EAMONN BRADY MPSI PROVIDES AN OVERVIEW OF THE CLINICAL CHARACTERISTICS OF ASTHMA, INCLUDING THE TREATMENT OPTIONS IN THE PHARMACY
A sthma is a long-term condition that can cause a cough, wheezing and breathlessness. The severity of the symptoms varies from person-to-person. In Ireland, respiratory diseases are the third-commonest long-term illness group after cardiovascular and musculoskeletal diseases, with asthma being the second-most common single condition reported after COPD.1
CAUSES
With asthma, the airways become oversensitive and react to stimuli that would normally not cause a problem, such as cold air or dust. Muscles around the wall of the airway tighten-up, making it narrow and difficult for air to flow in and out. The lining of the airways swells, and sticky mucus is produced. This makes it difficult for air
to move in and out. Tightening of muscle around the airways can happen quickly and is the most common cause of mild asthma. The tightening of muscle can be relieved with a reliever inhaler. However, the swelling and build-up of mucus happen more slowly and need a different treatment. This takes longer to clear-up and is a serious
problem in moderate-to-severe asthma.
FACTS ABOUT ASTHMA
The exact cause of asthma is not known. According to the Asthma Insights and Realities in Ireland (AIRI) report in 2002, 470,000 people have asthma in Ireland, meaning approximately one-in-eight of the population suffer from it. Ireland has the fourth-highest prevalence of asthma in the world after Australia, New Zealand, and the UK. The Irish Pharmaceutical Healthcare Association (IPHA) reported there were 600,000 GP consultations for asthma in 1997 and it is likely this figure has risen since.1
There is a strong genetic link. If a parent has asthma, the risk of their child getting it doubles. If both parents have it, it doubles again. And, if one in a family has asthma, the risk of the other children getting it increases, but it is not known by how much. In adults, it is more common in women than men. Asthma can start at any age, but most
commonly starts in childhood. Adult-onset asthma may develop after a respiratory tract infection. In many cases, asthma disappears during teenage years. Many asthma sufferers also suffer from other allergic conditions such
as hay fever, eczema and hives. Asthmatics who also have hay fever find that their symptoms get worse during hay fever symptoms.
In fact, research by allergy UK found that 69 per cent of asthmatics who also had hay fever reported that their symptoms worsened during hay fever season. Asthma has become more common in recent years. The incidence
of asthma among 13- and 14-year-olds has increased by 40 per cent from 1995 to 2003.14 The exact reason for this is not known. Many aspects of modern living, such as changes in housing, diet and a more sterile home environment, may have contributed to the rise in asthma over recent decades. This theory is called the ‘hygiene hypothesis’.
FACTS ABOUT ASTHMA IN CHILDREN
Asthma in children is more common in boys than girls. Children who develop asthma at a very young age are more likely to ‘grow out’ of the condition as they get older. If asthma is moderate-to-severe during childhood, it
is more likely to continue into adulthood. During the teenage years, the symptoms of asthma disappear in about three-quarters of all children with the condition.
Known risk factors for the development of asthma in children include:
- A family history of asthma, or other related allergic conditions (known as atopic conditions) such as eczema, hay fever or allergic conjunctivitis.
- Developing another atopic condition.
- Being exposed to tobacco smoke, particularly if the child’s mother smoked during pregnancy.
- Being born prematurely.
- Being born with a low birth weight.
A child with asthma should be taught to recognise the initial symptoms of an asthma attack, how they should respond, and when they should seek medical attention. Some children are less likely to develop asthma
than others. Studies have found those children who are given fewer antibiotics and those who live on or near farms have less asthma than children with different backgrounds. Medical researchers explain this with the ‘hygiene hypothesis’.
