Eamonn Brady MPSI provides a clinical overview of the different types of migraine, how to distinguish them from common headache, and the treatment options available
Migraine is a real condition, just like asthma, diabetes or epilepsy. Although not life-threatening, it has been found to have a greater impact of quality of life than conditions such as heart disease and diabetes. The World Health Organisation classifies migraine as the 12th-leading cause of disability worldwide among women and the 19th overall.
What is migraine?
Migraine is more than just a headache. It is a complex, attacking neurological condition. With attacks lasting anything from a couple of hours to perhaps three days, it is easy to see why it can have such a debilitating effect on those living with the condition. Migraine affects 12-to-15 per cent of people worldwide (around one billion), with similar percentage figures reported (up to 500,000) for those living with the condition in Ireland. In as many as 60 per cent of cases, the condition is inherited.
Prior to puberty, boys experience migraine as often as girls. Once into adulthood, migraine becomes three times more common in women than in men. This is due in large part to the hormonal changes in women from puberty to menopause. The highest prevalence in women around age 40, which then tails-off in the postmenopausal years.
With such high numbers affected in Ireland, it stands to reason that there are also economic and work-related impacts to be considered.
Ninety-two per cent of Irish migraineurs report that attacks affect their performance at work, with 39 per cent of those being severely affected. Therefore, the unemployment rate for those with severe migraine is two-to-four times higher than the prevailing overall rate. Migraine accounts for the loss of over half a million working days in Ireland each year, with 37 per cent of working Irish migraineurs missing more than five days per annum; the resultant cost to the economy is at least €250 million.
Causes
Whilst the precise cause of migraine is unknown, it is generally accepted that it relates to the abnormal functioning of nerve cells that affect the brain’s ability to process information such as pain, light, sounds and other sensory stimuli. As the condition is very individual, how each migraineur arrives at this point is then determined by a varied number of ‘trigger factors’, but generally once there, a pattern emerges, and an attack ensues.
These factors can be physical, environmental or genetic and in most cases, it will be a particular individual combination that will precipitate an attack. Someone may experience all or only some of the different stages of migraine during an attack. It follows, then, that identifying triggers is one of the keys to successful management of the condition.
Common symptoms and types
The word ‘migraine’ derives from a Greek word hemicrania (half-skull), which literally means ‘pain on one side of the head’. This accurately describes and differentiates migraine from other types of headache, as typically, it presents on one side of the head. An attack may consist of some or all the following symptoms:
Migraine without aura (around 80 per cent of all attacks)
- Moderate-to-severe pain, throbbing one-sided headache, aggravated by movement.
- Nausea and/or vomiting.
- Hypersensitivity to external stimuli (ie, noise, smells, light).
- Stiffness in neck and shoulders.
- Pale appearance.
Migraine with aura (in addition to above symptoms)
- With aura, around 20 per cent experience visual disturbances prior to the headache lasting up to one hour (most commonly blind spots, flashing light effect or zig-zag patterns; may also include physical sensations such as unilateral pins and needles in fingers, arm and then face).
- Blurred vision.
- Confusion.
- Slurred speech.
- Loss of co-ordination.
Other types:
Basilar migraine
Usually affecting teenage girls, this is a rare form of migraine that presents additional symptoms such as loss of balance, fainting, difficulty speaking and double vision. There can be loss of consciousness during an attack.
Hemiplegic migraine (sporadic or familial)
Usually beginning in childhood, this severe form of migraine causes temporary unilateral paralysis. May also feature extended aura period that could last for weeks. Generally related to a strong family history of the condition. It is a rare form of migraine; diagnosis usually requires a full neurological exam, as the symptoms may be indicative of other underlying conditions.
Ophthalmoplegic migraine
In addition to headache, this very rare form of migraine shows additional symptoms, such as dilation of the pupils. Inability to move the eye in any direction, as well as drooping of the eyelid, occurs. It occurs primarily in young people and is caused by weakness in muscles which move the eye.
Abdominal migraine
Symptoms are usually nausea- and stomach-related rather than headache. Occurs predominantly in children, usually evolves into typical migraine with age.
