An Overview Of The Causes, Diagnosis And Treatment Of Osteoarthritis
WHAT IS OSTEOARTHRITIS?
Osteoarthritis is by far the most common form of arthritis. Unlike rheumatoid arthritis, which is caused by inflammation, osteoarthritis is caused by ageing and long-term wear-and-tear in the joints. After years of use, the cartilage that cushions the joints can break down, until bone rubs against bone.
Osteoarthritis is rarely as crippling as rheumatoid arthritis, but it can have a big impact on a person’s life. It can make it hard to do everyday activities like getting dressed and walking up the stairs.
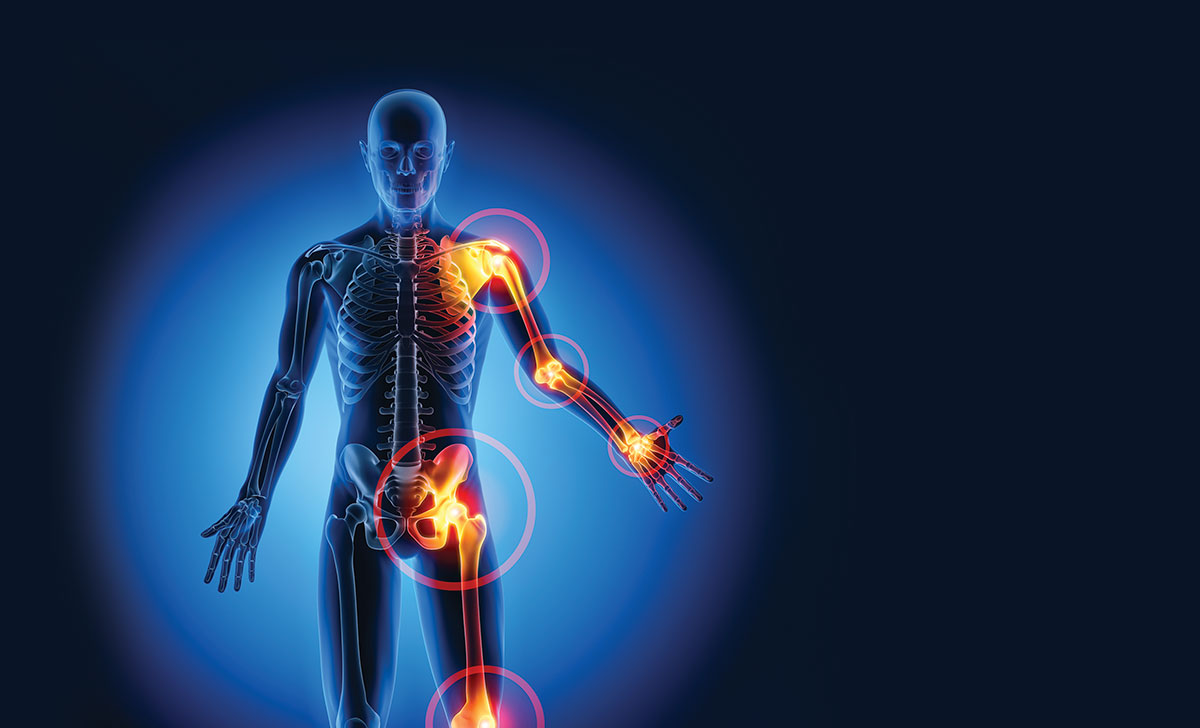
It most commonly affects the knees, hands, hips, and spine. It does not affect both sides equally and symmetrically as commonly as rheumatoid arthritis.
It causes more mobility disability in people over 65 than any other condition. Mobility disability means needing help walking or going up the stairs.
The condition is the number-one reason for joint-replacement surgery. It can take decades for enough cartilage to wear down to cause osteoarthritis. It occurs mostly in men after the age of 50 and in women after the age of 40. Women develop osteoarthritis mostly after menopause.
