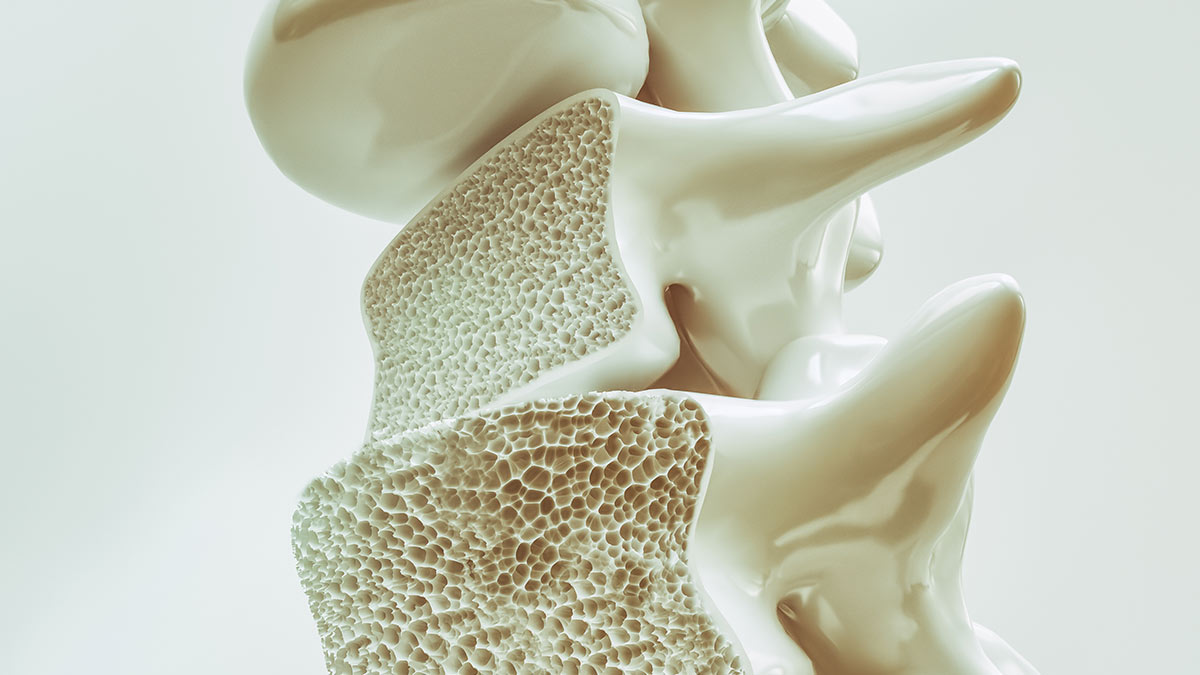
Osteoporosis is a skeletal disorder characterised by low bone mineral density (BMD), leading to an increased risk of fractures. Osteoporosis results from an imbalance between bone formation and resorption, causing a net loss of bone mass. Osteoporosis can often progress without symptoms until a fracture occurs. Osteoporotic fractures lead to a major decrease in quality of life, increasing morbidity, disability and mortality. In Ireland, it is estimated that approximately 300,000 people currently have osteoporosis.
There are several risk factors that increase the likelihood of developing osteoporosis. A gradual decrease in bone density is observed as an individual ages. Female gender is another risk factor, especially in postmenopausal women due to oestrogen deficiency. Other risk factors include being a smoker, low body weight, early menopause, sedentary lifestyle, family history of osteoporosis, excessive alcohol intake, and certain medications, including corticosteroids and anticonvulsants. Diagnosis of osteoporosis is based on BMD measurements, using dual-energy x-ray absorptiometry (DXA) scans. Osteopaenia is defined as a BMD T-score between 1 and 2.5, with a score below 2.5 reflecting osteoporosis. Fracture Risk Assessment Tool (FRAX) is a validated risk assessment tool for osteoporosis. This provides a 10-year probability of a major fracture and is useful in determining patients with osteopaenia that require intervention.