Triggers
A myriad of trigger factors, whilst in themselves not the cause of migraine, can build, bringing an individual to the point where a migraine attack is imminent. Again, these can be different for everyone and indeed, may differ for an individual each time, depending on their situation; trying to track down specifics can be difficult.
Let’s look at some of the most common:
Environmental factors
Just moving around doing normal day-to-day activities, which wouldn’t cost you a second thought, can be a potential danger for someone susceptible to migraine. Also:
- Bright or flickering lights (could be cinema, shop displays or sunlight through trees whilst driving).
- Certain types of lighting (fluorescent, strobe).
- Strong smells (especially perfume, paint, etc).
- Weather (variety of factors, ie, bright sun glare, muggy close days, humidity).
- TV/computer screens and monitors.
- Loud and persistent noise.
- Travel areas of pressure change, ie, altitude.
Just moving around doing normal day-to-day activities can be a potential danger for someone susceptible to migraine
Dietary triggers
Research indicates about 20 per cent of migraine attacks are brought on by dietary factors. Whilst people believe this to be the case, actual scientific evidence proving a link is virtually non-existent. In many cases, there may be other factors that precede consuming a ‘suspect’ food that could contribute more to the onset of an attack, ie, lack of sleep, skipping meals.
The most cited link is foods which are high in the amino acids tyramine and/or phenylethylamine, such as:
? Cheese (fermented, aged or hard mouldy types).
- Chocolate.
- Alcohol (beer and red wine particularly).
- Nitrites (common in processed meats).
- Sulphites (ie, preservative in dried fruit and red and white wine).
- Additives (MSG).
- Aspartame (diet drinks).
- Caffeine (coffee, tea, etc, although caffeine can be used to prevent migraine; it’s down to personal tolerance).
Hormonal triggers
Once females move into puberty and then adulthood, hormones play an increasing role in migraine prevalence. Oestrogen fluctuations due to menstruation or using oral contraceptive pills or HRT can sometimes trigger migraine. Conversely, migraine susceptibility can decrease during pregnancy when oestrogen levels are high.
In the main, migraine attacks lessen post-menopause (although can increase in the years preceding it). Identifying triggers can be the single most important step an individual can take in helping themselves to manage their condition. It may not be necessary to avoid situations completely, but instead build levels of awareness so that appropriate preventative steps and actions can be taken.
Treatment
The key to successful treatment is to establish correct diagnosis of migraine and eliminate other potential causes (tension or cluster headache in particular; see more at end of this article about non-migraine headaches). Some time spent with patients at an early stage reviewing their current medication regimen would prove hugely beneficial in identifying and/or preventing ‘medicine overuse headache’. In acute treatments, the goal is to stop or at least alleviate the effects of an attack once it has begun.
Analgesics
Used to target area-specific pain and especially if taken as early as possible once an attack begins, analgesics can be a hugely effective pain killer.
Aspirin
Traditional first line of defence, has anti-inflammatory properties that can help alleviate many of the physical symptoms of migraine.
Paracetamol
As effective as aspirin, but without the anti-inflammatory effects.
Combinations
Drugs that contain aspirin or paracetamol along with another agent such as codeine or caffeine; codeine and other opiates are best avoided due to addiction, side-effect risk and risk of triggering overuse headaches.
NSAIDs
Generally used for more severe migraine attacks, evidence shows ibuprofen to be highly effective. Soluble forms may act quicker than tablet form for those where stomach issues are part of their migraine episode.