THE ‘HYGIENE HYPOTHESIS’
The ‘hygiene hypothesis’ is a theory that lack of exposure in early childhood to infectious agents means that the child’s immune system has not been activated sufficiently during childhood. This lack of exposure is down
to our super-clean world of modern living, including antibacterial washes, vaccinations, and general sterility where children are not exposed to germs in a similar manner to previous generations of children. The theory suggests that because the immune system is ‘not activated’ during childhood, this leads to the immune system becoming over-sensitive to common substances such as pollen, dust mites and animal fur, leading to the higher
incidence of autoimmune conditions like asthma, hay fever and eczema in recent years.
One of the first scientific explanations of this theory was by a lecturer in epidemiology from the London School of Hygiene and Tropical Medicine, David P Strachan, who published a paper on the theory in the British Medical Journal in 1989.15 He noticed that children from larger families were less likely to suffer from autoimmune conditions like asthma. Families have become smaller in the Western world over the last 40 years, meaning less exposure to germs and infections; it is over the same period that health authorities have seen an explosion in autoimmune conditions such as asthma.
Further studies have been conducted since then, supporting the theory. For example, studies show that autoimmune diseases are less common in developing countries, however when immigrants from developing countries come to live in developed countries where living environments are more sterile, these immigrants suffer from increased levels of autoimmune conditions like asthma, and the rate of autoimmune conditions increases the longer immigrants live in developed countries.16
If asthma is moderate-tosevere during childhood, it is more likely to continue into adulthood
It is a difficult issue to tackle for the healthcare professional advising parents who want the best for their children; common sense tells us all that cleanliness is important. As a pharmacist, it is difficult to advise on the best balance for parents in relation to this theory. No journal or book will give a pharmacist exact advice. In my opinion, a balanced view is to ensure children are administered important vaccines but also ‘allow kids to be kids’, let children play outside with friends and try not to worry about them encountering dirt and germs, but always be cautious with children with life-threatening food allergies.
SYMPTOMS OF ASTHMA
- Difficulty in breathing/shortness of breath.
- A tight feeling in the chest.
- Wheezing (a whistling noise in the chest).
- Coughing, particularly at night.
- Hoarseness.
These symptoms may occur in episodes, perhaps brought on by colds or chest infections, exercise, change of temperature, dust, or other irritants in the air, or by an allergy, ie, pollen or animals. Episodes at night are
common, often affecting sleep.
COMMON TRIGGERS
Anything that irritates the airways and brings on the symptoms of asthma is called a trigger. Common triggers include house dust mites, animal fur, pollen, tobacco smoke, exercise, cold air and chest infections. Other
triggers which are less common include nonsteroidal anti-inflammatory drugs such as ibuprofen and diclofenac, emotional factors such as stress, sulphites in some foods and drinks (found in certain wines and used as a preservative in some foods, such as fruit juices and jam), mould or damp in houses, and food allergies, ie, nut allergy.
WHAT HAPPENS DURING AN ASTHMA ATTACK?
During an asthma attack, something triggers inflammation, a natural biological process. Inflammation is one of the ways that the body’s immune system fights infection. If the body detects a lung infection, it starts the process of inflammation. White blood cells engulf the infection area to kill the infection and prevent it spreading. The white
blood cells cause the airways to swell and produce mucus. In an asthmatic, the airways are over-sensitive to the effects of inflammation. As a result, too much mucus is produced, and the airways swell more than usual. Also, as a response to the inflammation, the muscles surrounding the airways begin to contract, making the airways narrower and narrower. The combination of excess mucus, swelling and contraction of the airways makes breathing difficult and produces the wheezing and coughing that is associated with asthma.
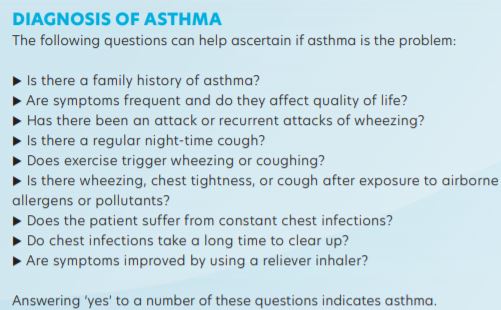
The following tests are often done to confirm the diagnosis of asthma:
- Spirometry is a simple breathing test that gives measurements of lung function. A spirometer is the device that is used to make the measurements. It is common to measure lung function with a spirometer before and after a dose of reliever to see if lung function has improved.
