A review of pharmacological treatments for schizophrenia, anxiety and depression
For the purposes of this article, I focus primarily on pharmacological treatment options for three mental health conditions, namely depression, anxiety, and schizophrenia. There is some overlap in the medications used.
I will not outline the causes, symptoms, etc, of each condition and I do not discuss talking therapies in this article. Talking therapies such as CBT should be the first-line as a treatment option for these and many other mental health conditions; medication should always be used in tandem with talking therapies for mental health disorders like depression and anxiety.
This article is split in three parts:
- Part 1: Antidepressants.
- Part 2: Medication for anxiety.
- Part 3: Medication for schizophrenia.
Part 1: Antidepressants
The first antidepressants were developed in the 1950s. There are now about 30 different kinds of antidepressants available and there are six main types:
- Tricyclics.
- MAOIs (monoamine oxidase inhibitors).
- SSRIs (selective serotonin reuptake inhibitors).
- SNRIs (serotonin and noradrenaline reuptake inhibitors).
- NASSAs (noradrenaline and specific serotonergic antidepressants).
- Melatonergic agonists.
- Serotonin modulators.
How antidepressants work in brief
Antidepressants increase the activity of neurotransmitters serotonin and noradrenaline in the brain. Melatonergic agonists increase the release of melatonin in the brain, which has a positive effect on mood and sleep. Agomelatine (Valdoxan) is the only drug in this class so far.
What are they used for?
Antidepressants should never be used for mild depression; they should only be used for moderate-to-severe depression. Antidepressants are also used for the following conditions:
- Severe anxiety and panic attacks.
- Obsessive compulsive disorders.
- Chronic pain.
- Eating disorders.
- Post-traumatic stress disorder.
How well do they work?
After three months of treatment, it is estimated that 50-to-65 per cent of patients with depression show improvement when treated with antidepressants. This compares with 25-to-30 per cent of patients who are treated with a placebo.
Are newer antidepressants better?
Older tablets such as tricyclic antidepressants are just as effective as the newer ones (SSRIs), but the newer ones generally have less side-effects. Newer antidepressants are less dangerous on overdose. However, older antidepressants still have some benefits. For example, because tricyclic antidepressants cause more drowsiness, they are sometimes prescribed to be taken at night in patients suffering from severe insomnia due to depression.
Side-effects of antidepressants
The most common side-effects are as follows:
Tricyclics
Tricyclics commonly cause dry mouth, a slight tremor, fast heartbeat, constipation, sleepiness, and weight gain. These effects are reduced if a low dose is given to start and the dose is then slowly increased. Other side-effects which are more common in older people include confusion, inability to pass urine, and postural hypotension. They should be avoided in patients with heart conditions, as they can cause irregular heartbeat. They can cause erectile dysfunction and delayed ejaculation in men. Tricyclic antidepressants are dangerous in overdose, as they can cause cardiac problems. This is especially true for amitriptyline, which should not be used for depression. Amitriptyline is generally only used for nerve pain nowadays.
SSRIs
SSRIs can cause nausea and anxiety initially; however, these side-effects often wear off after a few weeks. They can cause indigestion, but this can be avoided by taking with food. They can cause sexual dysfunction, such as loss of libido. There have been rare reports of episodes of aggression.
Most people only experience mild side-effects (if any). The side-effects usually wear off over a couple of weeks as the body gets used to the medication. The more serious ones — problems with urinating, memory problems, falls, confusion — are uncommon in healthy, younger, or middle-aged people.
SNRIs
The side-effects are very similar to the SSRIs, although venlafaxine should not be used with a serious heart problem. It can also increase blood pressure, so this should be monitored, especially initially.
MAOIs
This type of antidepressant is rarely prescribed these days. This is because they can cause a hypertensive response (dangerously high blood pressure) if foods containing tyramine are eaten with them. Foods containing tyramine include mature cheese, pickled herring, broad bean pods, yeast extracts, including brands like Bovril, Oxo and Marmite. Even stale or gone-off food can cause this reaction.