Triptans
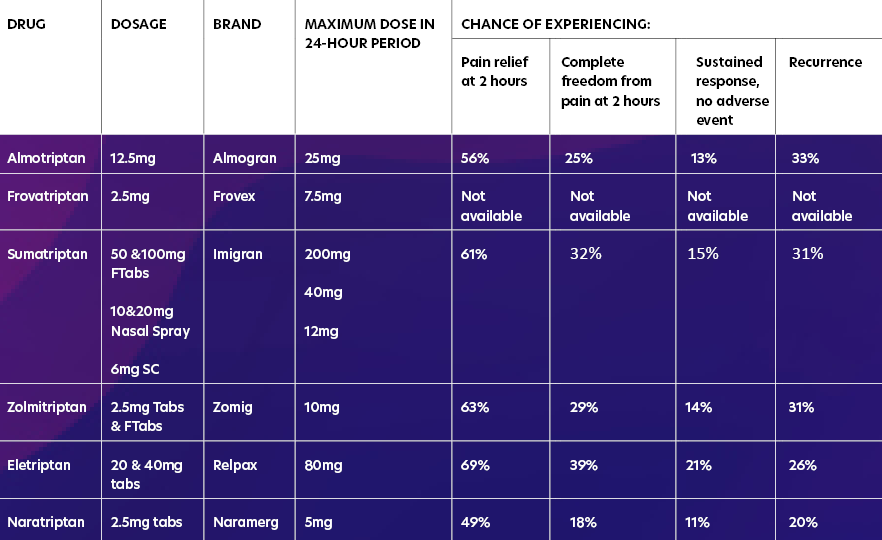
Triptans are highly effective, reducing the symptoms or aborting the attack within 30-to-90 minutes in 70-to-80 per cent of patients. Triptans target those neural serotonin receptors specifically involved in migraine attacks and can be used in the treatment of migraine with or without aura. All of them are available in tablet form, with some brands also available as fast-melt tabs, nasal spray or SC injection.
The table above shows those triptans available in Ireland, along with information from trials regarding effectiveness over the course of an episode. In all cases, these are only for treatment where migraine has been diagnosed and not for the treatment of hemiplegic, basilar or ophthalmoplegic migraine. Currently, all are POM, apart from sumatriptan, which now has an option for sale OTC in the pharmacy for patients who have been prescribed it in the past.
Preventative medication for migraine
Prophylactic medication may be considered if the patient has taken adequate lifestyle steps to prevent migraine, such as using a diary to determine triggers and avoidance of these triggers, but the migraine continues. It would be reasonable for a prescriber to consider prophylaxis for migraine if a patient must use analgesics for eight or more days of the month.
Prophylactic medication should be tried for four-to-six months at a reasonable dose to determine if it is working effectively. Prophylactic medication has potential side-effects that can limit dose or use. Amitriptyline, topiramate and flunarizine are the three most prescribed migraine prophylactic drugs, with amitriptyline being the most prescribed. Other prophylactics such as sodium valproate, pregabalin, gabapentin and pizotifen are considered second-line (often only used if the first three are not tolerated or ineffective).
Amitriptyline
A traditional tricyclic antidepressant but not used much for depression due to side-effects such as drowsiness, constipation, dry mouth, vivid dreams or nightmares and risks in people with glaucoma. It is dangerous in overdose. Low dose may be effective in preventing migraine; the dose for migraine varies between 10mg to 150mg, but the lower the better and it should only be titrated up slowly. Use at six months at maximum tolerated dose before considering changing.
Topiramate
Topiramate is traditionally an epilepsy drug that is sometimes used in low-dose form to prevent migraine. It must be used in caution in those with liver or kidney problems and must be avoided in pregnancy. Possible side-effects include nausea, vomiting, constipation, diarrhoea, decreased appetite, drowsiness and sleeping problems. Highest daily dose of 700mg but for migraine, recommended dose is 25mg to 200mg twice daily. Starting dose is 25mg at night for two-to-eight weeks and increase gradually.
Propranolol (Inderal)
This is an old-style beta blocker traditionally used for angina and blood pressure but is rarely used for these indications nowadays due to safer, newer versions of beta blockers with less side-effects. However, in low doses, it is used for migraine prophylaxis in some. It should be used in caution in people with asthma, COPD, some heart problems and diabetes. Side-effects can include cold hands and feet, pins and needles, tiredness and sleeping problems.
Flunarizine (Sibelium)
Flunarizine can take months to see a significant reduction in symptoms. Patients should be regularly reviewed to assess their response to this preventive treatment, and if a sustained attack-free period is established, interrupted flunarizine treatment should be considered.