- Peak expiratory flow rate (PEFR) is a breathing test. It uses a simple handheld device called a peak flow meter, which a patient blows into to measure lung function. The PEFR test is only suitable for children over five years of age.
- An exercise test to check if exercise worsens asthma symptoms. tacks from developing. Successful prevention can be achieved through a combination of medicines, lifestyle changes and identification and avoiding asthma triggers.
WHEN TO GET IMMEDIATE HELP
The following are signs of a severe asthma attack:
- The reliever inhaler does not help symptoms at all.
- The symptoms of wheezing, coughing, tight chest are severe and constant.
- Too breathless to speak.
- Pulse is racing.
- Feeling agitated or restless.
- Lips or fingernails look blue.
It is important to seek immediate medical help when these symptoms occur.
NON-PHARMACOLOGICAL MANAGEMENT
Asthmatics should be advised strongly not to smoke and to lose weight.2 Allergen avoidance measures may be helpful but the benefit of avoiding allergens such as dust mites or animal fur has not been proven in studies.3,4
Currently, there is insufficient or no evidence of the clinical benefit of complementary therapy for asthma, such as Chinese medicine, acupuncture, breathing exercises and homeopathy.5
TREATMENT
There is no cure for asthma. Symptoms can come and go throughout the person’s life. Treatment can help control the condition. Treatment is based on relief of symptoms and preventing future symptoms and attacks from developing. Successful prevention can be achieved through a combination of medicines, lifestyle changes and identification and avoiding asthma triggers.
RELIEVER INHALERS
A short-acting beta 2-agonist opens the airways. These work quickly to relieve asthma. They work by relaxing the muscles surrounding the narrowed airways. Examples of beta 2-agonists include salbutamol and terbutaline. They are usually blue in colour. They are generally safe medicines with few side-effects, unless they are over-used. It is important for every asthmatic to have a beta2 agonist inhaler. If an asthmatic needs to use their beta agonist inhaler too regularly (three or more times per week), they should have their therapy reviewed.
The main sideeffects include a mild shaking of the hands, headache, and muscle cramps. These usually only occur with high doses of relievers and usually only last for a few minutes. Excessive use of short-acting relievers has been associated with asthma deaths.5,6 This is not the fault of the reliever medication, but is down to the fact that the patient failed to get treatment for their worsening asthma symptoms.
In exercise-induced asthma, sufferers are advised to use a short-acting beta 2-agonist 10-to-15 minutes before they exercise, and again after two hours of prolonged exercise, or when they finish.
PREVENTER INHALERS
Preventer inhalers are slower-acting inhalers that reduce inflammation in the airways and prevent asthma attacks occurring. The preventer inhaler must be used daily for some time before full benefit is achieved.
The preventer inhaler usually contains an inhaled corticosteroid. Examples of preventer medicines include beclomethasone, budesonide, and fluticasone. Preventer inhalers are often brown, red, or orange. The
dose of inhaler will be increased gradually until symptoms ease. For example, a patient may start on a beclomethasone 100mcg inhaler and may be put on a beclomethasone 250mcg inhaler if there is not
enough improvement in symptoms.
Preventer treatment is normally recommended if the patient:
- Has asthma symptoms more than twice a week.
- Wakes up once a week due to asthma symptoms.
- Must use a reliever inhaler more than twice a week.
Regular inhaled corticosteroids have been shown to reduce symptoms, exacerbations, hospital readmissions and asthma deaths.5,7,8-11 The majority of patients require a dose of less than 400mcg per day to achieve
maximum or near-maximum benefit. Sideeffects are minimal at this dose. Smoking can reduce the effects of preventer inhalers. Preventers are very safe at usual doses, although they can cause some side-effects
at high doses, especially over long-term use. The main side-effect of preventer inhalers is a fungal infection (oral candidiasis) of the mouth or throat.
