A clinical synopsis of assessment and treatment options for a number of common and troublesome wounds.
I will discuss three types of wounds in this article. The three types are:
- Diabetic foot ulcers.
- Post-operative wounds (the basics).
- Pressure sores.
The aim of this article is not to go in depth into the causes and management of wounds, but to give the basic advice patients and their carers need to prevent, manage, and treat these wounds under the supervision of health professionals.
DIABETIC FOOT ULCERS
Diabetics have more foot problems than the general population due to their condition. Unfortunately, diabetics are at increased risk of serious foot problems, including gangrene, which can lead to amputation. However, these problems are preventable with proper foot care. Foot care is very important for diabetics, but especially if there is a loss of feeling in the feet, changes in the shape of feet, and foot ulcers or sores that do not heal. Nerve damage can cause loss of feeling in the feet. A diabetic may not feel a pebble inside their sock that is causing a sore, or a blister caused by poorly-fitting shoes. Foot injuries like these can cause ulcers, which may lead to amputation. Keeping blood sugar under control can help avoid serious foot problems.
A diabetic may not feel a pebble inside their sock that is causing a sore, or a blister caused by poorly-fitting shoes
ASSESSING A DIABETIC FOOT WOUND FOR INFECTION*
None: No signs and symptoms.
Mild: With at least two of below: Erythema 0.5-2cm/induration/tenderness/warmth/ pus discharge.
Moderate: Erythema >2cm and one of the findings above/OR: Infection penetrating to muscle tendon/bone/joint.
Severe infection/sepsis: Presence of systemic signs with at least two of below: Temperature >39°C or 90bpm/ respiratory rate >20/mi.
*Ref: IWGF (2019) IWGDF Guideline on the classification of diabetic foot ulcers. IWGDF Guidelines on the Prevention and Management of Diabetic Foot Disease
PREVENTION OF DIABETIC FOOT PROBLEMS
With a five-year mortality rate of more than 50 per cent in diabetes patients with foot ulcers and 80 per cent in patients who have a diabetes-related amputation, diabetes-related foot ulcer five-year mortality rates are similar or even worse than many types of common cancers. The key is prevention and regular check-ups. The basic tips below are essential, as prevention is easier than cure.
CHECK FEET DAILY
Diabetics may have serious foot problems but feel no pain. Look for cuts, sores, red spots, swelling, or infected toenails. Find a time (evening is best) to check feet each day. If you have trouble bending, use a mirror to help.
WASH FEET DAILY
Wash feet in warm, not hot, water. However, do not soak feet, as this will cause the skin to get dry. Before bathing or showering, test the water to make sure it is not too hot. Use a thermometer (32 to 35oC is safe) or elbow. Dry feet well, taking care to dry between toes.
KEEP FEET MOISTURISED
Rub a thin coat of skin lotion, cream, or petroleum jelly on the tops and bottoms of the feet. Do not put lotion or cream between toes, because this might cause an infection.
DO NOT OVERDO IT
If using a pumice stone to smooth corns and calluses after bathing or showering, rub gently, in one direction only, to avoid tearing the skin. Do not cut corns and calluses. Diabetics should not use razor blades, corn plasters or liquid corn and callus removers, as they can damage skin.
KEEP TOENAILS TRIM
Cut toenails each week or when needed. Wash and dry your feet first. Trim toenails straight across and smooth them with an emery board or nail file. Do not cut into the corners of the toenail, as this can cause in-growing toenails. If eyesight is poor, if toenails are thick or yellowed, or nails curve and grow into the skin, have a chiropodist trim them.
WEAR SHOES AND SOCKS
Wear shoes and socks at all times. Do not walk barefoot — not even indoors — because it is easy to step on something and cause skin damage. Always wear socks, stockings, or nylons with shoes to help avoid blisters and sores. Socks that have no seams are best. Specially-designed socks for diabetics are ideal.
AVOID HOT AND COLD
Always wear shoes at the beach or on hot ground and put sunscreen on the top of feet to prevent sunburn. Keep feet away from radiators and open fires and do not put hot water bottles or heating pads on feet. Check feet often in cold weather to avoid frostbite.
KEEP THE BLOOD FLOWING
Put feet up when sitting. Wiggle the toes for five minutes, twice or three times a day. Move ankles up and down and in and out to improve blood flow. Do not cross your legs for long. Do not wear tight socks, elastic or rubber bands, or anything restrictive around your legs. Stop smoking, as it reduces blood flow to feet.
SEE A HEALTH PROFESSIONAL
Diabetics should visit a chiropodist once every six months. Chiropodists are experts in foot health and should be the first stop if foot problems occur, especially in diabetics, as even minor issues can turn into serious problems very rapidly. Pharmacists and GPs can also help with foot problems.
