There are many minor eye conditions that are associated with the changing winter weather, such as dry eye. However, one condition that can also cause eye problems is Sjögren’s syndrome, an under-diagnosed autoimmune condition that can have a serious impact on quality of life.
People aged 60 years and older are particularly susceptible to eye problems and the pharmacist is in the best possible position to advise these patients. The Irish College of Ophthalmologists recommends lifestyle interventions to preserve eye health, including dietary advice. Foods high in antioxidants can help to prevent retinal damage, and certain eye conditions like cataracts and agerelated macular degeneration (AMD).
The harsh winter weather influences eye health due to factors such as increased heat indoors, as well as spending a lot of time outdoors in harsher weather conditions. Switching from cold weather to dry, heated indoor air can also have a detrimental effect on eyes and can easily dry them out.
Diet is also an important factor and an antioxidant which hugely beneficial is lutein, which is found in many fruit
and vegetables.1
Foods recommended for eye health that contain the antioxidant lutein include:
- Broad leaf greens, such as kale and spinach.
- Brightly-coloured fruit and vegetables, such as corn, carrots, orange sweet peppers and oranges.
- Oily fish like salmon, tuna and mackerel.
- Broccoli.
- Eggs.
However, if a patient is suffering from dry eyes, dry mouth or dry skin and the cause has not been diagnosed, Sjögren’s syndrome is a potential reason. Sjögren’s syndrome remains undiagnosed in many people. It is an autoimmune condition, meaning white blood cells attack other cells in the body. The cause is unknown. It
was first discovered by Swedish ophthalmologist Henrik Sjögren in the 1930s and ‘Sjögren’ is pronounced ‘Show-gren’. In Sjögren’s syndrome, the body’s white blood cells attack other cells in the body.
Research has resulted in the identification of a number of factors (ie, immunological, genetic, hormonal, and inflammatory) that may be involved in causing the condition. One theory being postulated is that inflammation or abnormality of the body’s glands causes an autoimmune reaction.2

The main and most obvious symptoms of Sjögren’s syndrome are dry eyes and dry mouth, as well as enlargement of the parotid glands (salivary gland located in the cheeks just in front of the ears). Dry eyes and mouth
occur in 95 per cent of cases.3 The hallmarks of Sjögren’s syndrome (ie, dry mouth and dry eyes) is known as sicca
syndrome. Fatigue and joint and muscle pains are other debilitating features in many who have the condition.
For some people, the symptoms are no more than a nuisance. However, for others, they are more severe and have a profound effect on their quality of life if not treated adequately. Whilst dry eyes and dry mouth are common features of Sjögren’s syndrome, most people who develop these symptoms do not have the disease; for example, dry eyes and dry mouth have been found to affect about 30 per cent of older people overall, and the majority of these cases are not due to Sjögren’s syndrome itself. Dry mouth and eyes can also be caused by many medicines, such as tricyclic antidepressants, antihistamines, decongestants, beta blockers (for blood pressure and heart conditions), codeine-type painkillers, diuretics, etc.
Therefore, before a patient is diagnosed, it must be checked that they are not taking one of these medicines that could be causing the dry eyes and mouth. Dry eyes lead to itchy eyes, grittiness and soreness, and can lead to damage to the cornea if not controlled. Dry mouth may not be immediately obvious on presentation, and the person may not complain of dryness, but they may describe experiencing an unpleasant taste, insatiable thirst, difficulty eating dry food such as cream crackers, and soreness/discomfort.
In itself, dry mouth is not normally a serious problem, but if not addressed it can lead to:
- Loss of taste.
- Thrush (fungal infection) in the mouth.
- Tooth decay and gum disease.
- Swallowing problems and dysphagia (the feeling of something getting stuck in the throat on swallowing).
- Sore or cracked tongue.
- Difficulty talking.
According to the Mayo Clinic, other complications of Sjögren’s syndrome can include:4
Most common complications involvinf eyes and mouth:
Yeast infections. People with Sjogren’ssyndrome are much more likely to develop oral thrush, a yeast infection in the mouth.
- Dental cavities. Because saliva helps protect the teeth from the bacteria that cause cavities, people are more prone to developing cavities if their mouth is dry.
- Vision problems. Dry eyes can lead to light sensitivity, blurred vision and corneal damage.
