Dr Donna Cosgrove PhD MPSI looks at the clinical considerations in treating coughs and colds in the community pharmacy
The common cold is probably the most widespread illness known: It is typically an acute, self-limiting infection of the upper respiratory tract caused by viruses. The most common cold-causing virus is the rhinovirus — 30-to-50 per cent of cases — and the coronavirus can cause up to 15 per cent of cases, although infection with over 200 viruses can result in the common cold.1,2
The symptoms of the common cold usually manifest between 24-to-48 hours after exposure but the incubation period, the period between exposure to an infection and the appearance of the first symptoms, can vary widely between viruses. For rhinoviruses, the incubation period is eight-to-12 hours. Symptoms worsen rapidly, and include nasal congestion, fatigue, and low-grade fever, and peak about two-to-three days after infection. Sneezing, sore throat and headache may be present, and a cough may occur, usually starting on the fourth or fifth day. Infections with the rhinovirus typically start with a ‘scratchy’ throat, followed by nasal congestion and discharge, sneezing and cough. Fever is common in children infected with the rhinovirus but is not frequently observed in adults.
The risk for common cold may be increased by factors like stress and lack of sleep. It occurs more frequently in younger people: Children have colds on average up to six or eight times a year, adults up to 60 years of age have about two-to-four colds per year, and individuals aged over 60 years only one cold per year. Common cold occurrence is clearly associated with the seasons, with increased incidence in autumn, peaking in winter and decreasing again in spring time.1,2 Patients with diseases including asthma, COPD and pneumonia may be at higher risk for complications as a result of the common cold, but in most cases the cold does not cause serious illness. Although symptoms of the common cold can last for up to three weeks, generally, they do not persist for more than a week or 10 days. It is impactful economically as the top cause of work and school absenteeism during the winter months. There is no cure, but many people seek out symptomatic treatment, leading to a multi-billion euro yearly expenditure on cough and cold treatment products.1
The common cold can frequently be mistaken for the flu, caused by the influenza virus. Influenza types A and B affect humans, with A causing more severe symptoms. Influenza is responsible for much worse symptoms than the common cold, with similar symptoms to the common cold but additional ones also, such as higher temperatures, chills, headaches, and myalgia.
There is no cure for the cold, but people can try a number of medications for symptomatic treatment. For suitable patients, there are a wide range of products available, including decongestants, antihistamines, expectorants, antitussives, and analgesic/antipyretic medications.1
OTC preparations
Most over-the-counter cough preparations are generally well tolerated and do not lead to serious adverse effects. It is unclear, however, whether over-the-counter cough preparations are helpful in acute cough.3 For children under six years, there is limited evidence of any significant benefit from treatment with many pharmacological OTC remedies for the common cold. Vicks VapoRub (camphor, menthol, and eucalyptus oils in a petroleum base) was rated highly by parents in a study of the treatment of nocturnal cough, congestion, and sleep difficulty caused by upper respiratory tract infection in children.4
The combination of antihistamine-decongestant was found in one review to be the most effective in adults, but many people experience adverse effects such as drowsiness, dry mouth, insomnia and dizziness. It is unclear if this is due more to one particular ingredient or the combination together due to the scarcity of published data examining this.2
Decongestants cause vasoconstriction via adrenergic agonism, resulting in decreased mucosal oedema and a decrease in congestion. These include pseudoephedrine and phenylephrine, and in topical nasal spray products, oxymetazoline. In clinical studies, oral pseudoephedrine appears more effective for nasal decongestion than phenylephrine. In a trial evaluating the effects of oxymetazoline, administration resulted in decreased symptoms of nasal congestion within one hour of use and lasted for up to seven hours. Prolonged use, however, should be avoided (no more than seven days) due to the risk of rhinitis medicamentosa (rebound congestion). This class of drugs is relatively safe when used appropriately but they are associated with a range of adverse effects due to adrenergic stimulation and CNS stimulation: Most commonly, increased blood pressure, tachycardia, palpitations, anxiety, arrhythmias, and urinary dysfunction.1 As a result, decongestants are not suitable in patients with heart disease, hypertension, thyroid disease, diabetes or benign prostatic hyperplasia.
