Donna Cosgrove MPSI discusses the ins and outs of folic acid and folate
The terms ‘folic acid’ and ‘folate’ are often used interchangeably, but there are important structural differences that lead to their differences in bioavailability. Folic acid (pteroylmonoglutamic acid, vitamin B9) is synthetic, and folate occurs naturally in human, animal and plant tissues.(1) Folic acid and folate are used in.(2) ?Folate deficiency anaemia;
- Helping the development of unborn babies’ brain, skull and spinal cord, reducing the risk of spina bifida;
- Helping to reduce side effects from methotrexate.
- Folic acid, which has much better bioavailability than food folate, is absorbed very quickly in the gut once taken. Folates are found in green leafy vegetables, asparagus, beans, legumes, liver and yeast, although it can be difficult to absorb adequate amounts of folic acid from diet alone due to much of it being lost in food processing and cooking.(2,3)
Folates function as cofactors in pathways required for DNA and RNA synthesis, serine and glycine metabolism, histidine catabolism, methionine synthesis, and methylation processes. They interact closely with other B vitamins B12, B6 and riboflavin. Severe folate (or also B12) deficiency leads to megaloblastic anaemia, manifesting as fatigue, weakness, and shortness of breath due to low levels of erythrocytes. Deficiency usually occurs as a result of increased demands, e.g. in pregnancy, and when folate availability is reduced due to low dietary intake or
malabsorption, which occurs in e.g. coeliac disease. In all individuals, the absence of anaemia does not indicate sufficient folate status: there is strong evidence emerging that shows folate has multiple roles in maintaining health. Suboptimal folate levels are linked with adverse outcomes throughout the lifespan.(1)
FOLIC ACID IN PREGNANCY
More than 30 years ago a landmark study (4) was published showing definitively that folic acid supplementation in mothers protects against neural tube defects (NTD), resulting in the recommendation to take this pre and during early pregnancy. Ideally women should take a folic acid supplement for at least 14 weeks before conceiving, and continue for at least the first 12 weeks of pregnancy. It is recommended that all women of childbearing age should take a 400mcg folic acid supplement every day, even if they are not planning to conceive.(2)
In pregnancy, increased folate is needed to sustain the growth of maternal, foetal, and placental tissue. Supplementation in early pregnancy when this is required prevents this decline, and also prevents megaloblastic anaemia of pregnancy. Low folate concentrations in the body at the time of conception are associated with neural tube defects, which often lead to significant disability or death for affected unborn babies and children.(5)
ADDITIONAL BENEFITS OF FOLIC ACID
In addition to preventing NTD, evidence shows that folic acid supplementation around pregnancy may help prevent congenital heart defects in infants, and possibly orofacial clefts. Insufficient folate or elevated homocysteine (an indicator of folate deficiency) levels are also linked to some adverse pregnancy outcomes for the mother, including gestational hypertension, preeclampsia, placental abruption, pregnancy loss, low birth weight and intrauterine growth restriction. Emerging evidence suggests a link between improved scores on cognitive tests and improved language processing in children of mothers who took folic acid compared to children of those who did not.
An association between low folate, B12 and B6 with an increase in cardiovascular disease and stroke risk has been observed in adults. There is also evidence that folate and B vitamins are important to maintain cognitive health in ageing and have been linked with dementia risk. Observational studies have identified a reduced risk of depression in older Irish adults who consumed fortified foods on a daily basis compared to non-consumers.(1)
NEURAL TUBE DEFECTS
On average, at least 214,000-322,000 pregnancies are affected annually worldwide by spina bifida (a spinal cord defect) and anencephaly (a brain defect). The most common known cause of spina bifida is insufficient folate concentration in the mother before and during the first three months of pregnancy. Individuals with spina bifida can be permanently disabled and have chronic physical and psychological health complications.(1,3)
Spina bifida means ‘split spine’. In Ireland, one in every 1,000 children born each year are affected, which is one of the highest incidences in the world. It is the most common NTD, which causes incomplete development of the spinal cord.(6) There are three types (Table 1).