Less common complications
May include:
- Lymph node cancer. A small percentage of people with Sjogren’s syndrome develop cancer of the lymph nodes (lymphoma).
- Lungs, kidneys or liver. Inflammation can cause pneumonia, bronchitis or other problems in the lungs, lead to problems with kidney function, and cause hepatitis or cirrhosis in the liver.
- Nerves. There may be numbness, tingling and burning in the hands and feet (peripheral neuropathy).
Typical effects of Sjogren’s syndrome are illustrated in Figure 1. Other symptoms of Sjögren’s syndrome can include dryness of the airways (which can lead to dry cough and chest infections) and glandular swelling. Swelling of the parotid glands occurs in approximately one-third of cases and can be painful in some cases6 and swelling of other salivary glands located under the jaw or in the neck area can also be a problem. Muscle ache and aching joints can occur, and joint ache typically occurs in onethird of cases.6 Raynaud’s phenomenon —coldness in the extremities of the body, such as in the hands and fingers — occurs in about 20 per cent of cases of Sjögren’s syndrome.
As stated above, Sjögren’s syndrome can also cause peripheral neuropathy in about a quarter of cases. Peripheral neuropathy is damage to the nerve endings in the extremities such as fingers and toes and can cause numbness, tingling, itching, pins and needles, as well as other manifestations.7
Sjögren’s syndrome is referred to as ‘primary’ if it develops in isolation, and ‘secondary’ if it occurs in combination with other autoimmune or rheumatic conditions such as fibromyalgia, systemic sclerosis, rheumatoid arthritis, or systemic lupus erythematosus. It is estimated that in 60 per cent of cases, Sjögren’s syndrome occurs with or is linked to other inflammatory autoimmune conditions.
Rheumatoid arthritis, for example, is a severe inflammatory condition that causes swelling, pain, and deformities in the joints and it tends to run in families. Systemic lupus erythematosus (otherwise known as lupus) is nine times more common in women. Lupus can cause inflammation in all organs, leading to joint pain, muscle pain, fever, fatigue and damage to all major organs if not controlled. Lupus is more rare in Europe and more common in people of Afro-Caribbean decent.
Fibromyalgia is a chronic pain disorder characterised by extreme tiredness and fatigue, while scleroderma is an inflammatory condition that affects the skin, leadingto hard skin and skin lesions, and can go on to damage other organs if not controlled. Counselling patients with Sjögren’s syndrome is important to help them manage their own care, and there are a number of steps these patients can be advised to take to reduce the severity of their symptoms. These include:8
For joint pain:
- Be more active, especially between flare-ups.
- Rest when joints are swollen and painful. Rest instead of trying to fight the fatigue during flare-ups. For dry nose, throat and upper airways:
- ? Regularly use saline nasal sprays.
- ? A home humidifier may help.
For dry eyes:
- Use lubricating eye ointments or gels at night.
- ? Wraparound sunglasses can prevent moisture loss from the eyes.
- ? Regularly use tear substitute eye drops, with single-dose preservative-free drops possibly showing more benefit.
- ? Limit use of drops with preservatives, which can cause dryness and irritation.
Dry mouth and other dental/ oral issues:
- Chewing sugar-free gum or sucking sugarfree hard sweets or lozenges stimulates saliva.
- Regularly take small sips of water.
- Avoid sugar-containing foods and drinks between meals.
- Use an electric toothbrush.
- Using products with artificial sweetener xylitol rather than sugar prevents tooth decay.
- Get regular dental check-ups.
- Use fluoride products specifically for dry mouth.
- Brush and floss teeth regularly (after meals especially). If regular day-time brushing is not possible, rinse regularly with water.
- Use artificial saliva in the form of mouth gels, mouthwashes and chewing gum.
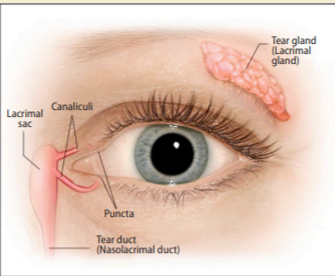
Image courtesy of Mayo Foundation for
Medical Education and Research
To relieve dry eyes, artificial tears have proven effective and should be used regularly by the patient. They come in drop form and gel form (the gel form has a longer-lasting effect, so is especially suitable before going to bed). There are many brands available over the counter from pharmacies; there is no evidence that one brand is any more effective than the next, though preservativefree versions are recommended by some eye specialists to reduce the risk of a preservative causing irritation.
