Integrating weight-loss injections into our healthcare system is a learning process, writes Fintan Moore
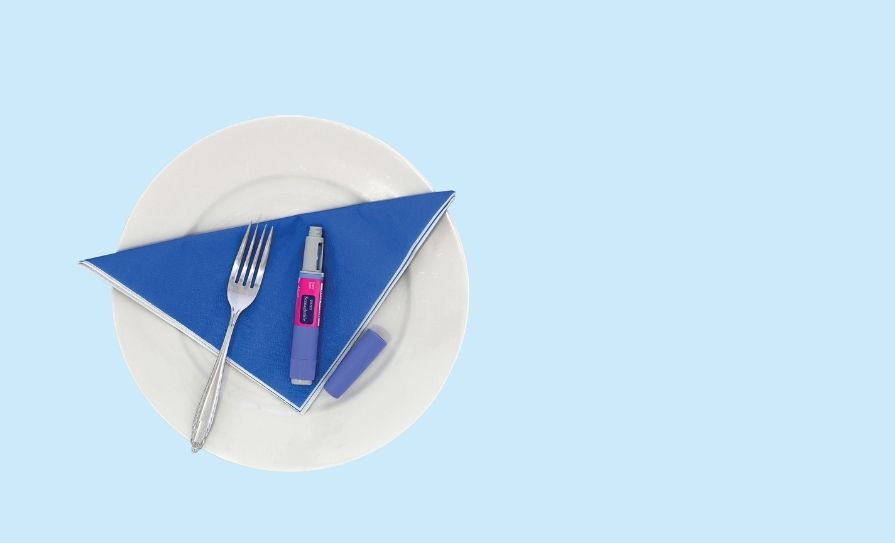
The use of weight-loss GLP- 1 injections has hit both medicine and society like a tsunami. From a standing start a few short years ago, the worldwide market is now worth over $50 billion and projected to break $100 billion by 2029.
In a world where so many people are suffering and dying from malnutrition, it can seem bizarre that so much money is spent on medication to tackle excess bodyweight — but obesity is a disease, and the GLP-1s are a genuine treatment option. However, because this class of drug is such a recent phenomenon, we are still at the stage of learning more about its long-term benefits and risks. One of the biggest unknowns is what happens when people use the
injections for several months with successful results, and then stop. A recent study published in the Journal of the American Medical Association (JAMA) had interesting findings.
The JAMA study involved more than 600 people who all used Mounjaro for 36 weeks as well as receiving advice about lifestyle, diet, and exercise. As expected, there were positive effects, with an average 20 per cent weight loss, and improvements in cholesterol, glucose control, and blood pressure.
After 36 weeks the group was split, with half still using Mounjaro and
half switched to a placebo. The diet and exercise support continued for both groups. Almost immediately the placebo group mostly started to regain weight and within a few months, a high percentage of those patients were approaching their starting weight.
In contrast, the Mounjaro patients continued to lose weight.
These findings indicate that (contrary to what had been hoped) using one of these medications as a short-term fix to ‘reset’ body weight and then staying at the new weight thanks to diet and exercise is not always a viable plan. Only about 20 per cent of the placebo group did not regain weight — these tended to be the patients who had lost the most weight, but there were no obvious ways to predict outcomes.
Another finding was that, on average, blood pressure rose again in almost all of the placebo group. Oddly, this occurred regardless of whether or not the person regained weight, although more regained weight tended to be linked with a higher increase in blood pressure. So, the one thing that is certain is that there’s still a lot to be learned.
Fake it until you make it
Healthmail may not be perfect and we’re probably still years away from a proper system of e-prescribing, but it’s certainly better than the completely antediluvian paper-based mess that we had for decades.
One of the fringe benefits of prescriptions arriving almost exclusively by Healthmail is that forged prescriptions are almost, but not quite, extinct. Back in the days before Covid and Healthmail, there were forgers who were very adept at creating fake prescriptions and finding suitably plausible people to present them at the counter without causing suspicion.
A good few years ago I spoke to a pharmacist who had a ‘home-help’ collecting benzodiazepines every month until he eventually smelled a rat and found out that she had a stolen prescription pad.
Another finding was that, on average, blood pressure rose again in almost all
of the placebo group
Forgeries are often a mess of mistakes with no hope of ever getting dispensed but at times, the most suspicious thing about a forgery is that the ‘doctor’ has actually written everything legibly and has a signature that looks like a name rather than a squiggle scrawled in Klingon.
Nowadays, hand-written prescriptions are so scarce that any written for a controlled drug (CD) immediately raise a flag, especially when brought in by a stranger. Irritatingly, they tend to deliberately land in at five minutes to closing-time in the hope that the pharmacist will dispense in a rush rather than look twice.
In reality, this doesn’t improve their odds and the enforced overtime just irritates the pharmacist even more. It’s often sad when computerisation causes the demise of a trade —
but when it comes to forging of prescriptions, I won’t complain.
Ryanpharm
Michael O’Leary isn’t everybody’s cup of tea, and a lot of people like to complain about Ryanair. Some of these same people gush about Aer Lingus and their ‘caring, friendly staff’, but I’m old enough to remember the days before Ryanair, when Aer Lingus used to charge £200 to fly one-way from Dublin to London.
Granted, there can be times when Ryanair staff may not be twinkly-eyed and fluffy, such as when enforcing baggage rules, but, overall, they do what they do cheaply and well. And there are also moments when I’d love to be able to take a leaf out of their book in the pharmacy. Imagine a world where every patient foible could be monetised with extra charges:
- Not ordering ahead for multi-item prescriptions, €50;
- Waiting rather than calling back after not ringing ahead, €75;
- Asking for ‘the usual’ then requesting extra items, €50;
- Same offence but taking items out, €50;
- Saying their doctor isn’t answering the phone when they haven’t even tried, €100;
- Tapping fingers on the counter while waiting, €125;
- Putting their €1.50 GMS levy on a slate while drinking a takeaway coffee, €150.
The list goes on…
Fintan Moore graduated as a pharmacist in 1990 from TCD and currently runs a pharmacy in Clondalkin. His email address is: greenparkpharmacy @gmail.com.