Two final-year pharmacy students and a senior preceptor in the APPEL programme offer their insights into how Covid-19 has affected their experiential placements
The first half of 2020 has seen unprecedented changes to all aspects of the pharmacy profession. It’s not just pharmacists who have faced a new way of working — pharmacy students have also had to meet the challenge of continuing their education in unexpected circumstances. Writing for Irish Pharmacist, final-year pharmacy students Aoife Ní Mhuircheartaigh (RCSI) and Edel Burton (UCC) and APPEL Senior Preceptor, Barry O’Sullivan MPSI, explain how Covid-19 has impacted on their experiential learning placements.

Aoife’s story
It’s safe to say that I did not expect my final-year experiential learning placement to include delivering pharmacy services through a small Perspex-covered hatch, but during a global pandemic, this is our new norm. The Covid-19 outbreak hasn’t changed what we do in community pharmacy, but rather the way in which we do things. Overall, the decision to insert a hatch was very well received within the community. People understand its role in protecting both patients and staff alike, and in ensuring the continuity of pharmacy services. The hatch allows us to maintain a physical distance from patients and prevents people congregating whilst waiting for prescriptions, as they are encouraged to call back or wait in their cars. We have also introduced a delivery service for our elderly and more vulnerable patients who are cocooning in their homes. We have a dedicated delivery driver, but we all pitch-in to deliver to our neighbours.
Our methods of communicating with patients have changed greatly over the course of the Covid-19 outbreak, especially since the Government lockdown was introduced. Phone calls, texts and emails are replacing the traditional face-to-face conversations for the most part. This is unusual territory for us in community pharmacy, because accessibility is often associated with our role as pharmacists within the healthcare system. It is important to note, despite common misconceptions, that pharmacists are still providing over-the-counter treatment as normal for non-Covid-related illnesses, for example hay fever, which usually occurs at this time of year.
Personally, I have tried to educate patients around hand hygiene and infection control measures and steer people towards reputable sources of information, which is difficult in the era of social media and forwarding chain messages.
Like many other pharmacies, we have adopted a team-based approach, where Team A and B never meet to limit transmission between staff if anyone becomes infected. With reduced staffing levels and a heavier than usual workload, effective time management is more important than ever, something they teach you about in college, but effectively dealing with the workload during a pandemic has been a steep learning curve.
A strategy that has worked well for us is one technician working at night preparing and assembling blister packs, as this is a labour-intensive but non-urgent task that requires space.
During this time of great uncertainty, much of our time is spent sourcing stock and ensuring the delivery of pharmacy services with as little disruption as possible. Measures have been put in place, such as the legalisation of emailed prescriptions, which has greatly facilitated the provision of seamless healthcare. It will be interesting to see what other changes come to pharmacy practice over the coming months and our role in providing vaccination when the time comes.
Edel’s Story
The APPEL Experiential Learning Placement Programme is a period of discovery, development and decisions. The Pharmacy Class of 2020 will forever be known as the first student pharmacists of the five-year integrated Masters Programme. I never thought we would also be known as the student pharmacists of the 2020 Covid-19 pandemic.
I started my journey as a student pharmacist on 6 January this year. My experiential learning placement was a split placement between the Mater Private Cork, and McCauley’s Pharmacy, Mahon Point, Cork. This placement was unique, as the pharmacy serviced the Mater Private Cork. Thus, I had the benefit of experiencing both the community and hospital settings on a weekly basis.
Queues down the shop and out the door, constant requests for hand sanitiser and worried patients seeking reassurance epitomised the effects of Covid-19 on community pharmacy, for me. As a student pharmacist, I strove to follow the example of my pharmacist colleagues, remaining professional and offering reliably-sourced information and advice. It was a time when I had to rely on every skill, behaviour and competency I had learned during my pharmacy education. A time when I had to deliver care, empathy and understanding as always, but at a distance.
