Testicular cancer (TC) represents 1 per cent of male cancers and 5 per cent of urological cancers; its incidence has increased in the past few years, especially in Western and industrialised countries.
TC is a rare disease, accounting for 1 per cent of male cancers and 5 per cent of urological cancers worldwide.1 It is, however, the most common cancer found in young men aged between 15 and 34 years, and approximately 173 men are diagnosed with testicular cancer in Ireland each year.7
Mortality associated with testicular cancer is relatively low at approximately 0.1 per cent of all annual cancers, and cure rates are greater than 90 per cent for all stages, with over 95 per cent five-year survival rates.1,9
The incidence of TC has increased in Western and industrialised countries in recent years, possibly due to an increased exposure to aetiological factors. The highest incidence of testicular cancer is observed in Western and Northern Europe at 8.7 and 7.2 per 100,000 men, respectively.9
Testicular cancer includes several types of cancer, such as germ cell tumours (GCT), sex cord-gonadal stromal tumours, and secondary testicular tumours. About 90-to- 95 per cent of testicular tumours arise from germ cells to generate the GCT, followed by 5-to-10 per cent gonadal stromal tumour, mixed GCT and secondary tumours.2
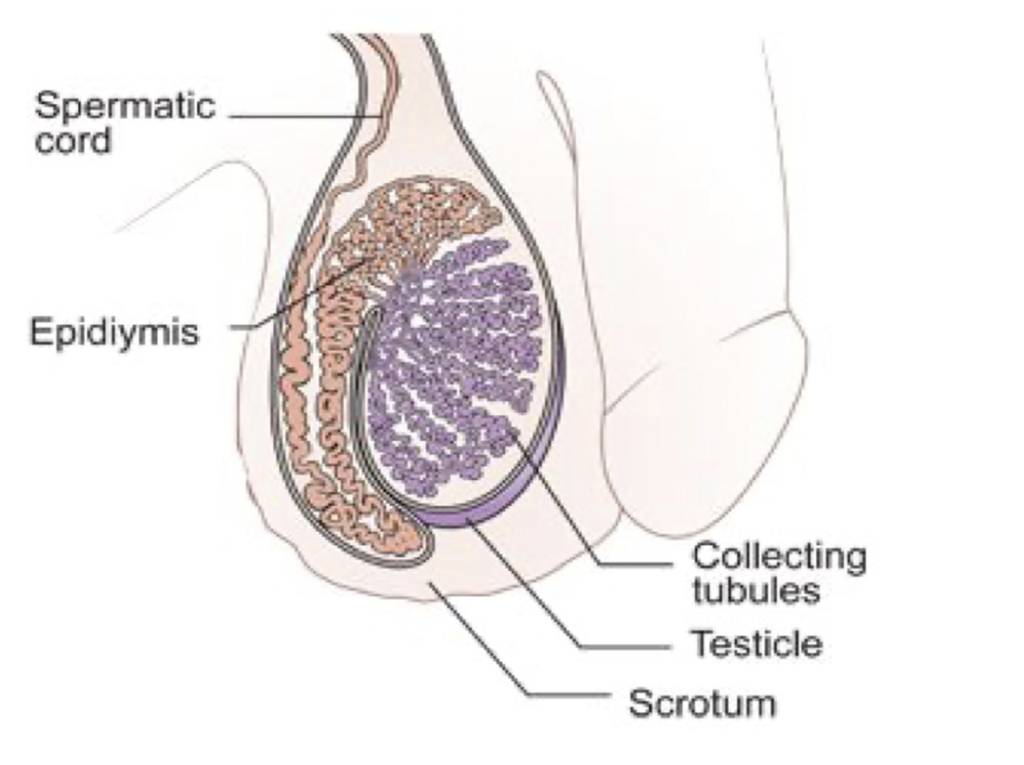
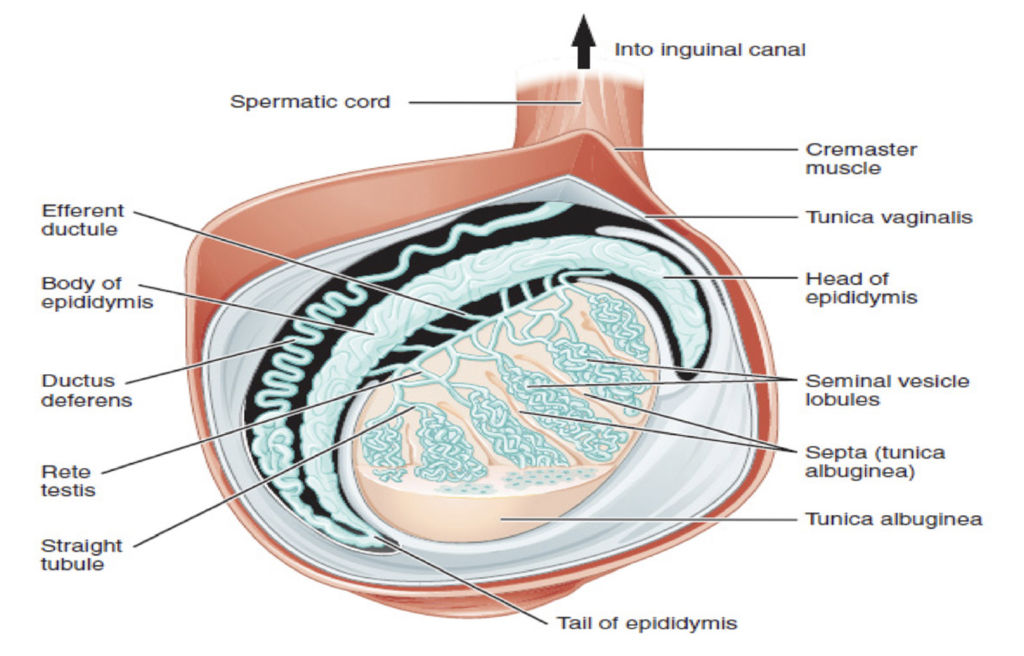
ANATOMY AND PHYSIOLOGY OF THE TESTES
The testes (male gonads) are located in a skin-covered, highly pigmented, muscular sack called the scrotum that extends from the body behind the penis. They produce both sperm and androgens, such as testosterone, and are active throughout the reproductive lifespan of the male. Paired ovals, the testes are approximately 4-to-5cm in length and are surrounded by two distinct layers of protective connective tissue. The outer tunica vaginalis is a serous membrane that has both a parietal and a thin visceral layer. Beneath the tunica vaginalis is the tunica albuginea, a tough, white, dense connective tissue layer covering the testis which also inverts to form septa that divide the testis into 300- to-400 structures called lobules. Within the lobules, sperm develop in structures called seminiferous tubules.8
RISK FACTORS
The main non-modifiable risk factors for testicular cancer are cryptorchidism (undescended testicle), family history, previous history of testicular cancer, genetic predisposition, ethnicity, congenital abnormalities and infertility.2
In cryptorchidism, the undescended testicle remains in the abdomen or groin, and the risk of developing the disease does not change even after surgery to move the testicle into the scrotum. In patients with cryptorchidism, the relative risk of developing testicular cancer ranges from 2.9 to 6.3. The risk is increased in both testes, although the risk is much higher in the ipsilateral testis (6.3 vs 1.7).5 Family history correlates to an increased risk and testicular cancer risk is significant in men whose father or brother had the disease. Patients with a father or brother with testicular cancer have a 3.8 and 8.6 times greater risk, respectively.5