Stimulation of nasal decongestants of the alpha-1 adrenergic receptors on vascular smooth muscle causes vasoconstriction, increasing blood pressure.5 The bioavailability of phenylephrine is increased with coadministration of paracetamol, which poses a potential risk due to many available cold remedies containing this combination. There appears to be a dose-dependent relationship between pseudoephedrine and blood pressure, and heart rate. Administration in individuals with normal blood pressure caused a 0.99mmHg increase in systolic blood pressure, compared to a 1.20mmHg increase in hypertensive patients. Studies have suggested the development of tolerance to this phenomenon: When the association was evaluated over a longer period, there was less of an effect of pseudoephedrine on blood pressure and heart rate observed.4 Evidence suggests that standard doses of pseudoephedrine in those with well-controlled hypertension have no significant effect on blood pressure, although their use is still not recommended by the manufacturers for people with hypertension.
Antihistamines
Antihistamines can also be considered for symptomatic treatment of rhinorrhoea, watery eyes and sneezing.1,2 Brompheniramine and chlorpheniramine are more useful for this than the second-generation antihistamines, which do not cross the blood-brain barrier.
The first-generation antihistamine action on histaminic and muscarinic receptors in the medulla appears to be responsible for these effects. Due to the histaminergic CNS effects, frequent side-effects include drowsiness and fatigue. Adverse effects from first-generation antihistamines caused by anticholinergic effects include dry eye and mydriasis, urinary retention and constipation. When recommending these medications to treat cold symptoms, it is important to be aware of the impact of certain side-effects on certain population groups, ie, those who may be more impacted or affected by impaired mental alertness. They should also be avoided in benign prostatic hyperplasia and glaucoma.1
Cough treatments
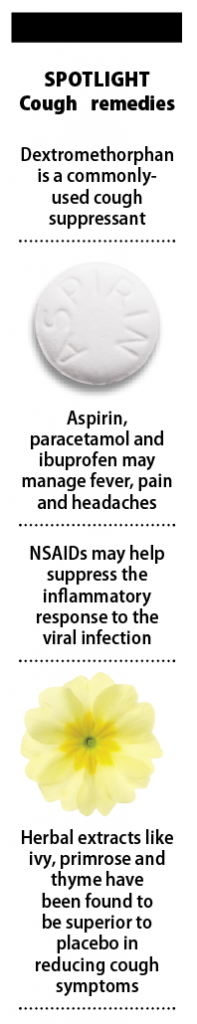
Dextromethorphan is a commonly-used cough suppressant. One study suggests beneficial effects of the drug in treatment of cough compared to placebo,1,3 however, another study shows no strong evidence for its use. Codeine, also used as a cough suppressant, has not been favoured as an effective treatment by clinical studies.
Expectorants are used with the aim of reducing the viscosity and volume of sputum present. Guaifenesin has been available for many years for this purpose, although firm evidence supporting its efficacy for this indication is difficult to find. Nonetheless, the drug is considered safe and is not linked with and clinically meaningful drug interactions. One trial found that mucolytics such as carbocisteine significantly reduced cough frequency by a risk ratio reduction of 50 per cent, as compared with placebo.6 In children, one trial favoured active treatment with mucolytics over placebo, with a statistically significant benefit for symptom score.3 Herbal extracts like ivy, primrose and thyme have been found to be superior to placebo in reducing cough symptoms.7 Interestingly, it has been suggested that the major benefit of cough syrups in soothing cough is likely due to the properties of the solvent or thickening agent, ie, glycerol, rather than the active ingredients. Glycerol itself has lubricating, demulcent and humectant properties.8
Aspirin, paracetamol and ibuprofen are available as analgesics and antipyretics OTC to manage fever, pain and headache that may present in the common cold. These agents are generally considered equally effective in symptom management, but potential side-effects and risk factors need to be considered when advising patients.1 NSAIDs may help suppress the inflammatory response to the viral infection, and have been shown to reduce the symptoms in rhinovirus infections,2 but are unsuitable for those with active ulcers or those with aspirin allergy.
Preventing the spread of cold viruses is the best way to prevent the spread of colds. Infection is transmitted into the nasal epithelium by airborne droplets and by hands and utensils. The virus attaches to intercellular receptors at the back of the throat, and through various mechanisms causes changes in the nasal mucosa, which are still not fully understood. As no epithelial destruction is observed during a common cold, it has been suggested that symptoms experienced are due to the inflammatory response of the host rather than the direct effect of viruses themselves.2 In order to prevent spread of the common cold, patients should be advised to wash hands frequently with soap, especially before preparing food or eating, to avoid touching the face with unwashed hands, and minimise contact with healthy individuals when a common cold is present.1







