A team, led by scientists from the Trinity Biomedical Sciences Institute (TBSI), has unearthed the possible target for treating the debilitating skin disease hidradenitis suppurativa (HS), which is a painful, chronic, inflammatory skin condition that can last decades.
Despite affecting up to 1% of the population it is often under-recognised and under-diagnosed. Given its high morbidity, reduced quality of life and poorly understood disease trajectory, there is an unmet need for effective therapeutic options, with new treatments badly needed.
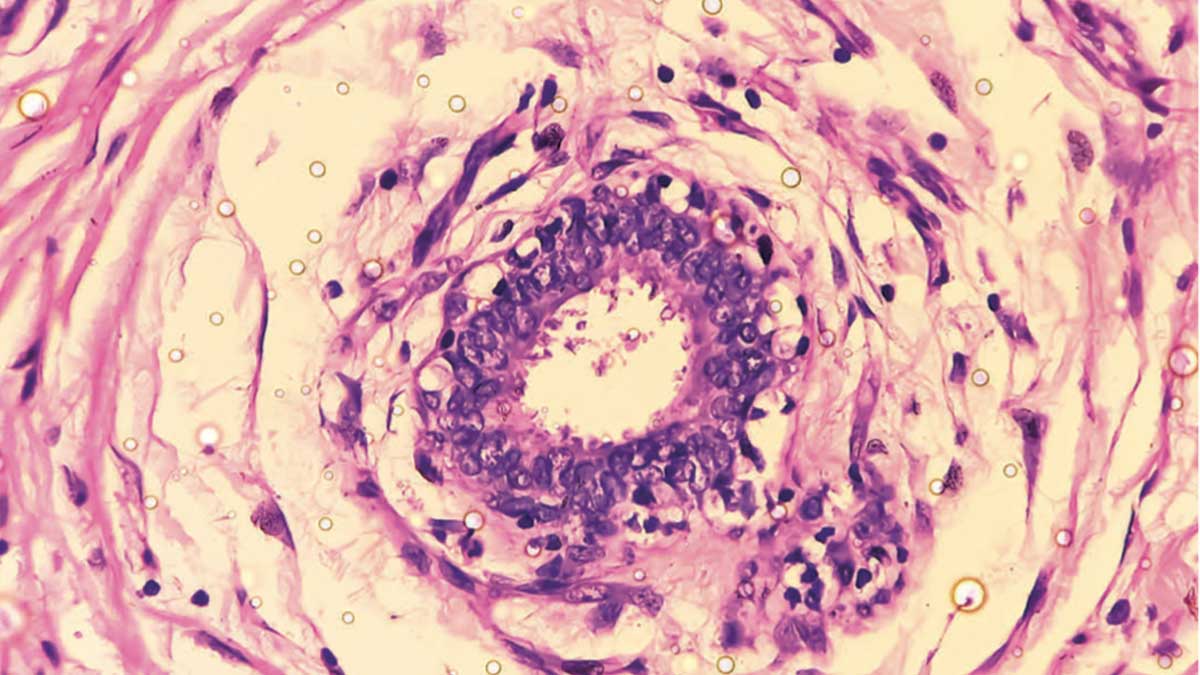
In the research, led by Dr Barry Moran and Conor Smith from Trinity’s School of Biochemistry and Immunology, and Professor Jean Fletcher from the School of Medicine, the scientists identified significantly increased numbers of proinflammatory immune cells in skin samples collected from HS patients.
Among other immune populations usually infrequent in healthy skin, these included Th17 cells, B cells, plasma cells and neutrophils.
When they analysed the gene profiles of thousands of these individual cells, they noted that genes and pathways linked with inflammation-associated Th17 cells, cytokines IL-17 and IL-1?, and the inflammation complex known as the NLRP3 inflammasome, were enhanced in HS skin – particularly in samples with a high inflammatory load.
Importantly, with regard to unearthing a potential target for treatment, the scientists then showed that blocking this NLRP3 inflammasome with a small molecule inhibitor significantly reduced the secretion of key inflammatory mediators in HS skin samples.
Speaking about the research, which has just been published in the prestigious British Journal of Dermatology, Dr Moran said: “Our work provides the first proof of principle that inhibiting the NLRP3 inflammasome reduces inflammation in HS skin and, as such, we have unearthed a potential target for treating this debilitating condition. Ultimately, we now have a rationale for targeting the inflammasome in HS using small molecule inhibitors, which are currently in trials for other indications.”
Conor Smith, co-author and PhD candidate at Trinity, said: “This was a real collaborative effort between our clinical partners in St Vincent’s University Hospital, particularly Professor Brian Kirby and his team who recruited patients and contributed invaluable clinical input, and our team in TBSI providing the scientific and technical expertise to make this study successful.
“Much of the research that we do here in the Fletcher lab is focused on improving our understanding of this debilitating disease and identifying potential new therapeutic options. We hope that this study can prompt further clinical investigations into the suitability of targeting the NLRP3 inflammasome to treat HS.”
Prof Fletcher added: “These small molecule inhibitors targeting the NLRP3 inflammasome may offer new treatment avenues beyond the biological treatments currently (or likely to be) approved in treating HS.”
This work was supported by a number of funders, including Science Foundation Ireland, AbbVie, Trinity’s Provost’s PhD Project Award, the British Skin Foundation and the City of Dublin Skin and Cancer Hospital Charity. An embargoed copy of the published journal article is available on request. The paper can be read on the publisher’s website.