TREATING POSTOPERATIVE WOUNDS (THE BASICS)
Many patients with postoperative wounds will be required to treat the wounds at home with the help of their healthcare professionals, including their GP, practice nurse and public health nurse.
| SINBAD SCORING FOR INDEX ULCER NO=0 YES=1 | ||
| Site: rearfoot? | No | Yes |
| Ischaemia: clinical signs of peripheral vascular disease? | No | Yes |
| Neuropathy: Sensory loss? | No | Yes |
| Bacterial infection: clinical signs? | No | Yes |
| Area: 1cm2 or more? | No | Yes |
| Depth: to tender or bone? | No | Yes |
| Total (yes only) | /6 |
Score = or > than 4/6 highest risk of amputation
SINBAD = Site, Ischaemia, Neuropathy, Bacterial Infection and Depth
SURGICAL WOUNDS
A surgical wound is the cut made to the skin by the surgeon during an operation. At the end of the operation, the cut is joined back together with either stitches, Steristrips or adhesive dressings (glue) to allow the skin edges to come together and heal. The skin edges usually form a seal within a day or two of the operation. The time this takes varies from person-to-person and from operation-to-operation.
DRESSINGS
Not all surgical wounds need dressings. The purpose of a dressing is to:
- Absorb any leakage from the wound.
- Provide ideal conditions for healing.
- Protect the area until the wound is healed.
- Prevent stitches catching on clothing.
STITCHES
Stitches are also known as sutures. Adhesive dressings (glue), Steristrips or tape may also be used. Most types of stitches are removed by a nurse or doctor, but some stitches do not need to be removed, as they dissolve. Stitches are usually removed 14 days after treatment, depending on the type of operation.
PROBLEMS WITH WOUND-HEALING
Most wounds heal without any problems. The most common complication after surgery is wound infection. An infection usually delays normal wound-healing.
WOUND INFECTIONS
Some people are more likely to develop wound infections than others. People are at an increased risk of infection if they:
- Smoke.
- Are diabetic.
- Have a condition or are having treatment which affects the immune system, such as leukaemia or chemotherapy.
It is important for the patient to know the signs of infection after going home. If a wound becomes infected, it may:
- Become more painful.
- Look red or swollen.
- Leak some blood-like liquid, pus, or blood.
- Have an unpleasant smell.
If the patient develops a high temperature (above 37.5°C), or notices any of the signs mentioned above, or have any concerns about the wound, they should contact the surgery team or GP as soon as possible.
CARING FOR A WOUND
There are measures to prevent infection and increase healing.
CHANGING THE DRESSING
The original dressing can be left in place for up to two days (or as advised by the nurse/doctor) if it is not oozing. The wound must be kept dry for two days. If the dressing becomes wet from blood or any other liquid, it must be changed.
When changing the dressing:
- Wash hands with soap and water.
- Carefully take the dirty dressing off, without touching the used side.
- Do not touch the healing wound with fingers.
- Take care not to touch the inside of the new dressing, so that it remains clean.
- Do not apply antiseptic cream under the dressing.
If the wound is healing, it can be left without a dressing, but the patient may prefer to have a dressing to cover the wound for protection, especially if clothing can rub against it.
TAKING CARE OF STITCHES
Dissolving stitches usually disappear in seven-to-10 days. Other stitches need to be removed after 14 days. The surgery team will explain when to have these stitches removed on the day of discharge from hospital. Nylon threads (the ends of the stitches) may poke out of the healing scar. Do not pull on these. If the loose ends are catching on clothes, cover the wound until the stitches are removed, to prevent them catching.
BATHING AND SHOWERING
Wait 24 hours after surgery before showering. When washing, follow this advice:
- Showering is preferable to bathing. Soaking the wounds might soften the scar tissue and cause it to open. Only take a bath if sure the wounds can be kept dry.
- Some waterproof dressings can be left in place whilst taking a bath or shower. Other dressings may need to be removed beforehand.
- Do not put any soap, shower gel, body lotion, talcum powder or other bathing products directly onto a healing wound. This will cause discomfort and may also encourage an infection.
- Do not worry if splashing occurs on the wound, but do not rub the wound area. This will cause pain and might delay the healing process.
- Pat the wound dry gently with a clean towel after bathing or showering.
PRESSURE SORES
Pressure ulcers are lesions caused by unrelieved pressure that results in damage to the underlying tissue. Generally, these are the result of soft tissue compression between a bony prominence and an external surface for a prolonged time.