NASSAs
Mirtazapine is the most common drug used in this group. The side-effects are very similar to SSRIs. It can cause drowsiness and weight gain, but it causes less sexual problems than SSRIs.
Antidepressant drugs do not have addictive properties like tranquillisers, alcohol, or nicotine
Melatonergic agonists
Side-effects include headache, migraine, and dizziness. It is considered to have less sexual side-effects and fewer withdrawal symptoms than other antidepressants.
More on the newest antidepressant on the market
As vortioxetine is the newest antidepressant on the market, I am going to discuss it in a little more detail than other antidepressants.
Serotonin modulator
Serotonin modulator is a relatively new class of antidepressant, used to describe vortioxetine (Brintellix), which is the only drug in this class. How it works is not fully clear, but it is thought to act as a serotonin reuptake inhibitor (SRI), agonist of the 5-HT1A receptor, and antagonist of the 5-HT3 and 5-HT7 receptors. It is indicated for major depressive illness and is generally reserved for when other antidepressants were not successful; generally where at least two other antidepressants were not successful.
There was no convincing clinical effectiveness evidence to show that vortioxetine was more or less effective than other antidepressants, but it may have a better overall safety profile than other antidepressants. Nausea is a very common side-effect, with the following being a common side-effect of vortioxetine: Dizziness, serotonin syndrome, flushing, diarrhoea, constipation, vomiting, pruritus and night sweats. It is recommended that treatment with vortioxetine is continued for at least six months after symptoms improve.
Vortioxetine is not associated with discontinuation symptoms, so it can be stopped abruptly without the need to taper the dose. Serotonin Syndrome (SS) or Neuroleptic Malignant Syndrome (NMS), potentially life-threatening conditions, may occur with vortioxetine. The risk of SS or NMS is increased with concomitant use of serotonergic-active substances (including triptans), medicinal products that impair the metabolism of serotonin (including MAOIs), antipsychotics, and other dopamine antagonists.
Patients should be monitored for the emergence of signs and symptoms of SS or NMS. Serotonin Syndrome symptoms include mental status changes (ie, agitation, hallucinations, coma); autonomic instability (ie, tachycardia, labile blood pressure, hyperthermia); neuromuscular aberrations (ie, hyperreflexia, incoordination); and/or gastrointestinal symptoms (ie, nausea, vomiting, diarrhoea). If this occurs, treatment with vortioxetine should be discontinued immediately and symptomatic treatment should be initiated.
The safety of vortioxetine in combination with other antidepressants has not been fully studied, but concomitant use should be avoided whenever possible. SS would be a risk if given with other antidepressants.
Are antidepressants addictive?
Antidepressant drugs do not have addictive properties like tranquillisers, alcohol, or nicotine. Therefore, the patient will not need to keep increasing the dose to get the same effect or they will not find themselves craving them when they stop taking them. However, up to a third of people who stop SSRIs and SNRIs have withdrawal symptoms which can last between two weeks and two months.
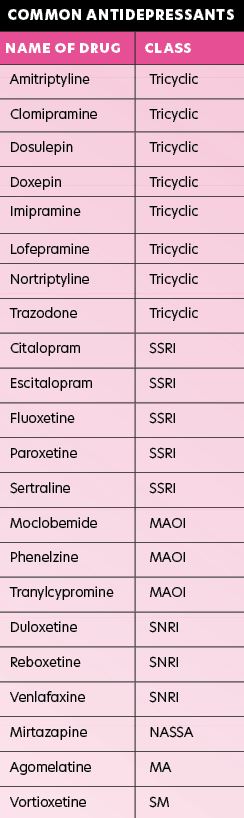
SSRI: Selective serotonin reuptake inhibitor
SNRI: Serotonin and noradrenaline reuptake inhibitor
MAOI: Monoamine oxidase inhibitor
NASSA: Noradrenergic and specific serotonergic antidepressant
MA: Melatonergic agonist
SM: Serotonin modulator
Withdrawal effects include gastrointestinal disturbance, headache, dizziness, sleep disturbance, fatigue, sweating and sensations in the body like electric shocks. In most people, these withdrawal effects are mild, but for a small number of people, they can be quite severe. They seem to be most likely to happen with paroxetine and venlafaxine. Withdrawal effects can be minimised by reducing them slowly when going off them.