Those diagnosed with cancer in one testicle are also more likely to get cancer in the other testicle. Patients with a personal history of TC have a 12-times greater risk of developing a contralateral testicular cancer than the general population. However, the greatest risk is in the first five years after diagnosis, and the 15-year cumulative risk is 1.9 per cent.5
Genetic and environmental factors play an important role in the genesis and development of testicular cancer. Several genes are implicated in its pathogenesis and different environmental factors have been investigated.1 Klinefelter’s syndrome, caused by a chromosomal abnormality, has been associated with testicular cancer and other cancer types, and congenital abnormalities of the testicles, penis or kidneys may also contribute to an increased risk of testicular cancer. Age represents one of the most frequent factors of testicular cancer occurrence and the highest incidence of GCT has been found in men between 15 and 35 years of age. Infertility is also strongly associated with testicular cancer. Caucasian men have a higher chance of getting the disease than Afro-Caribbean or Asian men.1,3
SYMPTOMS
TC may present as a painless scrotal mass, an incidental radiologic finding, post-traumatic symptom, or scrotal pain.5 An enlarged testicle or a small lump or area of hardness are usually the first signs of testicular cancer. Any lump, enlargement, hardness, pain, or tenderness in the testicle should be evaluated as soon as possible. Other symptoms of testicular cancer usually do not appear until after the cancer has spread to other parts of the body. Symptoms of testicular cancer may include:
- A painless lump or swelling on either testicle. Found early, a testicular tumour may be about the size of a pea or a marble, but it can grow much larger.
- Pain, discomfort, or numbness in a testicle or the scrotum, with or without swelling.
- Change in the way a testicle feels or a feeling of heaviness in the scrotum. For example, one testicle may become firmer than the other or testicular cancer may cause the testicle to grow bigger or to become smaller.
- Dull ache in the lower abdomen or groin.
- Sudden build-up of fluid in the scrotum.
- Although rare, some testicular tumours make hormones that cause gynaecomastia.
- Lower back pain, shortness of breath, chest pain, and bloody sputum or phlegm can be symptoms of later-stage testicular cancer.
- Swelling of one or both legs or shortness of breath from a blood clot can be symptoms of testicular cancer.
When cancer spreads to other sites such as the lungs, brain, abdomen or neck, symptoms including nausea, vomiting, gastric upset, cough, shortness of breath, weakness, sensory disturbances, abdominal pain, lumps in the neck/groin areas, and back pain, can occur. Prompt evaluation is important to ensure early diagnosis and treatment and decrease the burden of treatment in advanced disease.9
