One Of The Most Important Steps In Treating Migraine Is Recognising Whether Or Not The Patient Has A Headache Or Their Pain Is Actually A Migraine.
One of the most important first steps in the successful management of headache is diagnosing whether migraine is, or is not, the cause of the headache. Migraine is quite distinct from other headache types in how it presents and in how an episode evolves, attacks, and subsides. I discuss both ‘non-migraine’ and ‘migraine’ headaches to help distinguish between both and the treatment options for both, considering many painkillers are used for both types. Secondary headaches are a common problem; secondary headaches are headaches caused by other medical conditions or medication. Medication overuse headaches are a significant problem and are often associated with codeine overuse and addiction. The headaches I discuss here are primarily chronic headache disorders, but many have acute phases.
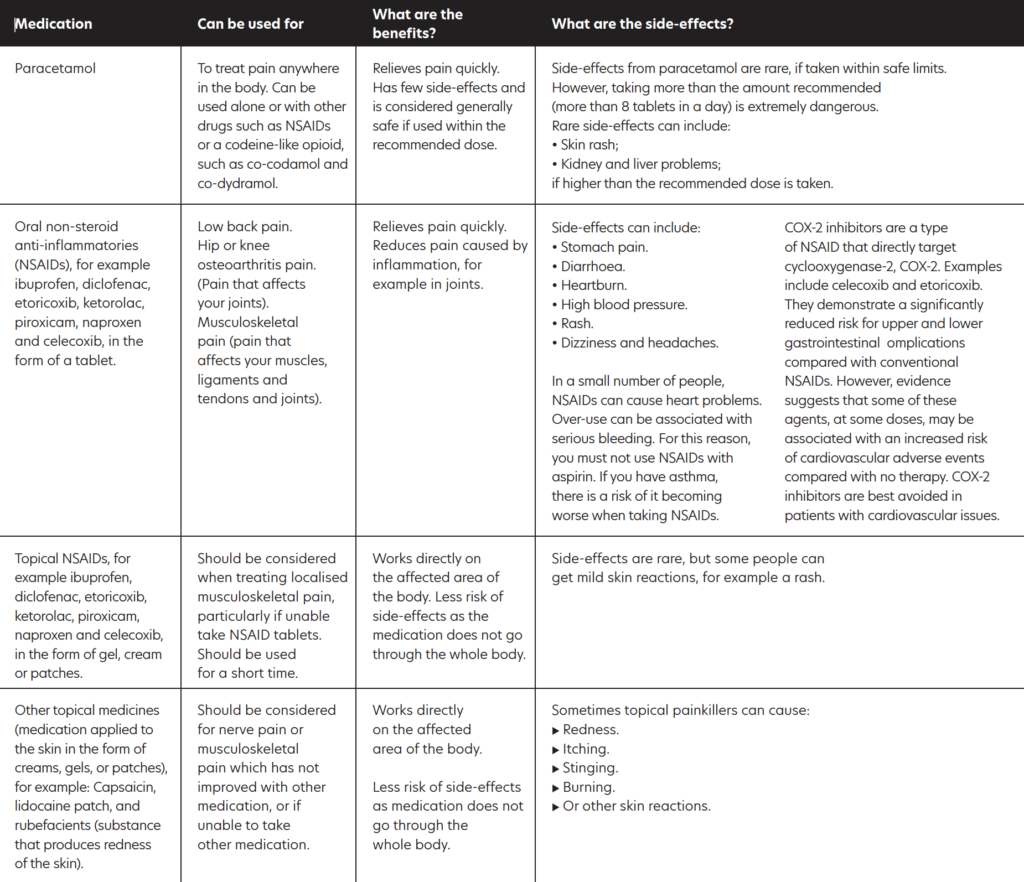
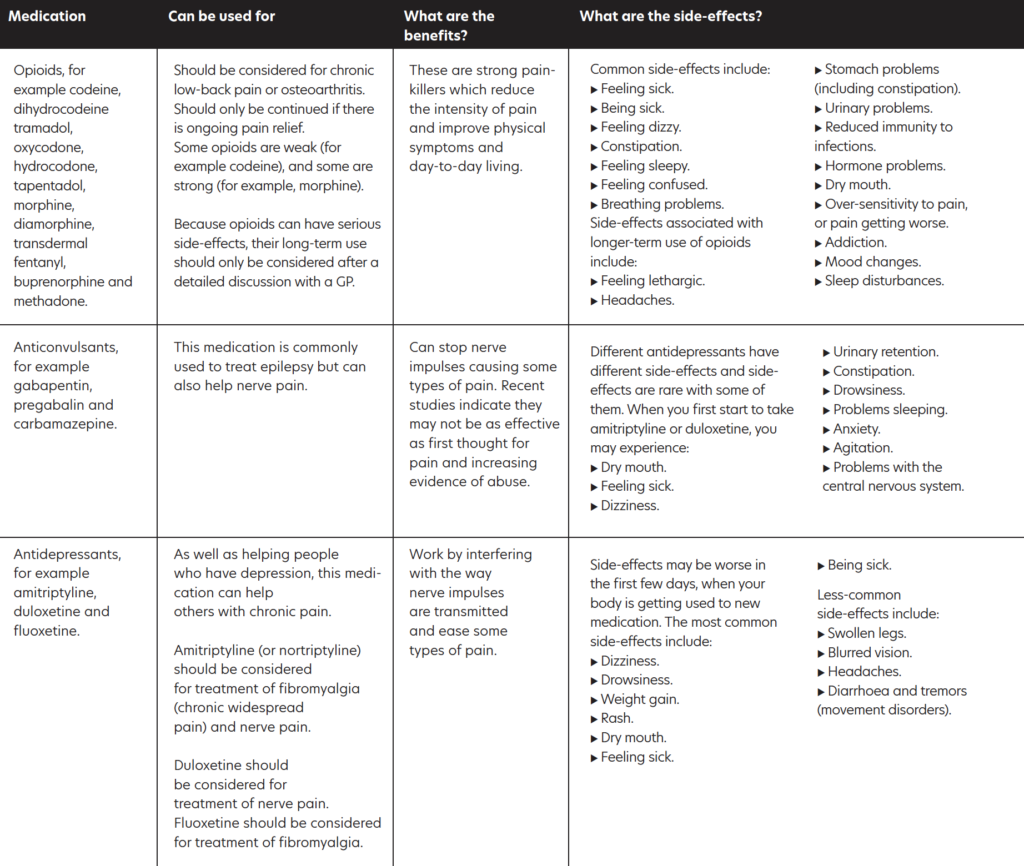
OVERVIEW OF PAIN MEDICATIONS
As well as discussing the types of headache experiences, I summarise in Table 1 the main types of painkillers available.
A. NON-MIGRAINE HEADACHES
1. Tension headache
The most common type of headache are tension headaches and these are usually caused by stress, poor posture, or inadequate lighting. Often beginning in the afternoon or early evening of a stressful day and presenting as a ‘band-like’ or ‘pressing’ sensation at the front of the head, they can last from one-to-six hours.
With tension headache, pain tends to be bilateral (both sides of head), constant and with no other symptoms, as opposed to migraine, which is usually confined to one side of the head, together with other identifiable symptoms.