The tear film contains three layers — fatty oils, aqueous fluid, and mucus — and this combination normally keeps the surface of the eyes lubricated, smooth and clear. However, problems with any of these layers can cause dry eyes. The basic physiology of the tear ducts is illustrated in Figure 2. There is no approved cure for Sjögren’s syndrome, so therefore the goal of any treatment methodology is to control symptoms using therapies, and to limit longterm damage. The patient must be referred to a rheumatologist for assessment and diagnosis, and an ophthalmologist is often involved in the treatment of the eye problems if they are severe enough. Smoking and drinking alcohol should be avoided and good oral hygiene should be maintained. Exercising as much as possible and a healthy balanced diet are also important. Vaginal lubricants may be required to tackle certain symptoms and it should be noted that candidiasis (thrush) is more likely with Sjögren’s syndrome due to vaginal dryness.
Dews II
Pharmacists should be aware of the TFOS DEWS II Definition and Classification system, which contains an evidence-based definition and a contemporary classification system for dry eye disease (DED). The algorithm provides detailed information on the management and therapy options for DED, including tear insufficiency, anti-inflammatory therapies, managament of the psychological aspects of DED, and a wide range of other important treatment considerations.
Full details can be accessed at https://www.tfosdewsreport.org/report-management_and_therapy/147_36/en/.
Over the counter
Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, can be prescribed over the counter to relieve muscle and joint pain. However, these should be used in moderation, as they can cause side-effects such as stomach irritation and ulcer, raised blood pressure and kidney problems. They should also be used in caution with other conditions such as asthma, heart disease and kidney disease. Mild corticosteroid cream such as hydrocortisone 1% cream — used sparingly and occasionally — may give some relief from the dry skin symptoms (although regular moisturisation is key to advised and prevent dry skin).
To relieve dry mouth, drinking plenty of fluids helps keep the mouth moist. Artificial saliva can also be prescribed over the counter and comes in the form of mouth gels, mouthwashes and chewing gum. Some brands available over the counter in pharmacies include BioXtra and Biotene. As well as moisturising, these therapies have enzymes that help stimulate the saliva glands. Another option for dry mouth is pilocarpine tablets and these are licensed for those who have some residual salivary function left.9
The dose is 5mg tablets to be taken four times daily, before each meal and at night.
Medications
As stated above, Sjögren’s syndrome may
progress to involve organs such as the kidneys, lungs, skin and lymph glands and
anti-inflammatory medication may be required in these situations.
Options include:
Careful monitoring with regular blood tests is required while taking immunosuppressants, as they can cause blood disorders and can affect the immune system. These drugs suppress the abnormal antibody production that causes Sjögren’s syndrome, ie, they prevent the body ‘attacking itself’. Examples include methotrexate, azathioprine, penicillamine and hydroxychloroquine. They are reserved for more severe cases, as they can have side-effects and are only commenced by specialist rheumatologists. It is recommended that use of immunosuppressive agents is limited to cases where Sjögren’s syndrome is affecting the major organs such as skin, lungs and kidneys.10
Steroids:
These tablets are taken orally and reduce inflammation. They are usually limited to when symptoms are particularly troublesome, as they can cause side-effects if used long-term.
Methotrexate is often the first-choice DMARD for rheumatoid arthritis (RA), but less so in Sjögren’s syndrome. It can be taken on its own or in combination with another DMARD. The most common sideeffects associated with methotrexate are sickness, mouth ulcers, diarrhoea, hair loss or hair thinning, and rashes on the skin. Regular blood tests to monitor blood count and liver are required, as methotrexate can cause potentially serious liver and
blood count problems.
Very rarely, it can affect the lungs, so chest x-rays and possibly breathing tests are performed when starting methotrexate. This is to provide a comparison for if the patient develops shortness of breath or a persistent dry cough while taking methotrexate. Most people tolerate methotrexate well and more than 50 per cent of patients take it for at least five years.