Testicular cancers are defined based on their cell type. The most common histology of testicular cancer is germinal-seminoma and non-seminoma. About 95 per cent of testicular cancers begin in germ cells, specialised cells in the testicles that make sperm. While these tumours typically start in the testicles, they also occasionally arise in the abdomen, chest, or other areas of the body, even if there is no evidence of cancer in or near the testicles. Seminomas make up about half of all germ cell tumours. They usually grow slowly and are less likely to metastasise to other parts of the body. Non-seminomas are often more aggressive than seminomas, and are more likely to spread beyond the testicle. Approximately 5 per cent of testicular cancers start in stromal cells, which make testosterone. Testicular stromal tumours are often benign.3
DIAGNOSIS
Evaluation by clinicians is guided by a complete history of the presenting symptoms, physical examination and assessment for risk factors. Testicular examination should include the affected and unaffected testis for comparison. The normal testis is 3.5-5cm in length, smooth, homogenous, movable and detached from the epididymis. Hard, firm, or fixed areas within or adjacent to the testes are abnormal and warrant further investigation. Physical examination should also include evaluation of the inguinal and supra-clavicular lymph nodes, the abdomen, and the chest for gynaecomastia.5 It is important to ask specifically about the history of cryptorchidism, orchiopexy, or inguinal hernia repair as an infant. A family history of testicular cancer in the father or a brother should be elicited. Physical examination findings of any solid intra-testicular mass should be considered to be testicular cancer until proven otherwise.9
Many signs and symptoms of testicular cancer are similar to those caused by non-cancerous conditions such as a spermatocele, varicocele, hydrocele, inguinal hernia, lymphoma, epididymo-orchitis or epididymitis, and differential diagnosis is important.4
Blood tumour markers include alpha-fetoprotein (AFP), beta human chorionic gonadotrophin (bHCG) and Lactate dehydrogenase (LDH).6
Scrotal ultrasonography can confirm the presence of a mass, and has a sensitivity of 92-to-98 per cent and specificity of 95-to-99.8 per cent.5
Once a solid intra-testicular tumour is identified, radical inguinal orchiectomy is performed both for diagnostic and therapeutic purposes.12 A biopsy of the suspect mass will be carried out and when suspicion for metastatic disease is present, additional imaging with CT of the chest and abdomen may be done for staging.5 Staging is determined by the size of the tumour, lymph node involvement, whether the cancer has spread, and if tumour markers are present.10 Tumour staging guides further management with options including active surveillance, chemotherapy, retroperitoneal lymph node dissection, and radiation therapy.9
STAGING11,12
Stages are based on four categories:
T (Tumour): This describes whether the tumour has spread to tissues near the testicle.