For most, treatment with an analgesic (paracetamol, aspirin, or ibuprofen) usually takes care of it. Engaging in self-management activities such as regular exercise, regular eye breaks from the computer at work, sensible eating habits and learning stress management techniques can all lead to a reduction in tension headaches.
2. Chronic daily headache
Different from tension headache, which is episodic in nature, chronic daily headache (CDH) refers to any headache that occurs on at least 15 days per month, with each at least four hours’ duration. Currently affecting 4-to-5 per cent of the population (and growing), variants of CDH can significantly affect an individual’s ability to function at work, at home and socially.
There are three distinct types:
> Chronic tension headache
Typically affects those with a history of ordinary tension headache and whilst similar, it occurs on at least 15 days per month. Whereas tension headache is usually related to individual situations, chronic tension headache tends to be provoked by more enduring ongoing personal situations, ie, job issues, family and relationship problems, grief, depression.
> Chronic (transformed) migraine
Diagnosed if you have migraine on 15 or more days a month over a period of at least six months. Over time, people with this diagnosis may experience an additional daily or almost-daily headache. As the frequency of these headaches increases, there is a corresponding decrease in actual headache pain, along with other migraine symptoms. The downside of this perceived relief is that the headaches become less responsive to treatment. With other effects such as depression and sleep disturbance, people will usually experience a more typical ‘breakthrough’ migraine attack on top of the enduring ‘background’ headache. See more on migraine later.