Some people have reported that, after taking an SSRI for several months, they have had difficulty managing once the drug has been stopped and so feel they are addicted to it. However, most experts agree this is due to the depression returning after discontinuation of the drug. The Committee of Safety of Medicines in the UK reviewed the evidence in 2004 and concluded, “there is no clear evidence that the SSRIs and related antidepressants have a significant dependence liability or show development of a dependence syndrome according to internationally accepted criteria”.
Suicidal feelings with SSRIs in younger people
There is some evidence of increased suicidal thoughts (although not actual suicidal acts) and other side-effects in young people taking antidepressants. However, NICE in the UK has stated that fluoxetine, an SSRI antidepressant, can be used in under-18s. There is no clear evidence of an increased risk of self-harm and suicidal thoughts in adults of 18 years or over. Young adults are more likely to take their own lives than older adults, so a young adult should be particularly closely monitored if he or she takes an SSRI antidepressant.
How long do they need to be taken for?
Studies show that if antidepressants are stopped within eight or nine months, the symptoms of depression are more likely to come back. The current recommendation is that it is best to take antidepressants for at least six months after the patient starts to feel better. In patients who have had two or more attacks of depression, then treatment should be continued for at least two years.
Antidepressants during pregnancy
The benefits of antidepressants sometimes outweigh the risks during pregnancy. Non-drug methods such as Cognitive Behavioural Therapy should be tried before drugs in pregnancy. If medication is needed, for example in cases of suicidal feelings, SSRIs are the most commonly prescribed. Tricyclics are best avoided in pregnancy.
Antidepressants in breastfeeding mothers
A baby will get only a small amount of antidepressant from mother’s milk. Babies older than a few weeks have very effective kidneys and livers. They are able to break down and get rid of medicines just as adults do, so the risk to the baby is very small.
Important points when taking antidepressants
- They should be taken every day, otherwise they will not work.
- After commencing, it will take one-to-two weeks to start working and maybe up to six weeks for full effect.
- With some of the older tricyclic drugs, it’s best to start on a lower dose and work upwards over a few weeks.
- The dose of SSRI antidepressant generally does not have to be increased slowly. The dose the patient starts with is usually the dose they carry on with.
- It doesn’t help to increase the dose above the recommended levels.
- Many patients are put off by the initial side-effects, such as nausea. Many of them wear-off in a few days. They should not be stopped unless the side-effects are very severe.
- Persevere — stopping too early is the commonest reason for people not getting better and for the depression to return.
- The doctor should be informed about any major changes in mood when the dose of antidepressant is changed.
- Alcohol should be taken in moderation only. Alcohol on its own can make depression worse, but it can also make patients slow and drowsy when taking antidepressants.