N (Node): Indicates whether the testicular cancer cells have spread to regional lymph nodes.
M (Metastasis): This refers to whether the cancer has metastasised.
S (Serum): This indicates the level of tumour marker proteins in the serum, or blood.
Once the individual T, N, M and S components are scored, they are combined to determine the overall testicular cancer stage group. The stages of testicular cancer are:
Stage 0: The cancer cells have not spread beyond the testicle. At this stage, tumours are also referred to as carcinomas in situ.
Stage 1 testicular cancer: The cancer has invaded tissues next to the testicle, but has not spread to lymph nodes, or more distant sites in the body. Levels of tumour marker proteins may be normal or elevated. The three subcategories of stage 1 testicular cancer are:
- Stage 1A: The tumour may have grown through the inner layer of tissue surrounding the testicle, but not the outer layer, and it has not spread to blood or lymph vessels. Serum levels of tumour markers are normal.
- Stage 1B: Tumours at this stage may have spread to blood or lymph vessels or may have invaded the outer layer surrounding the testicle, the spermatic cord or the scrotum. Serum levels of tumour markers are normal.
- Stage 1C: These cancers can demonstrate any degree of invasion of nearby tissues, and levels of tumour markers measured after the tumour has been removed by surgery are elevated.
Stage 2 testicular cancer: Testicular cancers at this stage have invaded tissues next to the testicle and can now be found in at least one nearby lymph node. Tumour marker levels may be normal or slightly elevated. Stage 2 testicular cancer has three subcategories:
- Stage 2A: Tumours at this stage have spread to one or more lymph nodes, but no node is larger than 2cm.
- Stage 2B: Tumours at this stage have spread to at least one lymph node, which is between 2-5cm in size.
- Stage 2C: These tumours have spread to at least one lymph node larger than 5cm.
Stage 3 testicular cancer: Testicular cancers at this stage have spread to distant lymph nodes or organs. Stage 3 testicular cancer has three subcategories:
- Stage 3A: These cancers have spread to a distant lymph node or the lungs. Tumour marker protein levels are normal or slightly elevated.
- Stage 3B: At this stage of testicular cancer, patients have moderately elevated levels of tumour marker proteins, and the disease has either spread to nearby or distant lymph nodes, or the lungs.
- Stage 3C: These cancers have high levels of tumour marker proteins and may have spread to nearby or distant lymph nodes, or the lungs. Alternatively, they may have spread to other distant organs, such as the liver or the brain, but in this case serum tumour markers can be at any level.