Treatment
The primary objective of osteoporosis is to preserve bone density, prevent fractures and improve overall bone health. Lifestyle modifications are very important in the management of osteoporosis. Increasing weight-bearing exercises, including walking, jogging and resistance training, help to maintain bone density. Treatment should be offered to help smoking cessation and to reduce alcohol consumption. Fall prevention strategies should also be considered for higher-risk individuals.
Adequate levels of calcium and vitamin D are required to maintain bone density. Therefore, calcium and vitamin D supplementation is recommended for individuals with a low dietary intake to raise these to normal levels. Excessive calcium intake is associated with an increased risk of cardiovascular events and supplementation should be individualised for patients.
Pharmacological interventions are the cornerstone of osteoporosis management. Bisphosphonates are the most prescribed drugs to treat osteoporosis. They exert their mechanism of action by inhibiting osteoclast activity. This decreases bone resorption and therefore reduces loss of bone density. Bisphosphonates are indicated for treatment of osteoporosis in postmenopausal women and men at high risk of fractures. Oral bisphosphonates can cause stomach upset and erosion of the oesophagus, which can be reduced by remaining seated upright or standing 30-to-60 minutes after administration. Patients who have been on bisphosphonates for more than five years should be assessed due to an increased risk of femoral fractures and osteonecrosis of the jaw. Examples of bisphosphonates include alendronate, risedronate, ibandronate and zoledronic acid. Alendronate is generally a 70mg tablet administered once-weekly, risedronate is a 35mg tablet administered once-weekly, and ibandronate is a 150mg tablet administered once per month. Zoledronic acid is administered as an intravenous infusion once per year.
The primary objective of osteoporosis treatment is to preserve bone density, prevent fractures and improve overall bone health
Denosumab is a monoclonal antibody that targets the receptor activator of nuclear factor kappa-B (RANK) ligand. This inhibits activity of osteoclasts and therefore prevents loss of bone density, reducing the risk of fractures. It is administered as a 60mg subcutaneous injection every six months. Denosumab is indicated for the treatment of osteoporosis in postmenopausal women that have an increased risk of fractures. Denosumab may not be as effective in the treatment of men, but it is effective in treating bone loss associated with hormone ablation therapy or long-term corticosteroid therapy. The safety and efficacy of denosumab is maintained over 10 years of treatment, with a long-term individualised osteoporosis management plan recommended to ensure treatment is not stopped or delayed without involvement of a healthcare professional. Hypocalcaemia is an adverse effect that is more likely in patients with renal impairment, which should be monitored.
Teriparatide is a synthetic form of parathyroid hormone that stimulates bone formation by osteoblasts. It is a High-Tech medication in Ireland and is supplied on the High-Tech Scheme. Teriparatide is indicated for patients with severe osteoporosis or those who can’t tolerate other treatment options. It is administered as a 20mcg subcutaneous injection daily for 24 months. The patient should have a repeat DXA scan and a new treatment plan implemented. Parathyroid hormone levels, serum and urinary calcium, vitamin D level and renal function should be investigated before commencing teriparatide treatment.
Selective oestrogen receptor modulators (SERMs) work by mimicking the effect of oestrogen on bone tissue, which promotes bone formation and reduces bone resorption. It is approved for the prevention and treatment of osteoporosis in postmenopausal women. Raloxifene is administered orally as a 60mg dose daily. It is associated with a small increase in the risk of venous thromboembolism and therefore should be used with caution in patients with a history of stroke or with risk factors for stroke. Hormone replacement therapy (HRT) is indicated for treating menopausal symptoms in females. Furthermore, HRT can help prevent the relatively rapid loss of bone density in the three-to-five years following menopause.
Role of the pharmacist
Pharmacists play an important role in osteoporosis management, particularly in patient education on osteoporosis and the risk factors. Furthermore, they can counsel on the importance of calcium intake, vitamin D intake and weight-bearing exercise. Through collaboration with other healthcare professionals, pharmacists can help select an appropriate treatment plan for patients. They can also counsel patients on how to optimise medication use, potential adverse effects, and the importance of adherence to medication. Finally, pharmacists can collaborate with other health professionals to ensure continuity of care and effectively manage treatment options to improve clinical outcomes for patients with osteoporosis.
References on request