This can be prevented by rinsing the mouth with water after inhaling a dose. The patient may also develop a hoarse voice. Using a spacer can help prevent these side-effects.
LONG-ACTING RELIEVER INHALERS
If short-acting beta 2-agonist inhalers and preventer inhalers are not providing enough symptom relief, a long-acting reliever (longacting beta 2-agonist) may be tried. Inhalers combining an inhaled steroid and a long-acting bronchodilator (combination inhaler) are more commonly prescribed than long-acting beta 2 agonists on their
own. Long-acting beta 2-agonists work in the same way as short-acting relievers, but they take longer to work and can last up to 12 hours.
A salmeterol inhaler is an example of a long-acting reliever inhaler used in Ireland. Long-acting relievers may cause similar side-effects to short-acting relievers, including a mild shaking of the hands, headache, and muscle cramps. Long-acting reliever inhalers should only be used in combination with a preventer inhaler. Studies have shown that using a long-acting reliever on its own (without a combination corticosteroid) can increase asthma attacks and can even increase the risk of death from asthma, though increased risk of death is small.17 In November 2005, the Food and Drug Administration in the United States issued an alert indicating the potential increased risk of worsening symptoms and sometimes death associated with the use of long-acting beta 2-agonists on their own.18
COMBINATION INHALERS
Examples of combination inhalers containing a long-acting beta 2 agonist and steroids include Seretide and Symbicort. Combination inhalers containing beta 2-agonists and corticosteroids can be very effective in
attaining asthma control. They have been shown to have better outcomes compared to leukotriene receptor antagonists, such as montelukast.19 Both treatment options led to improved asthma control; however, compared to leukotriene receptor antagonists, the addition of a long-acting beta 2-agonist to inhaled corticosteroids is associated with significantly improved lung function, symptom-free days, need for short-term beta 2-agonists, night awakenings, and quality of life.19 However, the magnitude of some of these differences is small.19
Most patients only need to take a course of oral corticosteroids for one or two weeks
OTHER PREVENTER MEDICATION
If treatment of asthma is still not successful, additional preventer medicines can be tried.
Two possible alternatives include:
- Leukotriene receptor antagonists (montelukast): Act by blocking part of the chemical reaction involved in inflammation of the airways.
- Theophyllines: Help widen the airways by relaxing the muscles around them. If asthma is still not under control, regular oral corticosteroids may be prescribed. This treatment is usually monitored by a respiratory specialist. Long-term use of oral corticosteroids has possible serious side-effects, so they are only used once other treatment options have been tried. Theophylline is known to cause potential side-effects, including headaches, nausea, insomnia, vomiting, irritability, and stomach upsets. These can usually be avoided by adjusting the dose. Leukotriene receptor agonists do not usually cause side-effects, although there have been reports of stomach upsets, feeling thirsty and headache.
OCCASIONAL USE OF ORAL CORTICOSTEROIDS
Most patients only need to take a course of oral corticosteroids for one or two weeks. Once the asthma symptoms are under control, the dose can be reduced slowly over a few days. Oral corticosteroids can cause sideeffects if they are taken for more than three months or if they are taken frequently (three or four courses of corticosteroids a year).
Side effects can include:
- Weight gain.
- Thinning of the skin.
- Osteoporosis.
- Hypertension.
- Diabetes.
- Cataracts and glaucoma.
- Easy bruising.
- Muscle weakness.
- To minimise the risk of taking oral corticosteroids, a person should:
- Eat a healthy, balanced diet with plenty of calcium.
- Maintain a healthy body weight.
- Stop smoking.
- Only drink alcohol in moderation.
- Do regular exercise.
WHEN CAN THERAPY BE REDUCED?
Once control is achieved and sustained, gradual stepping-down of therapy is recommended.5
Good control is reflected by the absence of night-time symptoms, no symptoms on exercise, and the use of relievers less than three times a week. Patients should be maintained on the lowest effective dose of inhaled
steroids, with reductions of 25-to-50 per cent being considered every three months.