TREATMENT AND PROGNOSIS
Treatment options for TC include surgery, radiation therapy, chemotherapy and stem cell transplant. Sometimes more than one type of treatment might be used, including chemotherapy and/or radiotherapy.9
The management of seminomas depends on the extent of spread of the cancer. Surgery, radiotherapy and chemotherapy are used to treat seminomas and the stage of cancer will decide treatment options. Non-seminomas are usually treated with surgery and chemotherapy.10
When a diagnosis of testicular cancer is suspected based on physical examination and ultrasound findings, radical inguinal orchiectomy is performed, which removes the testicle, epididymis, and spermatic cord up to the level of the internal inguinal ring. In this procedure, these structures are delivered through an inguinal incision made along Langer’s lines in the groin. If the mass is too large to pass through a standard 3-to-5cm inguinal incision, the incision can be carried inferiorly to the anterior scrotum to allow for removal of the testis in its tunics along with the spermatic cord. Trans-scrotal orchiectomy or biopsy is contraindicated, as doing so alters the lymphatic drainage patterns and impacts further management. Further surgery or radiotherapy or chemotherapy will be based on the disease’s stage and response to the initial management.9
Following radical inguinal orchiectomy, patients should avoid heavy lifting and high-impact activities for four weeks and should wear supportive underwear to prevent scrotal swelling or haematoma. Retroperitoneal lymph node dissection is major intra-abdominal surgery, after which dedicated postoperative rehabilitation should be undertaken.9
Removing one testicle does not affect libido or the ability to have an erection, providing the remaining testicle is normal. The removal of a testicle may be traumatic, especially for a young man, and a testicular prosthesis can be placed in the scrotum at the time of surgery. Fertility can be compromised by testicular cancer treatment. However, the potential to father children should not be greatly affected provided the other testicle is normal. Chemotherapy, however, does affect sperm production in this testicle and it is recommended that patients with testicular cancer arrange to freeze sperm in case there are problems with fertility later on.7 Adequate counselling should be given regarding the possibility of infertility, sperm-banking and also regarding the placement of a testicular prosthesis if required.9
Prognosis is determined by the histology, extent of distant tumour spread, and extent of tumour marker elevations. For men with disseminated seminomas, the main adverse prognostic variable is the presence of metastases to visceral organs other than the lungs. A tumour that originated in the mediastinum has a worse prognosis when compared to a tumour that originated within the testicle.9
PATIENT EDUCATION AND TESTICULAR SELF-EXAMINATION
There is no national screening programme for detecting testicular cancer in Ireland.6 Testicular self-examination is one of the simplest and most effective ways to identify testicular cancer early, although there is controversy about its efficacy.7 Despite opportunities for an early diagnosis, most men seek medical help only after some time has passed, when symptoms have intensified, or after receiving information about the condition from someone else or the media. Despite the fact that knowledge about testicular cancer and testicular self-examination in developed counties is higher, testicular self-examination is still rarely performed. Most patients present with a testicular mass, which suggests that testicular self-examination could aid early detection.1
It is important to educate men of all ages about testicular cancer and testicular self-examination and that healthcare professionals, especially nurses, are well informed and able to discuss it with their patients. Healthcare professionals play a key role in providing information about testicular cancer risk factors and symptoms and in explaining the importance of testicular self-examination. Mortality associated with TC is relatively low at approximately 0.1 per cent of all annual cancer deaths.
TESTICULAR SELF-EXAMINATION7
- Often, the best place to check is in the bath or shower where the scrotum is relaxed and the testicles can be felt easily.
- Hold the scrotum in both hands.
- Use your fingers and a thumb to examine the testicles.
- It is common for one testicle to be slightly larger than the other.
- Gently feel each testicle, one at a time.
- You should be able to feel a soft tube at the top and back of both testicles. This tube, called the epididymis, carries the sperm. It may be slightly tender but do not confuse this with an abnormal lump in the testicles.
- If you notice a lump or anything unusual, contact your GP immediately. The GP will be able to assess and if necessary, refer to a consultant for further investigations.
- Do not be embarrassed or nervous.
- Remember, early detection of the disease is the best chance of a cure.