> Medication overuse headache
This is caused by the overuse of medication, taken primarily to alleviate headache. In the main, this relates to analgesics (paracetamol, aspirin, ibuprofen, but with codeine being the worst culprit), although can also occur with migraine-attacking drugs (triptans). Those most commonly affected are those with a history of tension headaches or migraines that have become more frequent or severe over time. They take medication to gain relief from the pain, only to find the headache returning once the drugs have worn off. Sufferers then take more medication to alleviate continued pain, pain eases, drugs wear off, pain returns, etc (a vicious circle). It becomes easy then to fall into a cycle of taking medication for a headache that is itself caused by medication. Once in this spiral, the only way to break the cycle completely is through withdrawal. This is best achieved through consultation with a doctor. Typical withdrawal side-effects can be worsening headaches, nausea, and anxiety for a couple of weeks.
3. Cluster headache
Affecting around 1 per cent of people, this is a rare but very severe headache found six times more commonly in men than women, and usually begins in late 20s or early 30s. Typically, attacks begin in the middle of the night. Primary symptom is a severe stabbing pain affecting one side of the head. The side affected can vary between attacks, but only in very rare cases would it affect both sides of the head at the same time. The duration of an attack can be between 15 minutes and up to three hours. Attacks come in clusters (hence the name) and can occur several times a day over a period of weeks or even months. After each cluster though, attacks
can disappear for months or years.
A cluster attack can be distinguished from a migraine attack in that with cluster headache, the person is agitated during an attack or unable to sit or lie at peace or find relief though sleep.
During an attack, other symptoms may occur, such as red or watery eyes, runny nose, nasal congestion, or facial sweating. In addition, a sufferer’s eyes may be affected, with constriction of the pupil or drooping or swelling of the eyelid. Cluster headache has been described by some medics as ‘the most painful event that can happen a person’.
Whilst the cause is unknown, suspected trigger factors include alcohol, tobacco, irregular sleeping patterns, and stress and decreased blood oxygen levels. The most common treatment for cluster headache is the inhalation of pure oxygen and is only successful if the mask fits perfectly.
The three primary types of headaches described above are the most common non-migraine headaches. There are other types of headaches, ie, those relating to sinus problems or over-exertion, especially exercise. These are known as secondary headaches.
B. MIGRAINE
I discussed migraine in detail in Irish Pharmacist earlier in 2022 (including the new migraine treatments called anti- CGRPs), so this month’s article is a quicker summary of migraine.
COMMON SYMPTOMS AND TYPES
The word ‘migraine’ derives from a Greek word hemikrani (half-skull), which literally means ‘pain on one side of the head’. This accurately describes and differentiates migraine from other types of headaches as typically, it presents on one side of the head.
An attack may consist of some or all the following symptoms:
- Migraine without aura (around 80 per cent of all attacks).
- Moderate-to-severe pain, throbbing one-sided headache, aggravated by
- movement.
- Nausea and/or vomiting.
- Hypersensitivity to external stimuli (ie, noise, smells, light).
- Stiffness in neck and shoulders.
- Pale appearance.
MIGRAINE WITH AURA (IN ADDITION TO ABOVE SYMPTOMS)
- Aura: Around 20 per cent experience visual disturbances prior to the headache lasting up to one hour (most commonly blind spots, f lashing light effect or zig-zag patterns; may also include physical sensations such as unilateral pins and needles in fingers, arm and then face).
- Blurred vision.
- Confusion.
- Slurred speech.
- Loss of co-ordination.
Other types:
BASILAR MIGRAINE
Usually affecting teenage girls, this is a rare form of migraine that presents additional symptoms such as loss of balance, fainting, difficulty speaking, and double vision. There can be loss of consciousness during an attack.
HEMIPLEGIC MIGRAINE (SPORADIC OR FAMILIAL)
Usually beginning in childhood, this severe form of migraine causes temporary unilateral paralysis. May also feature extended aura period that could last for weeks. Generally related to a strong family history of the condition. It is a rare form of migraine; diagnosis usually requires a full neurological exam, as the symptoms may be indicative of other underlying conditions.
OPHTHALMOPLEGIC MIGRAINE
In addition to headache, this very rare form of migraine shows additional symptoms, such as dilation of the pupils. Inability to move the eye in any direction, as well as drooping of the eyelid, occurs. It occurs primarily in young people and is caused by weakness in the muscles which move the eye.
