Writing For Irish Pharmacist, Prof Dominic A Hegarty Outlines How Pain Awareness Month This September Is A Crucial Tool To Draw Attention To An Under-Recognised Phenomenon.
Every September since 2001, when the American Chronic Pain Association first led a coalition of groups to highlight the needs of those with living with chronic pain, the spotlight is shone on one of the most common illnesses that effects so many individuals. Every year, the same staggering number of one in every four individuals attending healthcare professionals with chronic pain does not seem to change. Every year, we lament the cost chronic pain has on society.
UNDER-RECOGNISED AND UNDER-TREATED
“Chronic pain is vastly under-recognised, funded, and treated when considering its significant impact on American lives,” so says US Pain Foundation CEO Nicole Hemmenway. In fact, the recently-published report from the US Foundation on Pain (2022) highlights that nearly three-quarters (74 per cent) of the 2,378 respondents had lived with pain for more than 10 years. The most common pain conditions were primarily musculoskeletal in nature: Back pain (67 per cent), arthritis (56 per cent), chronic low back pain (56 per cent), nerve pain or neuropathy (53 per cent), and neck pain (51 per cent).
Over half (52 per cent) said their average pain level is 7 or more on a scale of 1-10. Ninety-five per cent of respondents had at least one comorbidity, and almost all reported that pain restricted their ability to engage in routine activities, like exercise, household chores, sleeping, and socialising. The majority (60 per cent) said they feel anxiety-like symptoms daily or a few times a week, and a similar portion (59 per cent) feel depression-like symptoms daily or a few times a week. Closer to home, these statistics reflect a similar pattern in the Irish healthcare service.
GLOBAL YEAR OF PAIN 2022
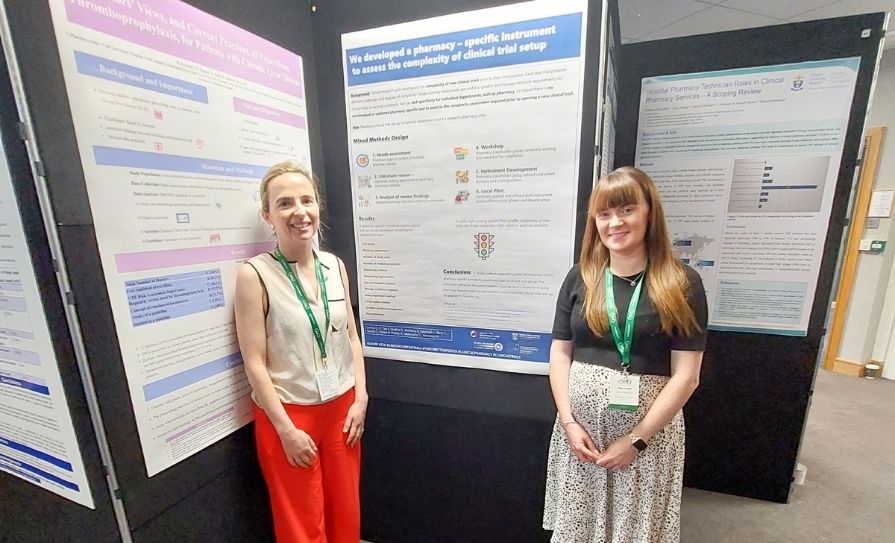
The aim of the IASP 2022 Global Year in Pain is to increase awareness of pain knowledge and how it can benefit those living with pain. The key objective is to increase the awareness of clinicians, scientists, and the public of our accumulating pain knowledge and of how this may be used for the benefit of those living with pain.
How timely it is, especially when the majority of people with chronic pain feel stigmatised by their medical care providers. This was a key finding of a comprehensive survey by the US Pain Foundation. The report identified that people with pain often feel their healthcare providers are not equipped to manage their pain effectively. Over two-thirds (69 per cent) either did not feel, or only ‘rarely’ or ‘sometimes’ felt, that their provider was on a team with them.
TREATMENTS THAT HELP — AND BARRIERS TO ACCESS
The value of multidisciplinary (MDT) approaches in pain management are well recognised. The same resources are not equally available nationally and in some regions, the concept is no more than a long-term ambition. However, not everyone in pain needs access to all aspects of the MDT.
For example, the top strategies used in MDT include activity restriction or modification (73 per cent), stress reduction techniques (42 per cent), heat therapy (41 per cent), and meditation and mindfulness (40 per cent). In fact, activity restriction or modification is the most-used specific ‘therapy’ of any kind across all categories, aside from prescription medications as an entire category.
When it comes to medications, a majority (77 per cent) said prescription medications are the most helpful treatment in managing their pain. Access to interventional pain procedures continue to be the ‘Holy Grail’ for many, but with demand outstripping supply, there is an obvious bottle-neck.
In this context, perhaps we should assess individuals on a case-by-case basis to identify the clinical need to maximise outcome and not simply take a ‘one size fits all’ approach, referring individuals into an already-overcrowded healthcare system.
CHANGE IS NEEDED
At present, the physical limits of an already-overburdened and underfunded pain service are evident. For this reason, one must consider all possible options to support individuals. But there is hope. For example, University College Cork recognised that ensuring our graduate doctors appreciate the importance of pain management, and reduce the risk to those with chronic pain of feeling stigmatised by their medical providers, appointed its first Associate Professor in Pain Medicine. Also, Chronic Pain Ireland is once again supporting the Pain Awareness September campaign, and their 2022 theme is ‘Inspiring Pain Freedom’. They inspire and empower people by ensuring they have the knowledge, skills and self-awareness to take control and improve their quality of life.
For certain individuals, part of that healing journey starts with self-management strategies and tools. Chronic Pain Ireland is collaborating with the HSE for Pain Awareness Month and running the Living Well with Chronic Pain Programmes, with several informative talks and webinars throughout this month. By directing some individuals to this pathway, they can be provided with timely and effective support.
FUTURE PLANNING
Pain Awareness Month allows us to recognise the importance of what we can do for our individual patients. It highlights that not enough is being done for the management of chronic pain in Ireland. Clearly, there are ample opportunities for all of us — patient groups, healthcare providers, insurers, and policy-makers — to work together to better serve people with pain and improve pain care for everyone.
References on request
Author : Professor Dominic A Hegarty
BSc, BMedSc, MB, MSc (Pain Management), PhD. FCARSCI, FFPMCAI, FIPP.
Consultant in Pain Management & Neuromodulation, Mater Private Hospital, Cork.
Associate Professor of Pain Medicine, UCC, Ireland. Honorary Consultant Guy’s & St. Thomas’ Hospital, London. Clinical Lead Neuromodulation Research, Tyndall National Institute, UCC.
President Elect World Institute Of Pain (WIP).
Clinical Director, Pain Relief Ireland www.painreliefireland.ie