Researchers are finalising a solution that homes in on a pain-free method of administering insulin, writes Vittoria D’Alessio
Lee Calladine pricks his skin with a needle up to eight times a day to give himself an injection of insulin – the hormone that keeps his type 1 diabetes in check.
Without insulin, his blood-sugar levels would become dangerously high and eventually fatal.
Game changer
Calladine, aged 54, has been diabetic for 25 years and the insulin top-up routine is so familiar to him
that he’s long past feeling squeamish about piercing his skin. Still, the practice is burdensome.
“I have to rotate where I do my injections,” said Calladine, who lives in the UK city of Portsmouth and works as an event coordinator for the Diabetes Research & Wellness Foundation. “If you inject the same place too often, you damage the tissue and get a lump. And if you then inject into that lump, the insulin won’t get absorbed.”
While a cure for type 1 diabetes is the holy grail, another game changer for Calladine and millions of other people like him around the world would be the ability to deliver insulin without needles or syringes.
That’s where Prof David Fernandez Rivas, a bioengineer at the University of Twente in the Netherlands, believes he can help.
Prof Fernandez Rivas leads a research project that received EU funding to develop a method to deposit liquids into skin and other soft materials using compression rather than needles.
The technique is known as BuBble Gun, which is also the name given to the five-year project that will run until the end of 2024. Fernandez Rivas invented the BuBble Gun with his research team, which is now refining the technology in the hopes of turning it into a reality.
Speedy squeeze
While electronic pumps that release insulin into the body throughout the day do exist, they are imperfect and still require a cannula needle to be inserted at the connection point.
With BuBble Gun, a laser beam is directed at the fluid medicine in a glass cartridge, heating it until it boils and creates a bubble. This bubble grows until it squeezes the liquid at high velocity – 30 to 100 metres a second – out of its tube and, in the case of a medicine, into the skin.
Rather than piercing the skin, the way a needle would, the drug is pushed between skin cells. This limits damage both to the skin and to the cells beneath it.
“The liquid effectively becomes the needle,” says Prof Fernandez Rivas, who moved to the Netherlands from Cuba in 2007 with a first degree in nuclear engineering and has been working in bioengineering and green technology ever since.
This approach could be a relief not just for nine million people worldwide including Calladine who have type 1 diabetes but also for millions of others who have unrelated conditions that also require regular injections.
Other potential beneficiaries are the 25 per cent of people who are scared of needles and who can, as a result, avoid certain medical interventions including vaccination.
“Removing pain and fear from the injection process will have a big impact on a lot of people with needle phobia,” says Prof Fernandez Rivas.
Tissue challenges
Most injections penetrate the body until they reach muscle. These are regarded as the simplest injections to administer and the dose gradually diffuses out of the muscle into the body’s blood-circulation system.
Rather than piercing the skin, the way a needle would, the drug is pushed between skin cells. This limits damage both to the skin and to the cells beneath it
Many drugs, however, can do the job just as well – or perhaps better – when delivered into the more superficial layers of skin.
Fernandez Rivas is confident that many vaccines, for instance, would work just as well when delivered between the layers of the skin. Currently, they tend to be injected into muscle.
This means BuBble Gun has potential uses beyond insulin delivery.
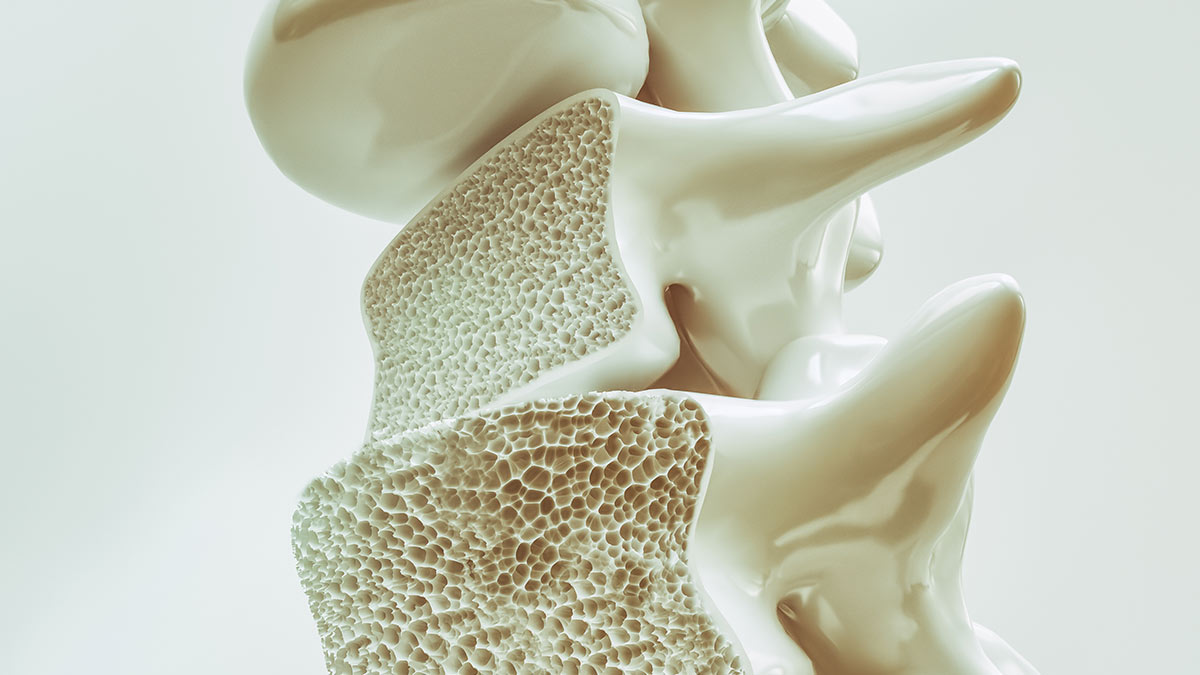
A key technical challenge tackled by the research team relates to skin depth, which varies depending on age, gender, ethnicity, and lifestyle. Smoking, for instance, makes the skin thinner.
As a result, the ‘gun’ pressure needs to be adjusted to take these differences into consideration.
“You need the jet of fluid to penetrate the skin to just the right depth without splashback or seeping into nearby tissue or material, which would alter the dose unpredictably,” says Prof Fernandez Rivas.
The researchers are still working on precisely controlling the drug jet as it enters soft tissue.
Since 2018, they’ve been conducting laboratory experiments on materials that simulate skin as well as on real skin tissue. Tests on human tissue have been in progress since 2022. If all goes well, trials on healthy human volunteers will start later this year.
Planned prototype
The BuBle Gun team has created a start-up company called FlowBeams. Through this, the researchers hope that a prototype of the gun will be ready to showcase to potential industry partners before 2025. Fernandez Rivas foresees a time eventually when diabetes patients will be able to use a modified version that incorporates the microjet technology into a skin patch. The patch would include a sensor that both tests blood-sugar levels on a continual basis and pushes insulin into the body as the need arises. “Imagine how this would transform the life of an anxious parent who wakes up multiple times in the night to check their child with diabetes isn’t having a blood-sugar swing in their sleep,” says Prof Fernandez Rivas. l
This article was written by Vittoria D’Alessio and first appeared in Horizon magazine