ABDOMINAL MIGRAINE
Symptoms are usually nausea- and stomach-related rather than headache. Occurs predominantly in children, usually evolves into typical migraine with age.
MIGRAINE TRIGGERS
A myriad of trigger factors, whilst in themselves not the cause of migraine, can build, bringing an individual to the point where a migraine attack is imminent.
Again, these can be different for everyone and indeed, may differ for an individual each time, depending on their situation; trying to track down specifics can be difficult. The most common triggers include:
ENVIRONMENTAL FACTORS
Just moving around doing normal day-to-day activities can be a potential danger for someone susceptible to migraine:
- Bright or flickering lights (could be cinema, shop displays or sunlight through trees).
- Certain types of lighting (fluorescent, strobe).
- Strong smells (especially perfume, paint, etc).
- Weather (variety of factors, ie, bright sun glare, muggy close days, humidity).
- TV/computer screens and monitors.
- Loud and persistent noise.
- Travel areas of pressure change, ie, altitude.
DIETARY TRIGGERS
Research indicates about 20 per cent of migraine attacks are brought on by dietary factors. Whilst people believe this to be the case, actual scientific evidence proving a link is virtually non-existent. In many cases, there may be other factors that precede consuming a ‘suspect’ food that could contribute more to the onset of an attack, ie, lack of sleep, skipping meals.
The most-cited link is foods which are high in the amino acids tyramine and/or phenylethylamine, such as:
- Cheese (fermented, aged, or hard mouldy types).
- Chocolate.
- Alcohol (beer and red wine particularly).
- Nitrites (common in processed meats).
- Sulphites (ie, preservatives in dried fruit and red and white wine).
- Additives (MSG).
- Aspartame (diet drinks).
- Caffeine (coffee, tea, etc; although caffeine can be used to prevent migraine, it is down to personal tolerance).
HORMONAL TRIGGERS
Once females move into puberty and then adulthood, hormones play an increasing role in migraine prevalence. Oestrogen fluctuations due to menstruation or using oral contraceptive pills or HRT can sometimes trigger migraines. Conversely, migraine susceptibility can decrease during pregnancy when oestrogen levels are high.
In the main, migraine attacks lessen post-menopause (although can increase in the years preceding it). Identifying triggers can be the single-most important step an individual can take in helping themselves to manage their condition. A diary noting possible triggers including diet, sleep and other events, including symptoms, is important when seeing a doctor to seek treatment, as it will help the doctor better identify the type of migraine (or if it is even migraine) and help to better manage treatment. It may not be necessary to avoid situations completely, but instead build levels of awareness so that appropriate preventative steps and actions can be taken.
MEDICATION FOR MIGRAINE
Ideally, advise on promotion of self-help, self-management, and other treatments to help improve the condition and add value to the benefit offered by medication.
Given the wide and varied nature of chronic pain, there can be a myriad of medication options. The effectiveness of medication depends on the nature and severity of the pain. It is important that non-medication management options are considered, including exercise, relaxation therapies (especially for the likes of tension headaches), physiotherapy and cognitive behavioural therapy, just to name a few.
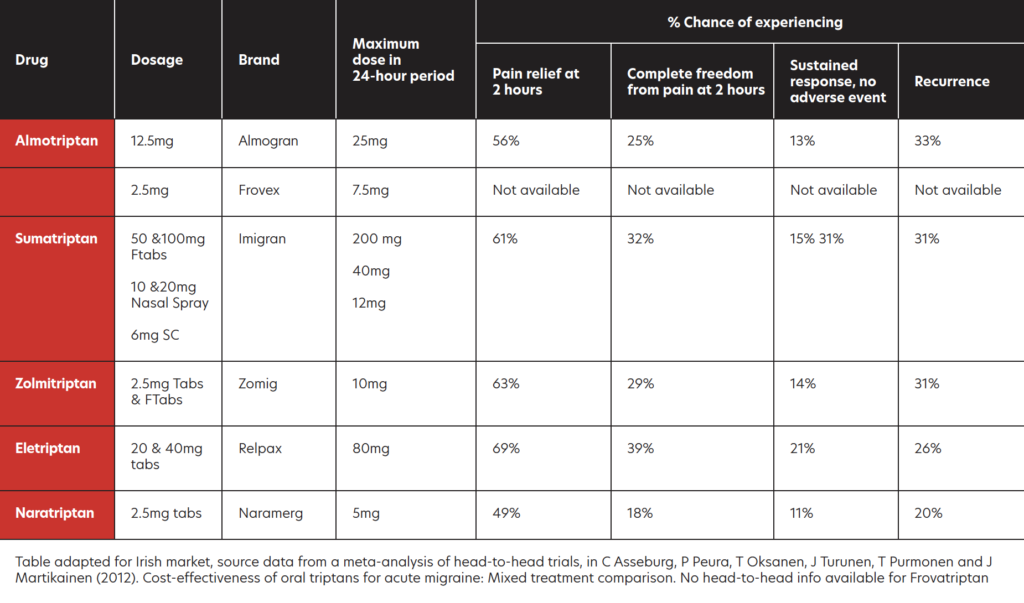
TRIPTANS
Regarding treatment of chronic pain caused by migraine, in addition to standard paracetamol and NSAIDs, triptans are considered the most effective to combat acute attacks if ordinary analgesics do not work.