Flunarizine maintenance treatment
If the patient is responding satisfactorily to flunarizine and a maintenance treatment is needed, the same daily dose should be used, but this time interrupted by two successive drug-free days every week, ie, Saturday and Sunday. Even if the preventative maintenance treatment is successful and well tolerated, it should be interrupted after six months and it should be re-initiated only if the patient relapses.
Migraine is quite distinct from other headache types in how it presents and in how an episode evolves, attacks and subsides
Treatment is started at 10mg daily (at night) for adult patients aged 18-to-64 years and at 5mg daily (at night) for elderly patients aged 65 years and older. It is good practice to start at 5mg for all patients before titrating up. Side-effects include increased weight, increased appetite, depression, insomnia, constipation, stomach discomfort and nausea.
Gabapentin
Like topiramate, gabapentin is traditionally an epilepsy drug. It may be used if topiramate, flunarizine or propranolol are not effective or tolerated. However, in recent years, studies have indicated that gabapentin may not be as effective for preventing migraine as first thought. Side-effects can include dizziness, drowsiness, appetite increase, weight gain and suicidal thoughts.
Sodium valproate is another epilepsy drug occasionally used for migraine prevention if other prevention options fail or are not tolerated. Other preventative medicines include pizotifen (Sanomigran) and pregabalin (Lyrica).
Riboflavin (vitamin B2)
There has been some indication that vitamin B2 supplementation may help prevent migraine; however, this has not been proven.
Is it really migraine? Distinguishing between non-migraine headache
One of the most important steps in the successful management of migraine is in diagnosing that it is actually migraine which is the cause of the headache. Migraine is quite distinct from other headache types in how it presents and in how an episode evolves, attacks and subsides. Let’s look at the three most common ‘primary’ types of non-migraine headache (secondary being headaches caused by other medical conditions).
Tension headache
The most common type of headache is tension headache and is usually caused by stress, poor posture or inadequate lighting. Often beginning in the afternoon or early evening of a stressful day and presenting as a ‘band-like’ or ‘pressing’ sensation at the front of the head, they can last from one-to-six hours.
With tension headache, pain tends to be bilateral (both sides of head), constant and with no other symptoms as opposed to migraine, which is usually confined to one side of the head, together with other identifiable symptoms.
For most, treatment with an analgesic (paracetamol, aspirin or ibuprofen) will usually take care of it. Engaging in self-management activities such as regular exercise, regular eye breaks from the computer at work, sensible eating habits and learning stress management techniques can all lead to a reduction in tension headaches.
Chronic daily headache
Different from tension headache, which is episodic in nature, chronic daily headache (CDH) refers to any headache that occurs on at least 15 days per month with each at least four hours’ duration. Currently affecting 4-to-5 per cent of the population (and growing), variants of CDH can significantly affect an individual’s ability to function at work, at home and socially. There are three distinct types:
Chronic tension headache
Typically affects those with a history of ordinary tension headache and whilst similar, it occurs on at least 15 days per month. Whereas tension headache is usually related to individual situations, chronic tension headache tends to be provoked by more enduring ongoing personal situations, ie, job issues, family and relationship problems, grief, depression.
Chronic (transformed) migraine
Diagnosed if you have migraine on 15 or more days a month over a period of at least six months. Over time, people with this diagnosis may experience an additional daily or almost-daily headache. As the frequency of these headaches increases, there is a corresponding decrease in actual headache pain along with other migraine symptoms. The downside of this perceived relief is that the headaches become less responsive to treatment. With other effects, such as depression and sleep disturbance, people will usually experience a more typical ‘breakthrough’ migraine attack on top of the enduring ‘background’ headache.
Medication overuse headache
This is caused by the overuse of medication, taken primarily to alleviate headache. In the main, this relates to analgesics (paracetamol, codeine, aspirin or ibuprofen), although can also occur with migraine-attacking drugs (triptans). Those most affected are those with a history of tension headaches or migraines that have become more frequent or severe over time.