SPACER DEVICES
Spacers are large plastic or metal containers with a mouthpiece at one end and a hole for the inhaler at the other. The medicine is puffed into the spacer by the inhaler and it is then breathed in through the spacer mouthpiece. Spacer devices in combination with metered dose inhalers (MDI) have several advantages: a) No need to co-ordinate inhaler activation with inspiration; b) improvement in lung deposition; and c) reduction in oropharyngeal deposition (resulting in fewer local side-effects and lower systemic absorption).2 Some inhalers emit an aerosol jet when pressed. These work better if given through a spacer, which increases the amount of medication that reaches the lungs and reduces side-effects.6
Some patients, especially children and elderly patients, find using inhalers difficult, and spacers can help. However, spacers are often advised even for patients who use inhalers well, as they improve the distribution of medication in the lungs. Spacers are also good for reducing the risk of thrush in the mouth or throat with corticosteroid inhalers. When a spacer device is being used, only one puff of the inhaler must occur at a time.
ASTHMA DEATHS
Underestimating the severity of the fatal attack by the doctor, patient or relatives is the biggest cause of death in asthmatics.5,12,13 There were 92 asthma-related deaths in Ireland in 1999.1 The risk of dying from asthma
increases with age and asthma-related deaths are extremely rare in children. Patients at most at risk of death are those who have severe asthma, are obese, have a history of non-compliance with therapy and have one or more adverse psychological factors, such as: Alcohol or drug use; employment or income problems; social isolation; or current or recent tranquilliser use.
ASTHMA AND COVID-19 RISK
People with moderate-to-severe asthma may be at higher risk of getting very ill from Covid-19. Covid-19 can affect the nose, throat, lungs (respiratory tract); cause an asthma attack; and possibly lead to pneumonia and
acute respiratory disease.20 Patients with severe asthma are classed as the highest risk (extremely vulnerable) to Covid-19. Those with less-severe asthma are classed as highrisk to Covid-19.21 Depending on the patient’s
asthma severity, asthmatics will be higher in the priority list during the Covid-19 vaccine roll-out.
Currently, there is no evidence of increased infection rates in those with asthma.22 The best advice for asthmatics during this pandemic is to keep doing what they are advised to do all along — continue taking the controller medication and inform a healthcare provider of any symptoms that develop. The normal public health advice, including practicing social distancing and washing hands regularly, is the best advice.22
ASTHMA AND PREGNANCY
Medication used for asthma will not cause any problems for the developing baby in the womb. Due to the changes that take place in the body during pregnancy, asthma symptoms may change during pregnancy. For
some women, asthma improves; for others, asthma worsens and for others, asthma stays the same. The most severe asthma symptoms experienced by pregnant women tend to occur between the 24th and 36th week of
pregnancy. Symptoms then decrease significantly during the last month of pregnancy.
Only 10 per cent of women experience asthma symptoms during labour and delivery, and these symptoms can normally be controlled using reliever medicine. Asthmatics who are pregnant should manage their asthma in the same way as before pregnancy. The medicines used for asthma have been proven to be safe to take during pregnancy and when breastfeeding. The one exception is leukotriene receptor antagonists (Montelukast).
There is no evidence that it can harm babies during pregnancy and breastfeeding. However, there is not enough evidence about its safety compared with other asthma medications. However, if leukotriene receptor antagonists are needed to control asthma during pregnancy, the GP or asthma clinic may recommend that they are continued. This is because the risks to the patient and child from uncontrolled asthma are far higher than any
potential risk from this medicine. Theophyline is often avoided during pregnancy and breastfeeding because of reports of neonatal irritability and apnoea.
Written and researched by Eamonn Brady (MPSI), owner of Whelehans Pharmacies in Mullingar
References
- Brennan N, O’Connor T. Ireland needs healthier airways and lungs
– the evidence (INHALE). June 2003. - Stenius-Aaniala B, Pousa T, Kvarnstrom J, Gronlund EL et al.