Part 2: Medication used for anxiety
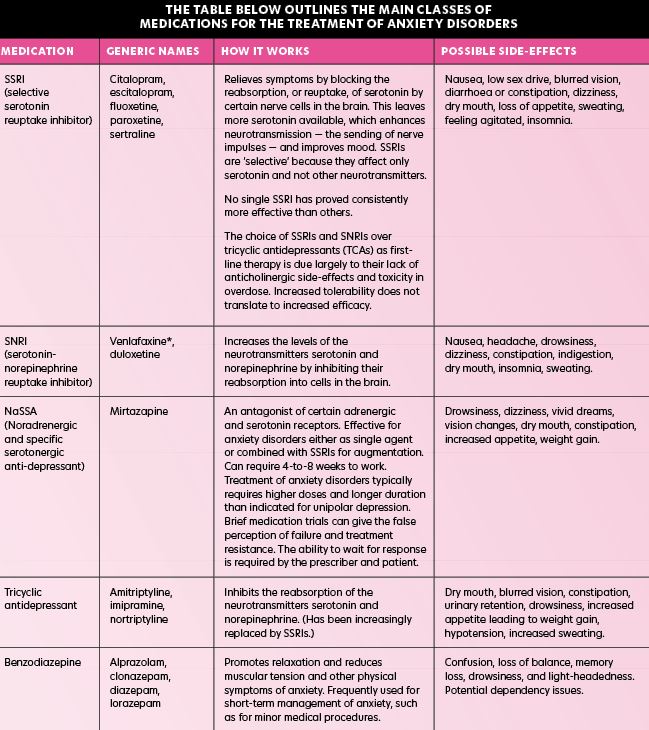
Anxiolytics
Anxiolytic medications are the second set of medication for treatment of acute anxiety, with antidepressants being the first set. These medicines abort current symptoms of anxiety and do little to prevent symptom recurrence. Anxiolytics can be divided into benzodiazepines and non-benzodiazepines. Benzodiazepines are frequently thought of as the classic anxiolytic. This class of medication provides a wide range of choices in terms of onset of action, half-life, and the presence of an active metabolite. There are no specific recommendations in terms of use of one benzodiazepine over another in the treatment of anxiety disorders.
In general terms, benzodiazepines with shorter half-lives and more rapid onset of action are more likely to lead to rebound anxiety when the effects of the medication wane, leading to a need to take more of the medication. If possible, longer-acting benzodiazepines (ie, clonazepam) should be used in conjunction with antidepressants, when the prescriber needs to decrease anxiety acutely, to allow for treatment engagement, and/or treat symptoms that are threatening patient safety.
If possible, treatment should be limited in duration and stopped once antidepressants lower overall anxiety levels and patients are able to engage in other forms of treatment. Although benzodiazepines are effective, physiological dependence develops in all users, so misuse poses potential problems. Tapering benzodiazepines must be gradual and can be dangerous if completed too abruptly. The withdrawal syndrome that accompanies benzodiazepine cessation closely parallels that of alcohol withdrawal.
The mildest form is rebound anxiety that can be seen with reducing or missing doses and is most common with short-acting benzodiazepines (ie, alprazolam). In rare cases, severe withdrawal symptoms can be seen, which can lead to seizure, coma, and death. Although exact rates of risk are unknown, severe withdrawal is rare and more likely in patients taking higher doses, for prolonged periods, and for whom the medication is discontinued abruptly. Co-occurring substance use disorder is common and in such situations, treatment with benzodiazepines is contraindicated.
When anxiety needs to be controlled acutely, but benzodiazepines are not indicated, there are other alternatives. The anticholinergic agent hydroxyzine, b-blocker propranolol, gabapentin and pregabalin are effective alternatives as anxiolytics without abuse potential.
Other medications:
Antihistamines
Whilst usually prescribed to treat allergic reactions, some are used to treat anxiety short-term, as they have a calming effect on the brain, helping lessen feelings of anxiety. Hydrazine is the most prescribed for treating anxiety.
Pregabalin
May be offered if SSRI or SNRI are not suitable. Although prescribed for epilepsy, has been found to be beneficial in treating anxiety.
Buspirone
Can help ease psychological symptoms. Belongs to group of medicines known as anxiolytics. Usually taken for at least two weeks before any improvement is noticed. Works in a similar way to benzodiazepines.
Condition-specific medication treatment recommendations
Generalised anxiety disorder (GAD)
Daily SSRI/SNRI. Anxiolytics may be needed as a bridge for severe symptoms until antidepressants provide relief.
Panic disorder (PD)
Daily SSRI/SNRI. Use long-acting anxiolytics because short-acting agents are unlikely to abort panic attacks.
Obsessive-compulsive disorder (OCD)
Daily SSRI/SNRI. Anxiolytics may be needed as a bridge for severe symptoms until antidepressants provide relief.
Social anxiety disorder (SAD)
Daily SSRI/SNRI. Propranolol is useful for public speaking.
Post-traumatic stress disorder (PTSD)
Daily SSRI/SNRI. Anxiolytics may be needed as a bridge for severe symptoms until antidepressants provide relief. Benzodiazepines are generally not recommended.