Sulfasalazine has a slow onset of effect (one-to-three months).11 Patients may need to discontinue long-term treatment of sulfasalazine due to gastrointestinal complaints. DMARDs help to ease symptoms and slow down the progression of inflammatory conditions. When antibodies attack the tissue in the joints, they produce chemicals that can cause further damage to the bones, tendons, ligaments, and cartilage and in the case of Sjögren’s syndrome, they affect the eyes and salivary glands. DMARDs block the effects of these chemicals. The earlier a DMARD is started, the more effective it will be but they must be started by a consultant rheumatologist. It is therefore important to seek treatment with a rheumatologist early if showing signs of a severe inflammatory aspect of Sjögren’s syndrome that is causing damage to other organs or if Sjögren’s syndrome is secondary to an accompanying autoimmune or rheumatic condition, such as rheumatoid arthritis or lupus.
The most common DMARDs include methotrexate, hydroxychloroquine, and sulfasalazine. These are now often referred to as conventional DMARDs since the advent of biological DMARDs in recent years. Similar efficacy has been reported for methotrexate and sulfasalazine in studies of up to 12 months.12,13 The response of DMARDS is usually monitored every one-to-three months initially until symptoms improve.
Prognosis
The outlook in terms of mortality for Sjögren’s is not unfavourable, even though quality of life is affected. The authors of a 2017 study wrote: “Overall, the prognosis of Sjögren’s syndrome is favorable. The life expectancy of pSS [primary Sjögren’s syndrome] patients is comparable with that of the general population… However, the patients’ quality of life is reduced by the diverse manifestations of the disease. Cardiovascular disease, infections, solid tumors, and lymphoma are the main causes of death. In patients with sSS, life expectancy is determined by the primary disease.”14
References
- https://www.eyedoctors.ie/your-eye-health/
looking-after-your-eyes.asp. - Nikolov NP, Illei GG; Pathogenesis of Sjögren’s
syndrome. Current Opinion on Rheumatology.
2009 Sep; 21(5):465-70. - Ramos-Casals M, Brito-Zerón P, Sisó-Almirall
A, Bosch X. Primary Sjögren’s syndrome. British
Medical Journal. 2012;344:e3821 doi: 10.1136. - Mayo Clinic: Sjögren’s syndrome.
https://www.mayoclinic.org/diseasesconditions/sjogrens-syndrome/symptomscauses/syc-20353216. - Kassan SS. Managing dry eyes and dry
mouth in Sjögren’s syndrome. American Journal of Managed Care. 2001;7
(supplement):S444-S450. - Chang HJ, Burke AE, Glass RM. Sjögren syndrome. JAMA, July 28, 2010, Volume 304, No 4.
- Gemignani F, Marbini A, Pavesi G, et al.
Peripheral neuropathy associated with primary
Sjögren’s syndrome. Journal of Neurology,
Neurosurgery and Psychiatry. 1994;57:983-986. - Arthritis Foundation. Sjögren’s’s syndrome.
Self-Care, 2021. - Papas AS, Sherrer YS, Charney M, et al; Successful Treatment of Dry Mouth and Dry Eye
Symptoms in Sjögren’s Syndrome. Patients
with Oral Pilocarpine: A Randomised, PlaceboControlled, Dose-Adjustment Study. Journal of
Clinical Rheumatology. 2004 Aug;10(4):169-177. - Ramos-Casals M, Tzioufas AG, Stone
JH, Sisó A, Bosch X. Treatment of primary
Sjögren’s syndrome: A systematic review.
JAMA 2010; 304:452-60. - SPC for Salazopyrin®. Available at
www.medicines.ie. - Lee D, Weinblatt M, Rheumatoid arthritis.
The Lancet 2001; 358: 903-11. - Young A, Rheumatoid arthritis: Current approaches to drug treatment. Prescriber 19 Jan
2004; pages 48-55. - Ana-Luisa Stefanski, Dr med, Christian Tomiak, Dr med, Uwe Pleyer, Prof Dr med, Thomas
Dietrich, Prof Dr med Dr med dent, Gerd
Rüdiger Burmester, Prof Dr med, and Thomas
Dörner, Prof Dr med. Diagnosis and Treatment
of Sjögren’s Syndrome. Dtsch Arztebl Int. 2017
May; 114(20): 354–361.