So long as there is no arterial disease, venous leg ulcers benefit from elevation and compression dressings
CLINICAL MANIFESTATIONS AND DIAGNOSIS
Pressure ulcers are usually easy to identify by their appearance and location overlying a bony prominence. It is important to distinguish pressure ulcers from ulcers that result from diabetic neuropathy or arterial or venous insufficiency. They also may be confused with other conditions that cause redness of skin, such as cellulitis. Superficial moisture-induced lesions, such as maceration (softening and whitening of skin) over a bony prominence, should not be labelled as pressure ulcers. Characteristics of lesions that need to be distinguished from pressure ulcers are:
- Diabetic neuropathic ulcers are seen in patients with diabetes who have peripheral neuropathy. The diabetic ulcer characteristically occurs on the foot, usually on the ball of the foot just behind big toes or on the top of toes.
- Venous insufficiency ulcers are usually found on the inner part of the lower leg, usually just above the ankle. Approximately 70 per cent of all leg ulcers are venous ulcers. They can occur either on one or both legs and each leg may have more than one ulcer. They can range from painless to extremely painful. These types of ulcers are common in people who have a history of leg and feet swelling. The ulcer usually presents itself as an open sore in an area that already typically exhibits a red-to-brown discolouration that has probably been present for some time. The area will also be swollen. Prior to the formation of the ulceration, the skin may have also been somewhat flaky and itchy as well. So long as there is no arterial disease, venous leg ulcers benefit from elevation and compression dressings.
- Arterial ulcers occur as the result of arterial occlusive disease. Approximately 10 per cent of all leg ulcers are arterial ulcers. Feet and legs often feel cold and may have a whitish or bluish, shiny appearance. Arterial leg ulcers can be painful. Pain often increases when the legs are at rest and elevated.
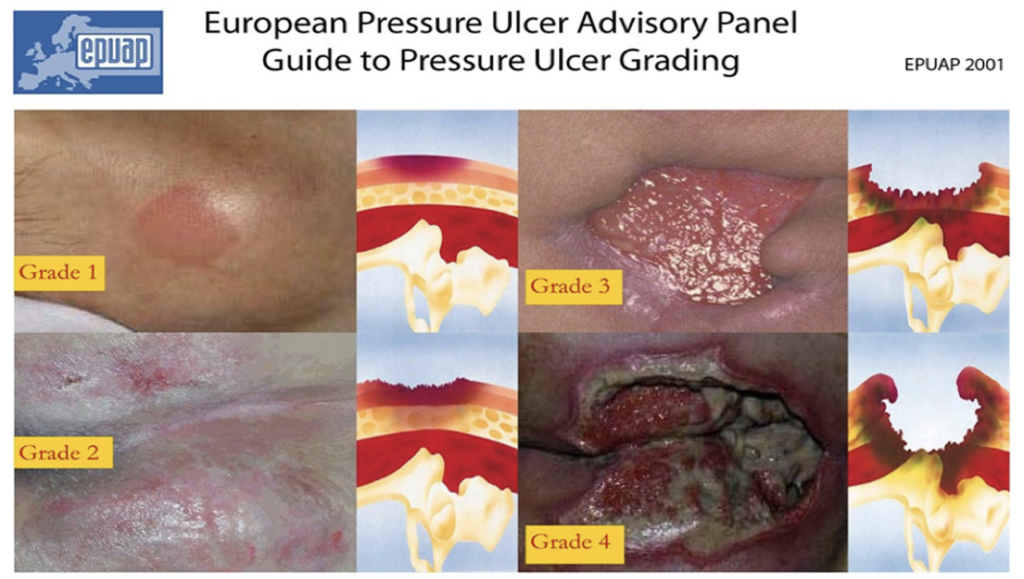
CLASSIFICATION SYSTEM
- Grade 1: Redness that does not whiten on touch. Discolouration of the skin, warmth, oedema, and hardness may also be used as indicators, particularly on individuals with darker skin in whom it may appear blue or purple. Grade 1 may be more difficult to detect in those with dark skin tones.
- Grade 2: Partial thickness skin loss involving epidermis, dermis, or both. The ulcer is superficial and presents clinically as an abrasion or blister. Surrounding skin may be red or purple. If bruising is visible at this stage, it can indicate deep tissue injury.
- Grade 3: Full thickness skin loss involving damage to or necrosis of subcutaneous tissue. Subcutaneous fat may be visible, but tendon, muscle or bone are not exposed. Slough may be present.
- Grade 4: Extensive destruction, tissue necrosis, or damage to muscle, bone, or supporting structures with or without full thickness skin loss. Extremely difficult to heal and can lead to fatal infection.
Unstageable — Full thickness tissue loss in which the base of the ulcer is covered by slough (yellow, tan, grey, green, or brown) and/or eschar (tan, brown or black) in the wound bed.
Eschar often covers deep ulcers, making it difficult to determine whether lesions are stage 3 or 4. Until enough slough and/or eschar is removed to expose the base of the wound, the true depth, and therefore stage, cannot be determined.