Part 3: Medication used for schizophrenia
In many cases, people living with schizophrenia do not realise they have a mental illness. They may not think they need help because they believe their delusions or hallucinations are real. Therefore, it is often up to family and friends to seek treatment. Occasionally, people with schizophrenia pose an immediate risk to themselves or others during an acute episode and may need rapid tranquillisation. Tranquillisation with benzodiazepines should only be a temporary measure.
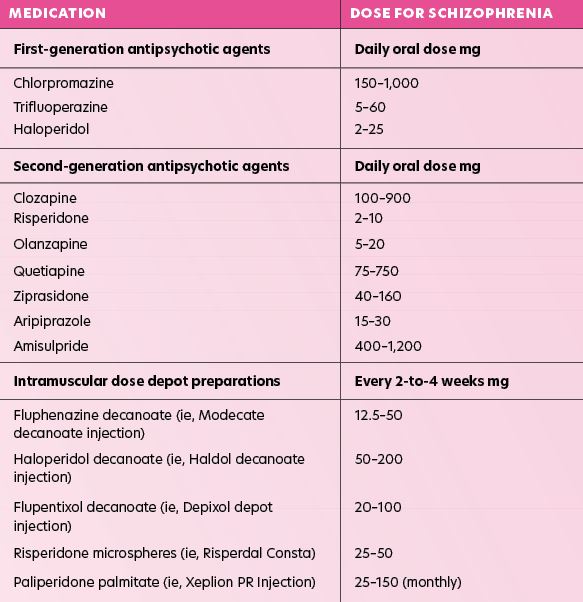
The causes of schizophrenia are still unknown; therefore, treatment focuses on eliminating the symptoms of the disease. Antipsychotics are mainly used to treat schizophrenia. They work by altering the balance of some neurotransmitters in the brain, thus controlling symptoms. Positive symptoms respond well to antipsychotic drugs, however they do not work as well on negative symptoms. Therefore, antipsychotic medication is usually taken on a long-term basis, thus preventing relapses. Antipsychotic drugs are broadly divided into two categories: Typical or atypical antipsychotics.
Older typical antipsychotics
These are sometimes called ‘first-generation’ antipsychotics and were the first type of antipsychotics developed in the 1950s for psychosis, especially schizophrenia. Examples include chlorpromazine, trifluoperazine, haloperidol, flupentixol, zuclopenthixol, and sulpiride. Thirty per cent of patients have a relapse during treatment with first-generation antipsychotic drugs, compared with 80 per cent without treatment.
Newer atypical antipsychotics
These were first introduced in the 1990s and are also known as ‘second-generation’ antipsychotics. Examples are amisulpride, aripiprazole, clozapine, olanzapine, quetiapine, and risperidone. Atypical antipsychotics are often used first-line for newly-diagnosed schizophrenia. This is because they demonstrate good balance between chance of success and the risk of side-effects. However, for people already stabilised on typical antipsychotic, there is no need to change to a newer one.
Depot injections of an antipsychotic drug
In some cases, an injection of a long-acting antipsychotic drug is used once symptoms have eased. The drug from a depot injection is slowly released into the body and is given every two-to-four weeks to prevent relapses. The main advantage is that it prevents the problem of non-compliance. Non-compliance can be a problem with schizophrenia, as the patient often does not realise they have a problem. An American study showed that 74 per cent of patients with schizophrenia discontinued medication within 18 months without consulting with their doctor, leading to relapses. Non-compliance is similar for atypical and typical antipsychotics; therefore, depot injections can be a solution.
There are five FGA depot injections and two SGAs (risperidone (Risperdal Consta) and paliperidone (Xeplion)) available in Ireland as a long-acting injection (LAI).
? Has recently had a heart attack ? Is at risk of having irregular heartbeats (cardiac arrhythmias).
