The most recent worldwide survey on the emerging role of vaccination in pharmacies sheds light on increasing public trust in the profession but also highlights areas where significant improvement is required. Pat Kelly reports
The latest global survey by the International Pharmaceutical Federation (FIP) reinforces the case for pharmacists to be given powers to extend vaccination services and illustrates an ever-increasing level of trust in the profession among the public. However, it also highlights the barriers and obstacles for the uptake of pharmacy-based vaccination (PBV). The report, titled An Overview of Pharmacy’s Impact on Immunisation Coverage, is the first such report since 2016 and involved 106 organisations from 99 countries, amounting to the most representative survey on the subject ever, with more than double the number of responses compared to the 2016 survey.
In this survey, a number of aspects related to pharmacist-led immunisation were evaluated, including vaccine administration, training and certification, vaccination records, advocacy initiatives, regulatory frameworks and barriers and limitations to expanding pharmacy to include vaccination services.
Among the main findings were that few respondents reported higher levels of engagement activities, such as assessing vaccination status and identifying high-risk groups. As a result, an increase in proactive advocacy initiatives was recommended.
Engagement
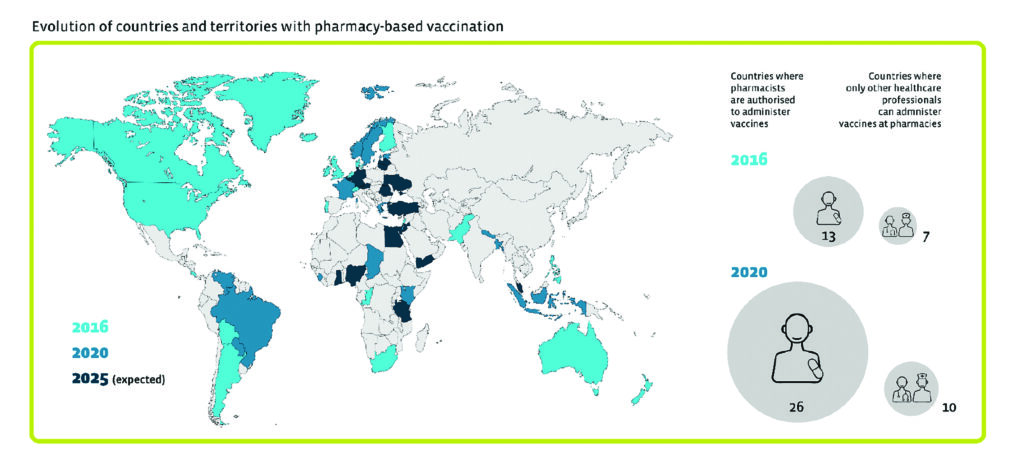
Different levels of pharmacist engagement were reported, however 70 per cent of respondents said pharmacists play an active role in educating members of the public on the facts around vaccine-preventable diseases and advocating for vaccination. Overall, PBV is now available in 36 countries and territories, representing an increase of 16 compared to the 2016 study (see figure). However, the authors noted that there is a “long way to go” in terms of vaccination administered by pharmacists, with 66 countries and territories not having PBV in place currently. Of those 66 countries and territories, 16 said they are either developing or proposing pharmacist-led vaccination policies, which they hope will take effect within the next one-to-five years.
In terms of the administration of PBV, pharmacies are involved in providing 36 different vaccine types, with the most commonly-administered ones being influenza (94 per cent of respondents); followed by hepatitis B (61 per cent); and tetanus (58 per cent), while 96 per cent reported that they are authorised to vaccinate adults. In almost 80 per cent of vaccinations, pharmacists are accountable as vaccine administrator, pharmacy manager or pharmacy owner.
When a vaccine for Covid-19 becomes available, the authors stated that pharmacies “should be part of the vaccination pathways”. They also wrote that in light of the fact that influenza, pneumococcal disease, herpes zoster and pertussis are major causes of mortality and morbidity in the elderly population, pharmacists should be part of a greater focus on vaccination throughout the patient’s life course.