They take medication to gain relief from the pain, only to find the headache returning once the drugs have worn off. Sufferers then take more medication to alleviate continued pain, pain eases, drugs wear off, pain returns, etc (a vicious cycle). It becomes easy then to fall into a cycle of taking medication for a headache that is itself caused by medication. Once in this spiral, the only way is to break the cycle completely is through withdrawal.
Typical withdrawal side-effects can be worsening headaches, nausea and anxiety for a couple of weeks. Withdrawal is best achieved through consultation with a medical professional; the GP may be the patient’s first point of call, but the pharmacist has a major role in recognising signs of medication overuse headaches (ie, regular headaches, frequent purchases of analgesics) and is well placed to help the person identify and tackle the problem.
Cluster headache
Affecting around 1 per cent of people, this is a rare but very severe headache found six times more commonly in men and usually begins in late 20s or early 30s. Typically, attacks begin in the middle of the night. Primary symptom is a severe stabbing pain affecting one side of the head. The side affected can vary between attacks, but only in very rare cases would it affect both sides of the head at the same time. The duration of an attack can be between 15 minutes and up to three hours. Attacks come in clusters (hence the name) and can occur several times a day over a period of weeks or even months. After each cluster, attacks can disappear for months or years.
Typical withdrawal side-effects can be worsening headaches, nausea and anxiety for a couple of weeks
A cluster attack can be distinguished from a migraine attack in that with cluster headache, the person is agitated during an attack or unable to sit or lie at peace or find relief though sleep. During an attack, other symptoms may occur, such as red or watery eyes, runny nose, nasal congestion, or facial sweating. In addition, a sufferer’s eyes may be affected, with constriction of the pupil or drooping or swelling of the eyelid. Cluster headache has been described by some medics as ‘the most painful event that can happen to a person’, which emphasises the severity of the condition.
Whilst the cause is unknown, suspected trigger factors include alcohol, tobacco, irregular sleeping patterns, and stress and decreased blood oxygen levels. The most common treatment for cluster headache is the inhalation of pure oxygen and is only successful if the mask fits perfectly without leaking. The GP will be able to help with further information.
The three ‘primary’ types of headache I have described are the most common non-migraine headaches. There are other types of headache, ie, those relating to sinus problems or over-exertion, especially exercise. These are known as secondary headaches.
The pharmacist’s role
- Familiarise yourself with diagnostic criteria, which are available on www.migraine.ie, to enable you to recognise migraine and distinguish between migraine and other headache types, ie, cluster headaches, tension headaches.
- Enquire what treatments and medication the patient has used already to treat the headaches.
- Familiarise yourself with the stepwise analgesic ladder recommended for headaches and migraine, starting with paracetamol, aspirin and ibuprofen.
- As sumatriptan is now classified as a P medicine, pharmacists should familiarise themselves with this and the protocol of when they can offer it to a patient, ie, patients aged 18-to-65 who have been previously diagnosed with migraine by their GP.
- Pharmacist should be able to identify when to refer to a GP.
References
- NICE Clinical Guideline 150. Headaches costing report. September 2012.
- The Irish Nurses & Midwives Organisation, http://www.inmo.ie/Home/Index/7066/8626.
- World Health Organisation. The Global Burden of Disease: 2004 update, Part 3, p28–37. http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/.
- WHO (2001) The World Health Report 2001: Mental health, new understanding, new hope. World Health Organisation, Geneva, Switzerland, www.who.int/whr/2001/en/whr01_en.pdf.
- World Health Organisation. Lifting the Burden: Atlas of headache disorders and resources in the world 2011. WHO, Geneva; 2011.
- Steiner TJ. Lifting the burden: The global campaign against headache. The Lancet Neurology. 2004; 14:204–205. doi: 10.1016/S1474-4422(04)00703-3.
- Steiner TJ. Lifting The burden: The global campaign to reduce the burden of headache worldwide. J Headache Pain. 2005; 14:373–377. doi: 10.1007/s10194-005-0241-7.
- PSI. Pharmacy Practice Guidance 03. Guidance for Pharmacists on the Safe Supply of Sumatriptan 50mg Tablet. Oct 2018.