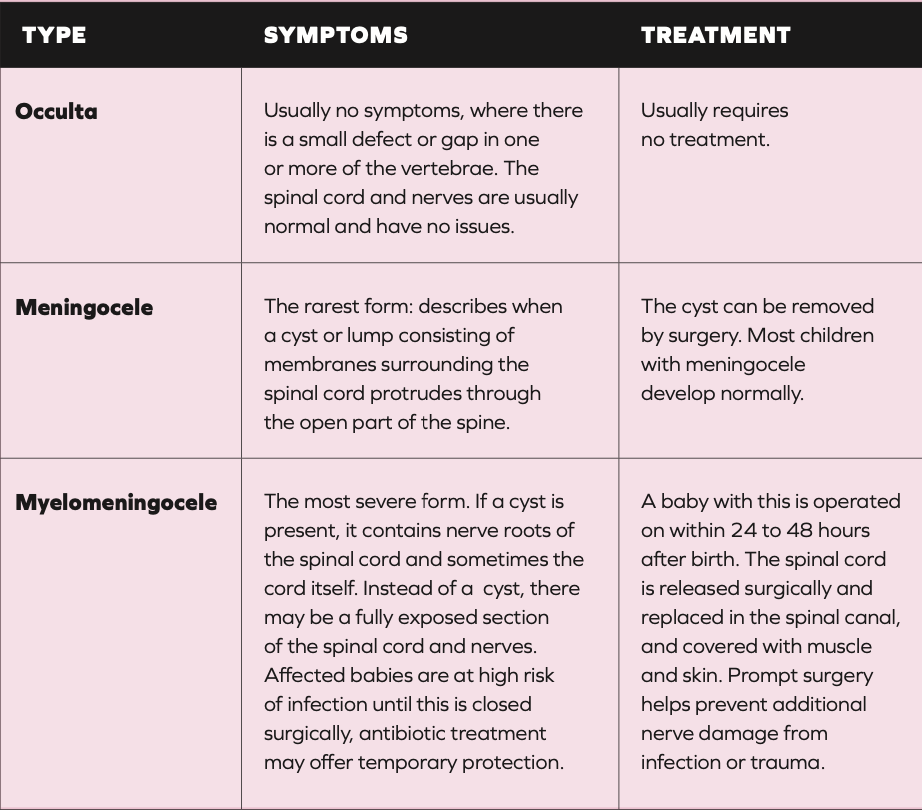
TABLE 1: Types of spina bifida(5)
Although genetic, nutritional and environmental factors are all thought to contribute to the development of spina bifida, more than 95% of parents of diagnosed children do not have any family history, although the risk of recurrence in any subsequent pregnancy is about one in 40.(6)
If there was a previous pregnancy affected by NTD, the recommended dose is 4-5mg daily. Unless this is the case, no more than 1mg folic acid per day to avoid the possible risks of excessive intakes. Although there is evidence to support 4mg per day in those who had a previous pregnancy affected by NTD, there is no evidence to support this level of supplementation in women with diabetes or obesity, as recommended by some clinical guidelines.
Despite active health promotion campaigns over many years, folic acid supplementation has had little or no impact in preventing NTD at a population level, primarily because women who have unplanned pregnancies only start taking folic acid after the period of neural tube closure. The neural tube normally closes within the first 28 days after conception.(1)
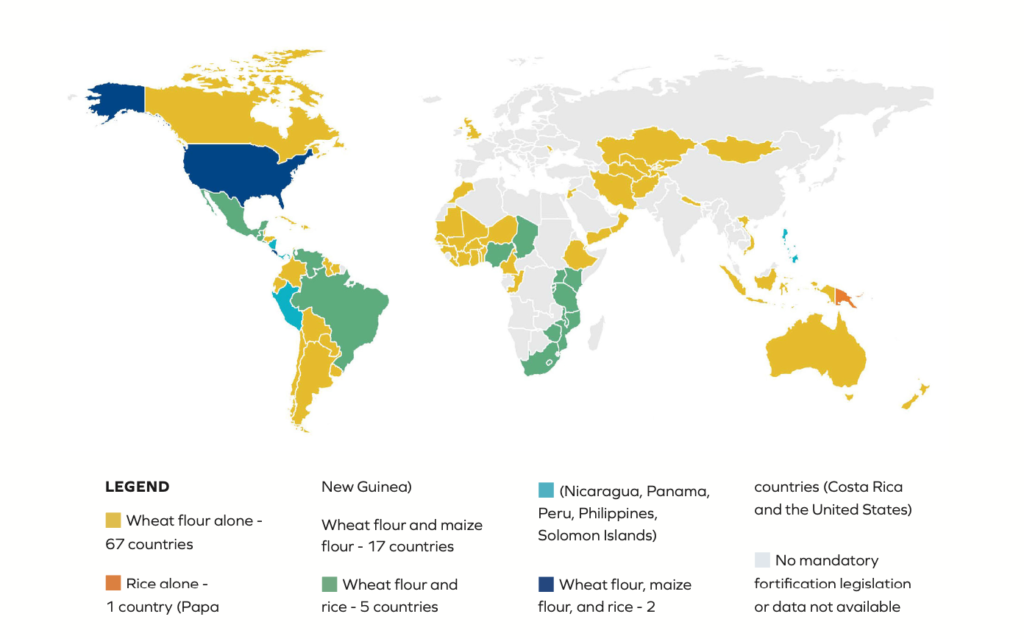
FIGURE 1: Countries in which food fortification with folic acid is mandatory, and the fortified items(7)
FOOD FORTIFICATION WITH FOLIC ACID
Fortification increases folate levels in women, leading to a reduction of spinal bifida and anencephaly. This also has economic benefits to the state, and allows conservation of medical resources that are otherwise dedicated to diagnosis and care of affected babies and individuals.(3) In the USA, the prevalence of low folate status in young women has reduced from between 21 and 30% to between 0.8 and 2.8% since mandatory folic acid food fortification was introduced. In Ireland, there is concern that the incidence of NTD is increasing in recent years, possibly related to a decline in folic acid fortified products. Voluntary fortification of food with folic acid and other micronutrients is permitted in Ireland, but not mandated.(1)
Although mandatory food fortification with folic acid is a very effective public health strategy to reduce folate insufficiency, only about 90 countries in the world implement this (Figure 1).