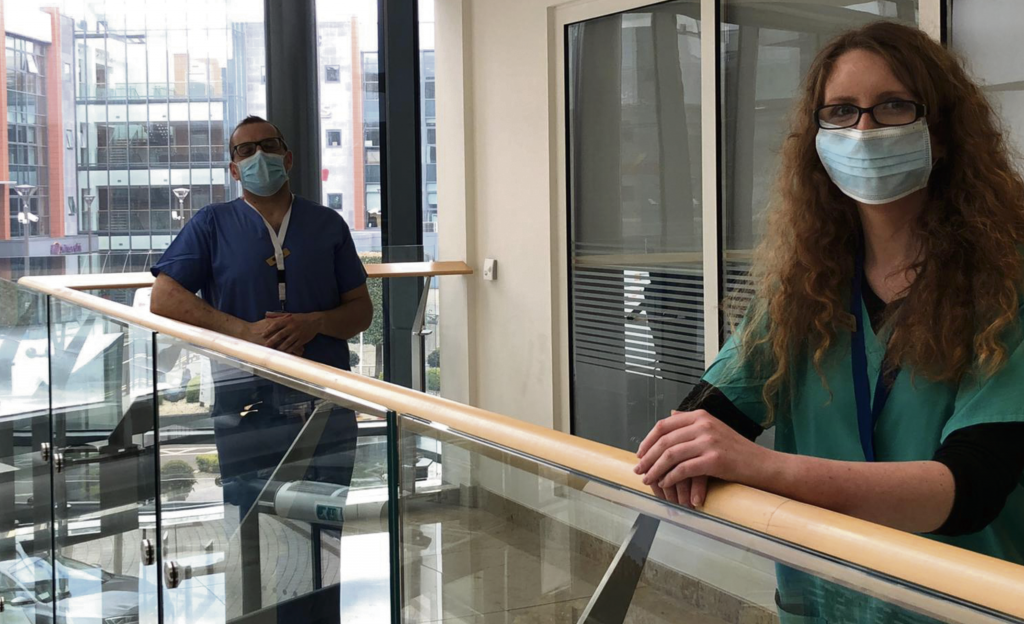
As of 30 March 2020, the Mater Private Cork opened its own Pharmacy Department. So, my experience of Covid-19 is now only from a hospital perspective. I now wear scrubs and a mask each day on placement, I am in different locations to some of my pharmacy colleagues, and I avoid restricted areas of the hospital. I no longer interact with patients; I fill out a Covid-19 screening form each morning upon entering the hospital and have been trained in the donning and doffing of personal protective equipment. A lot has changed in how we practice in the last few weeks. However, the Core Competency Framework hasn’t changed, the Code of Conduct hasn’t changed, and my passion for pharmacy certainly hasn’t changed. Patient-centred care is still at the root of pharmacy. As my Senior Preceptor has taught me well, circumstances might change and you might have to adapt your processes, but the rationale, logic and goal behind them remain constant.
The hospital’s patient profile has changed. Pre-Covid-19, it was an acute hospital with a high turnover, mainly caring for surgical and cardiac inpatients. Now the Mater Private Cork is accepting patients with a range of conditions requiring longer-term care. That has affected the medications we keep and increased our transfers from other hospitals. I am trained in Basic Life Support, have worked with the Nursing Department to put together folders on critical care medicines for each ward, and am currently completing an online course in Critical Care Medications.
Some elements of my daily routine have been removed and replaced by other tasks, due to the current situation. This is a challenging time for our country and the world we live in. As a student pharmacist, it is a challenge, but also a privilege to be able to work in this climate. I have truly seen that regardless of the situation, the health, wellbeing and safety of the patient is always our primary focus.
Barry’s Story
A Senior Preceptor perspective
As a Senior Preceptor, I believe our duty of care to oversee the professional development of the student pharmacist extends past the hours allocated and indeed, past the experiential learning time with them. Senior Preceptors need to ensure we are fostering the next generation of pharmacists to deliver a level of patient care and interdisciplinary support to our fellow healthcare professionals, better than we currently provide. We should always seek to be better at everything we do. Our patients deserve that.
The APPEL placement programme can be a potentially stressful time, away from their peers and familiar surrounds in university; student pharmacists must develop their skills quickly. Adding to this were two significant changes in the planned experiential learning programme for Edel. A change in placement provider and a global pandemic were certainly not in the placement training plan drawn up for Edel.
Like her peers, Edel has been a crucial asset as the pharmacy profession tooled-up for whatever Covid-19 may bring. Apart, but together, in their efforts.
During this time of flux and uncertainty, the Pharmacy Department of the Mater Private Cork was born. The transition period saw a lot of planning and an innumerable number of tasks to be carried out to ensure turbulence between the end of the external contract and commencement of the internal function was kept to a minimum. Edel was central to all this.
Additional to CPD cycles, core competencies and associated study, it was prudent to add one more item to Edel’s daily workload. We called it her ‘decompression time’. Defined down-time each day after work, where she sets aside the notes and tends to her wellbeing. Simple things like a family walk or Zoom with friends can very useful in dissolving the stress of Covid-19, PPE, infection control protocols, and so on.
In some ways, the current crop of student pharmacists are getting a learning experience far more complex than they could have foreseen at the outset; apart but together, they should be proud of their efforts.