Immediate and long-term effects of weight reduction in obese people
with asthma: randomised controlled study. BMJ 2000; 320: 827. - Cochrane Review on house dust mite control. BMJ 1998; 317:
1105-10, Cochrane Database of Systemic Reviews. 2004 Oct 18; 4. - Woodcock A, Forster L, Matthews E et al. Control of exposure to
mite allergen and allergen-impermeable bed covers for adults with
asthma. NEJM 2003 Jul 17; 349 (3): 225-36. - British Guideline on the Management of Asthma BTS, SIGN,
Revised edition April 2004 www.sign.ac.uk (Guideline 63). - Spelman R, Guidelines for the diagnosis and management of
asthma in general practice, ICGP 2003 (Jan). - Cates C Chronic Asthma – Extracts from ‘Clinical Evidence’. BMJ
2000; 323: 976-9. - Hatoum HT, Schumock GT, Kendzierski DL. Meta-analysis of
controlled trials of drug therapy in mild chronic asthma: The role of
inhaled corticosteroids. Ann Pharmacotherapy 1994; 28: 1285-1289. - O’Byrne PM, Barnes PJ, Rodriquez-Roisin R et al. Low dose inhaled
budesonide and formoterol in mild persistent asthma. American
Journal Respiratory and Critical Care Medicine 2001; 164: 1392-97. - Blais L, Ernst P, Boivin J-F, Suissa S. Inhaled corticosteroids and the
prevention of readmission to hospital for asthma. American Journal
Respiratory and Critical Care Medicine 1998; 158: 126-32. - Suissa S, Ernsst P, Benayoun S, Baltzan M et al. Low dose inhaled
corticosteroids and the prevention of death from asthma. NEJM 2000;
343: 332-36. - Bucknall CE, Slack R, Godley CC et al on behalf of SCIAD
collaborators. Scottish Confidential Inquiry into Asthma Deaths
(SCIAD), 1994-6. Thorax (BMJ) 1999; 54: 978-84. - Burr ML, Davies BH, Hoare A et al. A confidential inquiry into
asthma deaths in Wales. Thorax (BMJ) 1999; 54: 985-89. - www.asthmasociety.ie/all-about-asthma/Asthma-Statistics
(accessed by E Brady in 2012). - Strachan DP (November 1989). Hay fever, hygiene, and
household size. BMJ 299 (6710): 1259–60. - Gibson PG, Henry RL, Shah S, Powell H, Wang H (September
2003). Migration to a Western country increases asthma symptoms
but not eosinophilic airway inflammation. Pediatric Pulmonology.
36 (3): 209–15. - Shelley R Salpeter; Nicholas S Buckley; Thomas M Ormiston;
Edwin E Salpeter. Meta-Analysis: Effect of Long-Acting Beta-Agonists
on Severe Asthma; Exacerbations and Asthma-Related Deaths. Annals
of Internal Medicine. Volume 144, No. 12. June 2006: 904-912. - Advair Diskus, Advair HFA, Brovana, Foradil, Perforomist, Serevent
Diskus, and Symbicort Information (Long-Acting Beta Agonists). Post
Market Drug Safety information for patients and providers. www.fda.
gov. November 2005. - Ducharme FM, Lasserson TJ, Cates CJ. Long-acting beta
2-agonists versus anti-leukotrienes as add-on therapy to inhaled
corticosteroids for chronic asthma (Review). Cochrane Review. 2009
(Issue 3):1-107 - People with Moderate to Severe Asthma, National Centre for
Immunisation and Respiratory Diseases (NCIRD), Division of Viral
Diseases (US), Nov 2020. - Covid-19 and Asthma: What patients need to know. American
Academy of Allergy, Asthma & Immunology. Dec 2020 - People at higher risk from Covid-19. Health Service Executive,
Dec 2020.