Second-generation long-acting antipsychotic injections
Risperidone injection
Risperidone was the first second-generation LAI to be licensed in the UK and Ireland. The risperidone LAI antipsychotic works in a separate way to the first-generation depot injections. The drug will not reach a therapeutic level for a few weeks after injection; therefore, it is essential that the patient receives alternative antipsychotic medication during the initial period of treatment following the first injection.
Paliperidone injection
Paliperidone injection blocks serotonin 5-HT2 and dopamine D2 receptors. Dopamine and serotonin are neurotransmitters known to be involved in regulating mood and behaviour, amongst other things. Paliperidone is effective in relieving both positive and negative symptoms of schizophrenia, whereas older antipsychotics are usually less effective against the negative symptoms. Paliperidone also relieves ‘affective symptoms’ that are associated with schizophrenia, such as depression, guilt feelings or anxiety. Paliperidone injection is administered into the muscle of the upper arm or buttock, where it forms a reservoir of medicine that is slowly released into the bloodstream. The injection is given once every four weeks.
Patient suitability
Paliperidone LAI has not been shown to be any more efficacious than risperidone long-acting injection, but does have some practical advantages, including the fact that it does not have to be stored in the fridge, it is only administered once-monthly, and comes as a pre-filled syringe, meaning administration is easier and quicker. There are no data on efficacy in prevention of relapse relative to other long-acting injections.
Choice of drug
There are some differences between the various antipsychotic drugs. No one drug can be considered significantly better than the others, however one may be better for one individual than another. For example, some are more sedating than others, so may be suitable for patients who are agitated or cannot sleep. If one does not work so well, a different one is tried until a good response occurs.
A good response to antipsychotic medication occurs in about 70 per cent of cases. Symptoms such as agitation and hallucinations generally ease within a few days of starting medication. Symptoms like delusions usually subside within a few weeks and it can take several weeks for full improvement. Antipsychotic medication is normally continued long-term once symptoms improve. Long-term treatment aims to prevent relapses, or at least limit the number and severity of relapses. There is some evidence that the newer atypical antipsychotics have lower relapse rates than older typical antipsychotics.
Newer atypical antipsychotics have been shown in studies to be more effective at improving cognitive function (including attention, memory, and speech) than older typical antipsychotics. Newer atypical antipsychotics also appear to be more effective than older typical antipsychotics for negative symptoms of schizophrenia.
Clozapine should be tried for patients who have not responded adequately to treatment, despite the use of adequate doses of at least two different antipsychotic drugs. At least one of the drugs should be an atypical antipsychotic before trying clozapine.
Clozapine is very effective for psychotic symptoms, including hallucinations and breaks from reality. Clozapine can sometimes cause a serious condition called agranulocytosis, a loss of the white blood cells, which reduces the ability to fight infection. People who take clozapine must get their white blood cell counts checked weekly for the first 18 weeks and every two weeks after that for the first year and every four weeks thereafter, including the first four weeks after the drug is discontinued.
Other atypical antipsychotics do not cause agranulocytosis. While all antipsychotics lower the threshold for seizures (making an epileptic fit more possible), this effect is more pronounced with clozapine. The risk of agranulocytosis and the cost of blood tests is the main reason that clozapine is generally reserved for when other medication fails, which is estimated to be 30 per cent of cases.
For patients who have only one episode of schizophrenia and who remain symptom-free for two years with treatment, the medication may then be discontinued slowly; the patient should be closely monitored for relapse when medication is being discontinued.
Side-effects of antipsychotics
Side-effects can occur and there is a trade-off between easing symptoms and side-effects from treatment. Different antipsychotic drugs cause different types of side-effects. Sometimes one drug causes side-effects in some people and not in others. Often, two or more different drugs have to be tried before one is found that is best suited.
Anticholinergic side-effects are more common with the older typical antipsychotics and include dry mouth, blurred vision, flushing and constipation. These tend to be worse at the start of treatment and may ease off as the patient gets used to the drug. Chlorpromazine tends to cause skin photosensitivity when exposed to sunlight. Sunscreen must be used if going out in strong sun while taking chlorpromazine.