- TSE should be performed every month.
Men tend to seek help late for testicular problems for many reasons, such as anxiety, and fear of receiving an undesired diagnosis. Others feel ashamed, deprived of their masculinity and are too embarrassed to talk about it with anyone, even a partner. Researchers have found that when men are properly educated about testicular self-examination, they are more likely to carry it out and recognise symptoms of testicular cancer.1
OUTLOOK
Testicular cancer is the most common cancer in men aged 15-to-45 years and represents one of the most common curable malignancies when identified promptly and treated with a multimodal approach.9 It has excellent survival rates and having awareness about the disease and seeking prompt healthcare attention is of utmost importance. Since treatment is successful for most people with testicular cancer, one of the major future goals is to reduce the side-effects of treatment for people with early-stage cancer. In addition, treatments for poor-risk and recurrent cancers are being studied in clinical trials, along with research on the causes and genetics of testicular cancer. Stem cell transplant is most often used to treat testicular cancers that have re-occurred after treatment with chemotherapy. Current studies are looking at whether a stem cell transplant may be valuable as part of the first treatment for some patients with advanced germ cell cancers. Clinical trials are also underway to find better ways of reducing symptoms and side-effects of current TC treatments that can improve patients’ comfort and quality of life.13
References
1. Bresciani M, Boarin M, Facconi L, Manara F, Villa G. Awareness of testicular cancer among young men: A literature review. Int J Urol Nurs. 2020 Jul 17;15(1): 5-11. doi: 10.1111/ijun.12248.
2. Boccellino M, Vanacore D, Zappavigna S, Cavaliere C, Rossetti S, D’Aniello C, et al. Testicular cancer from diagnosis to epigenetic factors. Oncotarget. 2017 Sep 18;8(61):104654-104663. doi: 10.18632/oncotarget.20992.
3. MSK (2021). Testicular Cancer: Germ Cell Tumours. Available at: https://www. mskcc.org/cancer-care/types/testicular-germ-cell-tumors.
4. Cancer.Net (2020). Testicular Cancer: Symptoms and Signs. Available at: https://www.cancer.net/cancer-types/ testicular-cancer/symptoms-and-signs.
5. Baird D, Myers, G, Darnall C, Hu J. Testicular Cancer: Diagnosis and Treatment. Am Fam Physician. 2018 Feb 15; 97(4):261-268. https://www.aafp.org/afp/2018/0215/ p261.html.
6. Irish Cancer Society (2021). Symptoms and Diagnosis of Testicular Cancer. Available at: https://www.cancer.ie/ cancer-information-and-support/cancer-types/testicular-cancer/symptoms-and-diagnosis-of-testicular-cancer.
7. Marie Keating Foundation (2021). Testicular Cancer. Available at: https:// www.mariekeating.ie/cancer-information/ testicular-cancer/.
8. Anatomy and Physiology of the Male Reproductive System. Available at: https://courses.lumenlearning.com/suny-ap2/chapter/anatomy-and-physiology-of-the-male-reproductive-system/.
9. Gaddam, S. (2021). Testicular Cancer. StatPearls: Available at: https:// www.statpearls.com/ArticleLibrary/ viewarticle/29984.
10. St James’s Hospital (2021). Testicular Cancer. Available at: https://www. stjames.ie/cancer/typesofcancer/ testicularcancer/.
11. MacMillan Cancer support (2021). Stages of Testicular Cancer. Available at: https://www.macmillan.org.uk/cancer-information-and-support/testicular-cancer/stages.
12. Markman, M. (2021). Testicular Cancer Stages. Available at: https:// www.cancercenter.com/cancer-types/ testicular-cancer/stages.
13. CancerNet (2020). Testicular Cancer: Latest Research. American Society of Clinical Oncology: ASCO. Available at: https://www.cancer.net/cancer-types/ testicular-cancer/latest-research.