MAIN ASPECTS OF PREVENTION AND MANAGEMENT
- Repositioning of the patient regularly prevents pressure sores, ie, turning on the bed regularly if bed-bound.
- Treatment of concurrent conditions which may delay healing, ie, poor circulation.
- Pressure-relieving support surfaces such as beds, mattresses, overlays, or cushions.
- Local wound management using modern or advanced wound dressings and other technologies.
- Patients with identified grade 1 pressure ulcers are at a significant risk of developing more severe ulcers and should receive interventions to prevent deterioration.
PAIN RELIEF
- Pain is often significant and disabling for those with pressure ulcers.
- Paracetamol may be sufficient, but patients often require stronger analgesia.
- Non-steroidal anti-inflammatory drugs may increase peripheral oedema and are inappropriate for patients with pressure ulcers, ie, Ibuprofen, Diclofenac.
- Opioid analgesics may be needed for moderate-to-severe pain.
- Topical local anaesthetics such as lidocaine can provide numbness for a short period of time and can be useful for a specific procedure, but should not be used as the only method of pain relief.
- Wound-cleansing and dressing techniques may need to be reconsidered if they are causing severe pain. Adequate pain control should be provided for dressing changes and debridement.
- Patients may require a referral to a pain clinic.
NUTRITION
If oral intake is not adequate to ensure sufficient calories, protein, vitamins, and minerals, nutritional supplementation with enteral and parenteral nutrition (PEG feed) is recommended to correct deficiencies. Increased dietary protein intake promotes the healing of pressure ulcers. The protein target is usually 1.5g/kg/day. Cubitan is an example of a high-energy, high-protein oral nutritional supplement (ONS) with wound-specific nutrients (arginine, vitamin C, zinc, vitamin E). It increases healing times of pressure sores in under-nourished patients. However, it is important that oral nutritional supplements are reviewed regularly by a dietitian. While high-protein ONS such as Cubitan have a role in helping heal ulcers and other wounds, they should be discontinued promptly once the wound has healed. Food is the best vehicle for appropriate nutrient consumption. According to the National Medicines Information Centre in St James’s Hospital, Dublin, no studies have yet determined the optimum usage of ONS in terms of the most appropriate patients, the optimum dose, and duration of use. Despite lack of evidence, ONS has a role in many circumstances; therefore, it is important to liaise with nutrition specialists such as dieticians before ONS can be recommended. For the added reason of the high cost of ONS to the State, the HSE also recommends that ONS is only commenced after the patient is assessed by a dietician.
DRESSINGS
There is no conclusive research evidence to guide healthcare professionals’ decision-making about which dressings are most effective in pressure ulcer management.
However, professional consensus recommends that modern dressings (ie, hydrocolloids, hydrogels, foams, films, alginates, soft silicones) should be used in preference to basic dressing types, ie, gauze, paraffin gauze and simple dressing pads.
Grade 1 ulcers may be dressed in transparent films for protection, ie, Tegaderm, Opsite. Grade 2 pressure ulcers usually require an occlusive or semi-permeable dressing that will maintain a moist wound environment, ie, Comfeel Plus, Granuflex.
Ulcers with heavy exudate require an absorptive dressing to avoid build-up of chronic wound fluid that can lead to wound maceration and inhibit healing. An appropriate wound dressing can remove excess wound exudate while maintaining a moist environment to accelerate wound healing. Dressings with absorptive qualities include alginates, ie, Kaltostat, foams, ie, Allevyn, Biatain, and hydrocolloids, ie, Aquacel, Comfeel, Granuflex.
Desiccated ulcers are dry ulcers that lack wound fluids which help promote healing. Thus, pressure ulcer healing is promoted by dressings that maintain a moist wound environment while keeping the surrounding intact skin dry. Choices for a dry wound include hydrogels, ie, Granugel, Intrasite Gel, and hydrocolloids, ie, Aquacel, Comfeel, Granuflex.
DEBRIDEMENT
Necrotic tissue promotes bacterial growth and impairs wound-healing. Wound debridement may involve any of five approaches: Use of sharp dissection (take care when doing this on heels); mechanical debridement (wet-to-dry dressings); application of proteolytic enzymes; autolytic debridement under occlusive dressings (hydrocolloids or hydrogels); or biosurgery with sterilised maggots.
INFECTION CONTROL
- Reduce risk of infection and enhance wound-healing by hand-washing, wound-cleansing, and debridement. Protect from external sources of contamination, ie, faeces.
- If purulent material or foul odour are present, more frequent cleansing and possibly debridement are required.
- When there are clinical signs of infection which do not respond to treatment, x-rays should be undertaken to exclude osteomyelitis and joint infection.
- Systemic antibiotics are required for patients with bacteraemia, sepsis, advancing cellulitis or osteomyelitis.