Drowsiness is also common but may be reduced by reducing the dose. Extrapyramidal side-effects (movement disorders) can occur with typical antipsychotics. These include:
- Parkinson’s-type symptoms, for example, tremor and muscle stiffness.
- Akathisia, which is like a restlessness of the legs (a major cause of non-compliance).
- Dystonia, which is abnormal movements of the face and body.
- Tardive dyskinesia, which is a movement disorder that can occur with longer-term treatment with antipsychotics. It causes rhythm-like, involuntary movements. Tardive dyskinesia most commonly affects the mouth and can include lip-smacking, grimacing and tongue-rotating movements, although it can affect the arms and legs too.
About 30 per cent of people treated with typical antipsychotics long-term eventually develop tardive dyskinesia. Nowadays, people are closely monitored for symptoms of tardive dyskinesia and the drug is changed once the symptoms start to develop. If movement disorders are a problem, then other drugs may be used to try to counteract them. These include anticholinergic drugs such as biperiden (Akineton). Tardive dyskinesia will not respond to treatment with anticholinergic drugs but usually resolves slowly after discontinuation of the typical antipsychotic. However, it is irreversible in some cases. Propranolol (20-to-80mg daily) can be used to control akathisia.
Atypical antipsychotic drugs are less likely to cause movement disorder side-effects than typical antipsychotic drugs. This reduced incidence of movement disorders is the main reason why an atypical antipsychotic drug frequently is the first choice for treatment.
Atypical antipsychotics do have their own risks, particularly the risk of weight gain. Weight gain can occur, and this may increase the risk of developing diabetes and heart problems (due to raised cholesterol) in the longer term, thus blood sugars and cholesterol levels should be monitored regularly. Weight gain appears to be a particular problem with clozapine and olanzapine. For example, trials show that olanzapine can cause weight gain of 5.4kg within five weeks of treatment and weight gain of 20kg or more after longer-term treatment. Ziprasidone and amisulpride tend to cause less weight gain than other atypical antipsychotics. Atypical antipsychotic drugs can sometimes have the tendency to cause obsessive compulsive symptoms.
Use of antidepressants in schizophrenia
Antidepressants may be used in some cases, especially for patients primarily showing negative symptoms. Research suggests that taking an antidepressant drug in addition to an antipsychotic drug may be better than an antipsychotic drug alone in treating negative symptoms of schizophrenia. An antidepressant drug may also be useful to treat depression, which is common in people with schizophrenia. Patients who display manic episodes, including excitement and agitation, may benefit from mood stabilisers such as lithium carbonate or sodium valproate.
Outlook (prognosis) for schizophrenia patients
- In most cases, there are recurring episodes of symptoms (relapses). Most people live relatively independently, with varying amounts of support. The frequency and duration of each relapse can vary. Some people recover completely between relapses. Some people improve between relapses but never quite fully recover. Treatment often prevents relapses or limits their number and severity.
- In some case (approximately two-in-10 cases), there is only one episode of symptoms that only lasts a few weeks. This is followed by a complete recovery without any further relapses.
- For up to about 20 per cent of people with schizophrenia, medication is not very effective at controlling symptoms and they need long-term dependent care. For some, this is in secure accommodation.
- Depression is a common complication of schizophrenia.
- It is thought that up to a third of people with schizophrenia abuse alcohol and/or illegal drugs. This can make treatment more challenging.
- About one-in-10 people with schizophrenia take their own life.
The outlook is thought to be better if:
- Treatment is started soon after symptoms begin.
- Symptoms develop quickly over several weeks, rather than slowly over several months.
- The main symptoms are positive symptoms rather than negative symptoms.
- The condition develops in a relatively older person (aged over 25).
- Medication is taken as advised.
- There is good family and social support, which reduces anxiety and stress.
- Abuse of illegal drugs or alcohol does not occur.
Newer drugs and better psychological treatments mean that prognosis is now better than it was in the past. ?
References: Available upon request
Disclaimer: Brands mentioned in this article are meant as examples only and not meant as preference to other brands.







