Hand, foot, and mouth disease is a common illness in infants that is caused by a viral infection. Initial symptoms are a sore throat, fever, and unwillingness to take feeds. Mouth ulcers and rash on the hands and feet usually appear after a few days. Hand, foot, and mouth disease is usually self-limiting and symptoms can be treated with paracetamol and ibuprofen, with adequate hydration essential as dehydration is one of the main complications of this illness.
Fungal infections
Fungal infections in infants are often caused by the Candida species and can lead to conditions such as nappy rash and oral thrush. Ensuring proper cleaning and drying of the nappy area can reduce the risk of nappy rash, while using a protective barrier cream or topical antifungal can be used to treat nappy rash. Oral thrush is a common fungal infection in infants. Symptoms of oral thrush include white spots in the infant’s mouth, a white coating on the tongue and not wanting to feed. Oral miconazole gel can be used to treat oral thrush in infants four months and older.
Pharmacists have the drug knowledge and communication skills to play an important role in infant care. They are often the most accessible healthcare professional in the community and therefore they are often the first point of access in the primary care system
Bacterial infections
Bacterial infections can cause a wide range of illnesses in infants, from mild self-limiting ones to more severe, life-threatening illnesses. Each bacterial infection can have its own specific clinical presentation and complications, which necessitate a specific treatment approach.
Urinary tract infections (UTIs) in infants are as a result of bacterial colonisation in the urinary tract, often due to improper hygiene. Symptoms of a UTI include pain on urination, cloudy or foul-smelling urine, fever,
and irritability. Antibiotic therapy should be tailored to the specific bacteria identified during urine culture and sensitivity testing, and may include amoxicillin, cefalexin, trimethoprim, or nitrofurantoin.
Impetigo and cellulitis are common bacterial skin infections that are sometimes due to a break in the skin barrier or an open wound. Impetigo is highly contagious but is generally self-limiting and will clear within a couple of weeks. If treatment is necessary, topical or systemic antibiotics are effective. Fusidic acid can be applied topically, while flucloxacillin and cefalexin are commonly used systemic antibiotics to treat skin infections.
Respiratory bacterial infections are common in infants and are characterised by a cough, difficulty breathing, rapid breathing, and fever. A wide range of pathogens can cause respiratory infections and pneumonia is a common illness. Treatment of the respiratory infection depends on the specific pathogen involved, with amoxicillin and azithromycin commonly used antibiotics.
Meningitis is a serious illness characterised by inflammation of the meninges that surround the brain and spinal cord. Meningitis can be either viral or bacterial. Viral meningitis is usually not as dangerous as bacterial meningitis, and most people make a full recovery within 14 days. Bacterial meningitis is more severe and can be life-threatening, requiring immediate medical attention. Symptoms of meningitis are wide-ranging and include a rash that doesn’t fade when a glass is pressed against it, fever, neck stiffness, headache, body aches, sensitivity to light, seizures, confusion, and irritability. Prompt diagnosis with a lumbar puncture and intravenous antibiotic therapy is required for treatment of bacterial meningitis.
Pain
Pain is often an underdiagnosed and undertreated medical issue in the infant population, with up to 40 per cent of children complaining of pain at least once per week. A proper pain assessment tool is needed to establish the nature and severity of the pain in order to implement an optimal pain management approach tailored to the infant. Paracetamol and ibuprofen are effective treatment options available over-the-counter for mild-to-moderate pain. The recommended dosage for paracetamol is 15mg/kg per dose every four to six hours, with a maximum of 1g per dose and 4g per day. Ibuprofen is recommended at a maximum of 10mg/kg per dose every six to eight hours. Paracetamol has a favourable adverse effect profile when administered correctly, while adverse effects of ibuprofen and other non-steroidal anti-inflammatory drugs (NSAIDs) include nausea, vomiting, gastrointestinal bleeding, and diarrhoea. Opioids can be used to treat moderate-to-severe pain but should be used with caution, with appropriate dosing and close monitoring due to several potential adverse effects. Some of the warning symptoms that may accompany pain and that will require referral include convulsions, less responsive than usual, severe pain, unusual rash, blood in the urine or stool, and breathing difficulties.
Colic and reflux
Colic is a common condition that affects up to 20 per cent of babies and presents as excessive and frequent crying in babies that appear otherwise healthy. A baby has colic if they cry for more than three hours per day for more than three days per week for more than three weeks. Other symptoms can include clenching of fists, restlessness, and going red in the face. It usually starts when a baby is two weeks and resolves by four months old. The aetiology of colic is unknown. Potential causes of colic include alterations in faecal microflora, intolerance to cow’s milk, gastrointestinal inflammation, poor feeding technique, and maternal smoking. Colic can be very upsetting and difficult for parents of infants. There is no specific pharmacological treatment for colic, however different methods may help provide relief.
Gastroesophageal reflux is the passage of stomach contents into the oesophagus with or without accompanied regurgitation and vomiting. It is a common condition in infants and can affect up to 40 per cent of babies. Reflux usually improves and resolves before the infant is 12 months old, without need for pharmacological treatment. Diagnostic tests are not usually performed, unless there are atypical symptoms, warning signs, or suspected complications. Reflux in infants can be treated with several non-pharmacological methods that are outlined below. Proton pump inhibitors and histamine receptor antagonists are effective in treating reflux and can be used if non-pharmacological treatment methods fail.
Both colic and reflux can be helped by several different methods including:
- Holding or rocking the baby;
- Avoid overstimulating the baby;
- Sitting the baby upright during feeds;
- ‘Wind’ the baby after feeds;
- Minimising the amount of air in the bottle during feeds;
- Using lower volume feeds;
- Ensure the baby sleeps flat on their back.
Parents should bring their infant to the GP if any of the following warning symptoms are present:
- Has difficulty feeding or refuses feeds;
- Vomiting bile;
- Has blood in the mucus;
- Losing weight or not gaining weight;
- Parent is struggling to cope;
- Coughing or gagging during feeds.
Infant nutrition
Nutrition is vital in supporting healthy growth and development during infancy. Pharmacists can offer guidance on many aspects of infant nutrition including breastfeeding, formula feeding, and the introduction of solid foods. Breastfeeding offers many benefits to both mother and infant including providing excellent nutrition, improving immunity, and helping develop a bond between mother and child. Pharmacists can provide support on proper latch techniques, nipple care, and addressing issues such as milk supply and mastitis. Selecting an appropriate formula based on the infant’s age and nutritional needs is important to support growth and development in infants. Finally, as infants start to transition to solid food, pharmacists can offer advice on appropriate foods and how to address concerns such as food intolerance, colic, reflux, flatulence, and constipation.
Role of pharmacist
Pharmacists have the drug knowledge and communication skills to play an important role in infant care. They are often the most accessible healthcare professional in the community and therefore they are often the first point of access in the primary care system. Parents often present at a community pharmacy with a child with symptoms. Pharmacists can assess the patient and treat them with over-the-counter medication if appropriate. They can also reassure and relieve some of the stress that parents may have. Furthermore, they can recognise warning signs in infants and refer them onto another healthcare practitioner if necessary. Breastfeeding offers a wide range of benefits for both mother and infant. Transfer of medication into breast milk can occur but most medications are safe to use during breastfeeding. Pharmacists, as medication experts, can offer their expertise to breastfeeding mothers. Pharmacists have a multifaceted role in guiding parents and infants through the early stage in an infant’s development.
References upon request