After menopause, women are twice as likely as men of the same age to develop the condition. Being overweight and a family history of arthritis makes you more prone to the condition.
WHAT HAPPENS?
Osteoarthritis occurs when the cartilage at the ends of bones becomes damaged.
Cartilage is a hard, slippery, and flexible substance that coats the end of a bone, which allows it to move smoothly against the next bone without rubbing together. When cartilage is damaged, the affected bone tries to compensate and repair itself by thickening and growing out.
These outgrowths are called ‘spurs’, or osteophytes. However, these outgrowths in osteoarthritis grow abnormally and make the problem worse. The bone can grow into an abnormal shape, making the joint unstable and painful.
RISK FACTORS
The exact causes are unknown, and it is not all due to ageing and wear-and-tear.
Certain factors make it more likely, such as:
- Being over the age of 40.
- Women are more at risk than men.
- If you are overweight or obese, as there is greater strain on the joints.
- Playing a lot of high-impact sports, ie, Gaelic football and rugby.
- If you have an injury or an operation on a joint, you are more likely to have problems later.
- There is evidence that it runs in families.
However, it has less of a tendency to run in families than rheumatoid arthritis.
SYMPTOMS
The main symptoms of osteoarthritis are pain and stiffness of the joints. The joints may also become swollen, although this is less common than in rheumatoid arthritis. The pain is exacerbated by activity and relieved by rest.
Unlike rheumatoid arthritis, where pain and stiffness tend to be worse in the morning, the pain of osteoarthritis tends to get worse throughout the day. With severe osteoarthritis, the patient can experience pain even at rest. The joints may not be able to move as easily as before.
After menopause, women are twice as likely as men of the same age to develop the condition
There may be a ‘crunching’ feeling in the joints. Joints may make creaking sounds, called crepitations. As osteoarthritis progresses, the joints may become misshapen and look knobby, and they may become unstable. Muscle weakness may occur around the affected joints.
Some people find that the symptoms are affected by changes in the weather or the amount of activity they do. Sometimes pain and stiffness can be more severe in the early stages, especially in women who develop osteoarthritis around the time of the menopause.
It then tends to settle down over the next few years.
DIAGNOSIS
Unlike other forms of arthritis, there is no single test that can check for osteoarthritis, so a GP will ask about symptoms and examine the joint.
He or she will look for bony outgrowths, swelling, creaking, instability, and reduced movement of the joint. An x-ray can show up any narrowing within the joint or outgrowths of bone. X-rays only give limited information and in the early stages of osteoarthritis, joints may look normal.
TREATMENT
- Self-help Certain actions can prevent and reduce the symptoms of osteoarthritis, including losing any excess weight, wearing shock-absorbent shoes, using a walking stick, and wearing a knee brace. Taking regular exercise is important, as it keeps weight down and strengthens muscles which support the joints. Swimming is the best exercise for osteoarthritis, as it strengthens muscles without putting strain on the joints. Walking and cycling are also beneficial. There is a lot of evidence that exercise helps osteoarthritis of the knee, but there is less evidence that it helps osteoarthritis of the hip.
- Braces and orthotics — Knee braces can be very beneficial for those with instability of the knee. A knee brace can take pressure off the knee joint and hence provide pain relief. However, knee braces are not suitable in all cases and patients should get medically assessed before using a knee brace, as it can make the problem worse if not used appropriately. Research has shown that heel wedges can reduce pressure on the knee joints, however there is no evidence that they improve knee symptoms if used alone.
MEDICINES
There is no cure for osteoarthritis, however certain medications will relieve symptoms
- Paracetamol — Over-the-counter painkillers such as paracetamol can help. They should not be used in combination with alcohol or in those with liver problems. Paracetamol is safe for most patients once taken within the recommended dosage limits.