No country in Europe has implemented this fortification, meaning preventable NTDs are not being prevented. The advantage of mandatory food fortification is that it reaches all women including those who have not planned their pregnancy.(1,3)
CONCERNS ABOUT FOOD FORTIFICATION WITH FOLIC ACID
In many countries, including the UK and Ireland, folic acid food fortification has been delayed due to concerns relating to potential adverse effects. It was thought that folic acid may mask anaemia due to vitamin B12 deficiency. Adding vitamin B12 along with folic acid to food has been suggested as a solution to this, but more information on efficacy, dosage and feasibility is required.(1,3) Folate and B12 deficiency both cause megaloblastic anaemia. Very high amounts of folic acid can correct the anaemia associated with B12 deficiency, hiding the deficiency, but allowing the other problem of B12 deficiency (neurological disease) to continue.(8)
In the USA, where food fortification with folic acid has been a policy for more than 25 years, this has not shown up as an issue – the incremental intake in folic acid from food fortification is likely too small to cause masking.(9)
Another concern, which has still not been substantiated, is the idea that due to folic acid’s role in DNA synthesis, high intakes could increase malignant transformation of premalignant lesions. Evidence has shown that there are not likely to be adverse events linked to folic acid levels arising from mandatory food fortification, and the proven benefits outweigh any potential risks. However, vigilance in public health is still of ongoing importance in relation to any food fortification strategy.(1)
A report published in 2016(10) by the Food Safety Authority of Ireland recommended mandatory fortification
of bread or starch. Results of a public consultation were discussed in a previous report,(9) highlighting the support in this country for mandatory folic acid fortification of bread or flour by more than three-quarters (77.1%) of the submissions made. In addition, all relevant industry sectors (flour millers, improver/flavouring ingredient suppliers and large bread manufacturers) are willing to participate in a national folic acid food fortification programme.
The report summary estimates that a national policy of mandatory fortification of bread with folic acid would reduce the incidence of NTD- affected pregnancies by about 24%. In addition, it would lead to other health benefits associated with reducing folate deficiency. In 2021, Britain announced a plan for mandatory folic acid food fortification. With compelling results from 25 years of fortification helping to reduce concerns about possible harms, the UK may be the first of many countries in Europe to make this move.
REFERENCES
1. McNulty, H., Ward, M., Caffrey, A., & Pentieva, K. (2023). Contribution of folic acid to human health and challenges of translating the science into effective policy: a call to action for the implementation of food fortification in Ireland. Proceedings of the Nutrition Society, 82(2), 91-103.
2. Health Service Executive. (2021). Folic Acid. Available https://www2.hse. ie/conditions/folic-acid/#:~:text=If%20 you’re%20pregnant%20or,not%20 planning%20to%20get%20pregnant. 3. Kancherla, V., Botto, L. D., Rowe,
L. A., Shlobin, N. A., Caceres, A., Arynchyna-Smith, A., … & Berry, R. J. (2022). Preventing birth defects, saving lives, and promoting health equity: an urgent call to action for universal mandatory food fortification with folic acid. The Lancet Global Health, 10(7), e1053-e1057.
4. MRC Vitamin Study Research Group. (1991). Prevention of neural tube defects: results of the Medical Research Council Vitamin Study. The lancet, 338(8760), 131-137.
5. Mid West Spina Bifida and Hydrocephalus Association. (2020). Spina Bifida. Available https://www.spinabifida.ie/spina- bifida/#:~:text=Spina%20Bifida%20 literally%20means%20’split%20 spine’&text=Ireland%20has%20one%20 of%20the,development%20of%20 the%20spinal%20cord.
6. Viswanathan, M., Urrutia, R. P., Hudson, K. N., Middleton, J. C., & Kahwati, L. C. (2023). Folic acid supplementation to prevent neural tube defects: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA, 330(5), 460-466.
7. Food Fortification Initiative. (2022). 2022 Annual Report. Available https://static1.squarespace.com/ static/5e1df234eef02705f5446453/ t/6479fc300d14487cc 6b03587/1685716024333/FFI_ AnnualReport_2022.pdf
8. Food Safety Authority of Ireland. (2006). Report of the National Committee on Folic Acid Food Fortification. Available https://www. lenus.ie/handle/10147/44809
9. Mills, J. L., Molloy, A. M., & Reynolds, E. H. (2018). Do the benefits of folic acid fortification outweigh the risk of masking vitamin B12 deficiency?. BMJ, 360. 10. Food Safety Authority of Ireland. (2016). Update Report on Folic Acid and the Prevention of Birth Defects in Ireland. Available https://www. fsai.ie/getmedia/2b1deb65-0bc9- 416a-b0db-7cf46355db2f/folic-acid- report-2016.pdf?ext=.pdf