All are POM, apart from sumatriptan, with an OTC version recently becoming available in Ireland.
PREVENTATIVE MEDICATION FOR MIGRAINE
I previously discussed preventative medication for migraine in Irish Pharmacist, so for this article, I only give a quick summary of the preventative options.
Prophylactic medication may be considered if the patient has taken adequate lifestyle steps to prevent migraine, such as using a diary to determine triggers and avoidance of these triggers, but the migraine continues. It would be reasonable for a prescriber to consider prophylaxis for migraine if a patient must use analgesics for eight or more days of the month. Prophylactic medication should be tried for four-to-six months at a reasonable dose to determine if it is working effectively.
Prophylactic medication has potential side-effects that can limit dose or use. Amitriptyline, topiramate and flunarizine are the three most-prescribed migraine prophylactic drugs, with amitriptyline being the most prescribed. Other prophylactics such as sodium valproate, pregabalin, gabapentin and pizotifen are considered second-line (often only used if the first three are not tolerated or ineffective).
NEW MIGRAINE DRUGS
A new class of migraine preventive drugs called anti-CGRPs are monoclonal antibodies that have come to market. These antibodies inhibit the action of a neurotransmitter called calcitonin gene-related peptide. The four CGRP inhibitors are erenumab, fremanezumab, eptinezumab and galcanezumab.
The two CGRP inhibitors currently licenced in Ireland are erenumab (Aimovig) and fremanezumab (Ajovy) and are subject to a strict protocol for prescribing.
CGRP — ITS ROLE IN MIGRAINE
The neurotransmitter calcitonin gene-related peptide, or CGRP for short, plays a role in migraine. Its role in migraine includes:
- Being released in the trigeminal nerve.
- Increasing levels are seen during migraine attacks.
- It dilates blood vessels.
- It reduces mast cells (cells that control inflammation during allergic reactions).
- Causes an inflammatory fluid in blood vessels.
For this reason, CGRP inhibitors are effective in reducing migraine.
ERENUMAB
The European Medicines Agency (EMA) authorised erenumab (Aimovig) in June 2018. It was the first monoclonal antibody to work by blocking the activity of CGRP for use for the prevention of migraine. Erenumab is licensed for prevention of migraine in adults who have migraines for a minimum of four days per month. The dose is a subcutaneous 70mg injection every four weeks. If not controlled with 70mg every four weeks, the dose may be increased to 140mg every four weeks.
Studies show erenumab is effective at reducing the number of days on which migraines occur. The most common side-effects with erenumab (up to one-in-10 people) are reactions at the site of injection, constipation, muscle spasms, and itching. If the patient gets side-effects, they are normally mild.
NCPE: COST-EFFECTIVENESS FINDINGS FOR ERENUMAB (AIMOVIG)
In January 2019, the NCPE considered the comparative clinical effectiveness and cost-effectiveness of erenumab (Aimovig) for the prevention of migraine in adults who have at least four migraine days per month. Concluding, the NCPE recommended erenumab for reimbursement at both the 70mg monthly dose and 140mg monthly dose for chronic headaches. They recommended that erenumab only be prescribed for chronic migraine patients who have tried three or more prophylactic treatments unsuccessfully. The NCPE did NOT recommend the reimbursement of erenumab for episodic migraine (less-regular migraine) due to cost-effectiveness concerns.