- NSAIDs — If the pain is more severe, the doctor may prescribe anti-inf lammatory medicines known as non-steroidal anti-inf lammatory drugs (NSAIDs) to reduce the inf lammation. These are helpful in reducing pain, swelling and stiffness. Examples include diclofenac, naproxen or etoricoxib. Ibuprofen is an NSAID available over the counter in pharmacies. NSAIDs should be avoided or used in caution with asthma and heart problems and can cause stomach ulcers if overused. COX-2 selective NSAIDs are particularly associated with cardiovascular events in older people so should be avoided in the elderly, ie, etoricoxib, celecoxib. The doctor may consider a blood test to check if an NSAID is safe to use. Blood tests done before starting NSAIDs include creatinine concentration (checks kidney function) and liver function tests. These should especially be considered for the elderly and people with chronic illnesses, ie, kidney problems, bronchitis. Doctors often prescribe stomach protection medication such omeprazole or lansoprazole in combination with NSAIDs to prevent side-effects like stomach ulcers or bleeding.
- Topical preparations — Many NSAIDs are available in topical forms, such as creams or gels, which can be rubbed-on to give a local effect, ie, Difene Gel, Fastum Gel. These topical forms have fewer side-effects than NSAIDs taken orally. However, they are likely to be less effective, as less of the drug is absorbed. NSAID creams and gels are available on prescription and are allowed on the medical card (GMS) or DPS scheme. Topical diclofenac is available over the counter in pharmacies. Creams and gels containing capsaicin can give relief. Heat therapies such as a heat patch can also give some relief. Heat therapies are not allowed on medical card (GMS) or DPS schemes.
- Opioid analgesics — Opioid analgesics such as tramadol are a prescription- only painkiller, which may be considered in cases where NSAIDs are not tolerated or ineffective. However, opioids can become additive. Side-effects include drowsiness and constipation.
- Steroid Injections — Steroid injections into the affected joints may be a treatment option. It should only be considered where there is inf lammation in the joint. However, the effects of steroid injections only last up to four weeks (often only a week), so it is not a longterm solution.
- Supplements — Glucosamine and chondroitin supplements may provide pain relief. These chemicals are found naturally in cartilage, and it is thought that taking these supplements may improve the condition of damaged cartilage. They may also slow-down thinning of the cartilage. However, there is not enough evidence yet to prove that glucosamine and chondroitin help osteoarthritis. Because of lack of evidence, glucosamine was taken off the GMS approved list by the HSE a number of years ago, ie, no longer allowed on the medical card (GMS) or DPS schemes.
Hip resurfacing is an alternative to hip replacement and is more often used in younger patients
SURGERY
Surgery should only be considered when all other options have been tried. Surgical options available have advanced recently. Some options, such as realignment and hip resurfacing, are available even if you have only mild osteoarthritis.
Hip resurfacing is an alternative to hip replacement and is more often used in younger patients. It involves replacing the socket where the top of leg attaches to the pelvis with a ‘metal socket’.
The advantages of this compared to hip replacement is that it is very durable for young and active patients. It allows the patient to maintain full mobility, and even return to active sports in many cases. Some research shows that there is less pain and stiffness after hip resurfacing compared to hip replacement.
However, more research is needed to confirm this. Patients normally can resume normal daily activities a few weeks after hip resurfacing. Hip resurfacing lasts for 10- to-15 years on average. If you have a particularly painful joint, you may need an operation to replace it.
This is mostly done for the hip and knee joints, and both have high rates of success in improving mobility and reducing pain.
With proper selection of patients, 95 per cent of hip and knee replacements have excellent results, with 95 per cent of replacement joints lasting for 15 years. Eighty-five per cent of hip and knee replacements are due to osteoarthritis. References: Available upon request Disclaimer:
Brands mentioned in this article are meant as examples only and not meant as preference to other brands.
CONTRIBUTOR INFORMATION
Written and researched by Eamonn Brady (MPSI), owner of Whelehans Pharmacies in Mullingar Tel 04493 34591 (Pearse St) or 04493 10266 (Clonmore). www. whelehans.inet. Eamonn specialises in the supply of medicines and training needs of nursing homes throughout Ireland. Email ebrady@whelehans.ie