The expansion of pharmacists’ role in immunisation is encouraging, but not sufficient. Legislative and regulatory barriers must be overcome through evidence-based, quality advocacy, and they must address key issues, including reimbursement schemes
Reimbursement
Unsurprisingly, 78.4 per cent of respondents said reimbursement for vaccination services is ‘important’ or ‘very important’. However, only 10 respondents said the service is reimbursed by public health systems, with five reimbursed by private systems. In most countries and territories, vaccinations are paid for by the customer and in six cases, it is provided at no cost to the patient or health system, with the cost absorbed by the pharmacy itself.
In the area of vaccination records, the authors noted that it is “regrettable” that pharmacists do not have access to vaccination records in most countries and territories and even in countries where PBV services are established, only 12 out of 33 of these had full access to records, with the remaining 21 reporting access to some records only.
A disparity in continuity of care was also highlighted by the fact that in almost 50 per cent of countries and territories with PBV, pharmacists are not authorised to record vaccination details in a shared patient vaccination record. “This is a significant barrier in complex health systems where all healthcare professionals must know the vaccination status of each patient,” the authors wrote.
Where records do exist, paper-based vaccination records are the most common method, at 73 per cent of respondents, while shared electronic systems are in place in 27 countries and territories. However, it was noted that “barriers exist for pharmacists to be given read and write access. Correcting these barriers should involve logistical efforts and regulatory frameworks to create records that are easily accessible, comprehensive and readily and easily shared.”
In terms of training, in 35 countries where PBV is in place, a full 100 per cent of respondents said postgraduate training for pharmacists in vaccination exists, with undergraduate training in place in 16 countries. However, mandatory vaccine training is in place in only 68 per cent of cases within a subset of 22 respondents with PBV in place. “With more pharmacists gaining the authority to administer vaccines, it is imperative that training is put in place, in addition to certification renewal programmes, to ensure quality and sustainability of services,” the authors stressed.
Barriers
Overall, almost 1.8 billion people worldwide now have access to community pharmacy-based vaccination services, which represents an increase of almost 100 per cent compared to the 2016 study. However, barriers to further PBV exist and many of these are associated with governments and other healthcare professionals, and these are perceived as the most important obstacles among the respondents. In addition, lack of financial support from health systems was implicated and was considered an important component of equitable access to PBV and service sustainability.
However, once a PBV service is put in place, the results suggest that patients recognise its value and actively seek PBV. Another problem is “perceived barriers”, and these were noted between countries with or without PBV, with the perceived lack of patient demand or acceptance also noted. This was reported by 18 respondents, but was reported by only one with PBV.
Lack of confidence among pharmacists was also apparent in the results, at 43 per cent in countries and territories without PBV compared to 19 per cent of those where the service is in place; similarly, 51 per cent of countries without PBV cited limited access to training opportunities, compared to 23 per cent among those with the service in place. The authors suggest that this is overcome when regulatory frameworks support the delivery and implementation of the service.
In conclusion, the authors wrote that progress is evident and they highlighted the major increase in the availability of PBV worldwide. “An important increase in the number of countries where policy development is underway was also noted, which will only further pharmacists’ engagement in immunisation, increase availability to vaccine services, and increase vaccine coverage,” they wrote. “Moreover, respondents noted a generally positive attitude towards pharmacy-based vaccination and the removal of certain limitations and barriers.”
However, they added: “The expansion of pharmacists’ role in immunisation is encouraging, but not sufficient. Legislative and regulatory barriers must be overcome through evidence-based, quality advocacy, and they must address key issues, including reimbursement schemes. The framework for pharmacy-based vaccination, including vaccination records as well as training and certification, should be structured and harmonised. Collaboration with stakeholders, including governmental representatives and healthcare providers, should be maintained, in addition to patient education and awareness.
“As medicines experts, first-line healthcare providers and integral members of the healthcare team, pharmacists are valuable contributors to the health of their patients. Expanding pharmacists’ scope of practice as vaccinators will ultimately further their contributions to immunisation and to public health.”