FREMANEZUMAB
In September 2020, the NCPE recommended fremanezumab (Ajovy) for the prevention of migraine in adults with chronic migraine who have tried three or more preventative treatments unsuccessfully. In 2021, the HSE Drugs Group via the HSE’s Managed Access Protocol (MMP) allowed access to eligible patients to the two CGRP inhibitors licenced in Ireland. Compared to erenumab, fremanezumab offers the flexibility of either monthly dosing (225mg once-monthly), or quarterly dosing (675mg every three months).
HSE MANAGED ACCESS PROTOCOL FOR CGRP INHIBITORS
The HSE’s Managed Access Protocol allowing access to eligible patients to the two CGRP inhibitors licenced in Ireland was approved by the MMP in October 2021.
For the two CGRP inhibitors licenced in Ireland — fremanezumab (Ajovy) and erenumab (Aimovig):
- HSE has the High-Tech Protocols for prescribing the treatments, meaning these medications may be prescribed only by consultant neurologists who have agreed to the terms of the MMP.
- GPs cannot prescribe them.
- The patient must have failed to get adequate treatment response from at least three of the following drugs before CGRP inhibitors can be prescribed:
- Amitriptyline/ nortriptyline.
- Botulinum toxin Type A (Botox).
- Candesartan.
- Flunarizine.
- Metoprolol/propranolol.
- Pizotifen.
- Sodium valproate.
- Topiramate venlafaxine.
KEY POINTERS: MIGRAINE OR NOT?
Pharmacists can be asked if the patient’s headache(s) is migraine or not. If a patient has a definitive diagnosis of migraine from their GP or neurologist, the treatment plan is relatively well mapped-out.
A challenge for pharmacists and other health professionals is advising on adequate pain relief for patients not yet diagnosed with migraine; for example, a pharmacist cannot sell OTC sumatriptan to a patient was not previously diagnosed with migraine. As I alluded to earlier, it can be hard to distinguish between migraine and other headaches.
KEY DISTINGUISHING FACTORS
Neurological symptoms
Whilst migraine is known to most as a ‘headache’, headache is only one symptom of a larger problem. Migraine is classed as a neurological disease, meaning for many patients, in addition to severe headache, it also leads to incapacitating neurological symptoms.
Neurological symptoms of migraine can include some or all the following:
- A severe throbbing-type headache.
- Visual disturbances (known as an aura).
- Nausea and vomiting.
- Extreme sensitivity to light, touch, and smell.
- Dizziness.
- Paraesthesia in the face, ie, numbness, tingling in the face or extremities.
Neurological symptoms with migraine can occur without any headaches. In 15- to-20 per cent of migraines, neurological symptoms develop before head pain. About 4 per cent of migraine patients do not have any headaches, meaning they only present with some of the neurological symptoms described above (ie, classical migraine aura), making it very hard to diagnose.
Migraine typically affects one side of the head
Another distinguishing factor between migraine and non-migraine headache is that migraine typically only affects one side of the head, whereas other types of headaches tend to affect the whole head, ie, a tension headache usually affects both sides; cluster headaches often present around the eye. However, it must be borne in mind that for a minority of migraine patients, the headache can affect both sides of the head.
Migraine is classed as a neurological disease, meaning for many patients, in addition to severe headache, it also leads to incapacitating neurological symptoms
Pain quality
Another difference between migraine and non-migraine headache is the pain’s ‘quality’: A migraine headache tends to cause intense pain that is throbbing in nature that makes performing daily tasks very difficult.
Migraine often associated with triggers
More so than other causes of headaches, migraine is often associated with a wide array of possible triggers that can bring on bouts of headaches.
The following factors can trigger migraines:
- Bright lights or flickering lights.
- Emotional stress and anxiety.
- Certain foods and drink, ie, chocolate, cheese, alcohol, and cured meats. Many of these foods contain tyramine, which is a known trigger for migraine.
- Changes in weather (humidity, heat, pressure).
- Hormonal changes in women.
- Loud noises.
- Irregular eating habits or skipping meals.
- Strong smells.
- Tiredness.
- Too much or too little sleep.
In relation to migraine triggers, each patient is unique, and patients get to know over time which triggers to avoid.







